The middle cerebral artery (MCA) is one of the principal intracranial vessels. It is also the one that is most often involved in ischemic cerebrovascular disease, which accounts for a significant volume of brain imaging tests. With recent updates in the management of ischemic stroke (including intravascular treatment in increasingly distal vessels and in an increasingly widening spectrum of patients), it is becoming more important to know the details of the cerebral vascular anatomy to reach accurate diagnoses quickly and thereby improve patients’ prognoses. For these reasons, we present this anatomic review of the MCA, reviewing its segments and anatomic limits, its branching patterns, and its anatomic variants. We also provide a radiologic tool based on correlations between CT angiography and perfusion CT to facilitate the identification of the points of occlusion within the branches of the MCA, taking into account its different variants.
La arteria cerebral media es uno de los principales vasos intracraneales y el más implicado en la patología cerebrovascular isquémica, la cual constituye un importante volumen de nuestras exploraciones. Con las últimas actualizaciones en el manejo del ictus isquémico (que implican tratamiento intravascular sobre vasos cada vez más distales y en un espectro de pacientes cada vez más amplio) se hace más importante conocer al detalle la anatomía vascular cerebral, para poder establecer diagnósticos rápidos y certeros y mejorar así el pronóstico de los pacientes. Por ello, realizamos este repaso anatómico de la arteria cerebral media, revisando sus segmentos y límites anatómicos, sus patrones de ramificación y sus variantes anatómicas. A su vez, proporcionamos una herramienta radiológica basada en la correlación entre la angio-TC y la TC perfusión para facilitar la identificación de los puntos de oclusión dentro del árbol vascular de la arteria cerebral media teniendo en cuenta sus diferentes variantes.
The middle cerebral artery (MCA) is, along with the anterior cerebral artery, one of the terminal branches of the internal carotid artery. It is responsible for supplying blood to large parts of the cerebral hemispheres. Hence, it is the vessel seen to be affected in the majority of cerebral ischaemic events,1 which account for a great many radiological emergencies in our setting. In recent years, stroke management has been undergoing changes. The latest American Heart Association/American Stroke Association guidelines2 feature updates to the prior guidelines on endovascular treatment in stroke, including the use of mechanical thrombectomy up to the first 24h from the onset of symptoms in certain patients (those with large-vessel occlusions, mismatches on imaging tests [perfusion/diffusion] and certain clinical characteristics),3,4 and the use of endovascular techniques in occlusions up to the M3 segment of the MCA in particular patients.
All this requires radiologists to have clear and accurate knowledge of vascular anatomy, so that in an emergency situation, faced with the diagnosis of a cerebral ischaemic event, they can quickly and correctly determine the site of occlusion in the vascular tree, where a mechanical thrombectomy will likely be performed right away. With this, radiologists can help speed along the diagnosis and treatment pathway and optimise the patient's prognosis. Thus, in addition to a review of the anatomy of the MCA with its possible anatomical variants and abnormalities, we present a radiological tool based on correlating perfusion and computed tomography (CT) angiography to facilitate determination of the location of obstruction in the affected branch in the diagnosis of a cerebral ischaemic event.
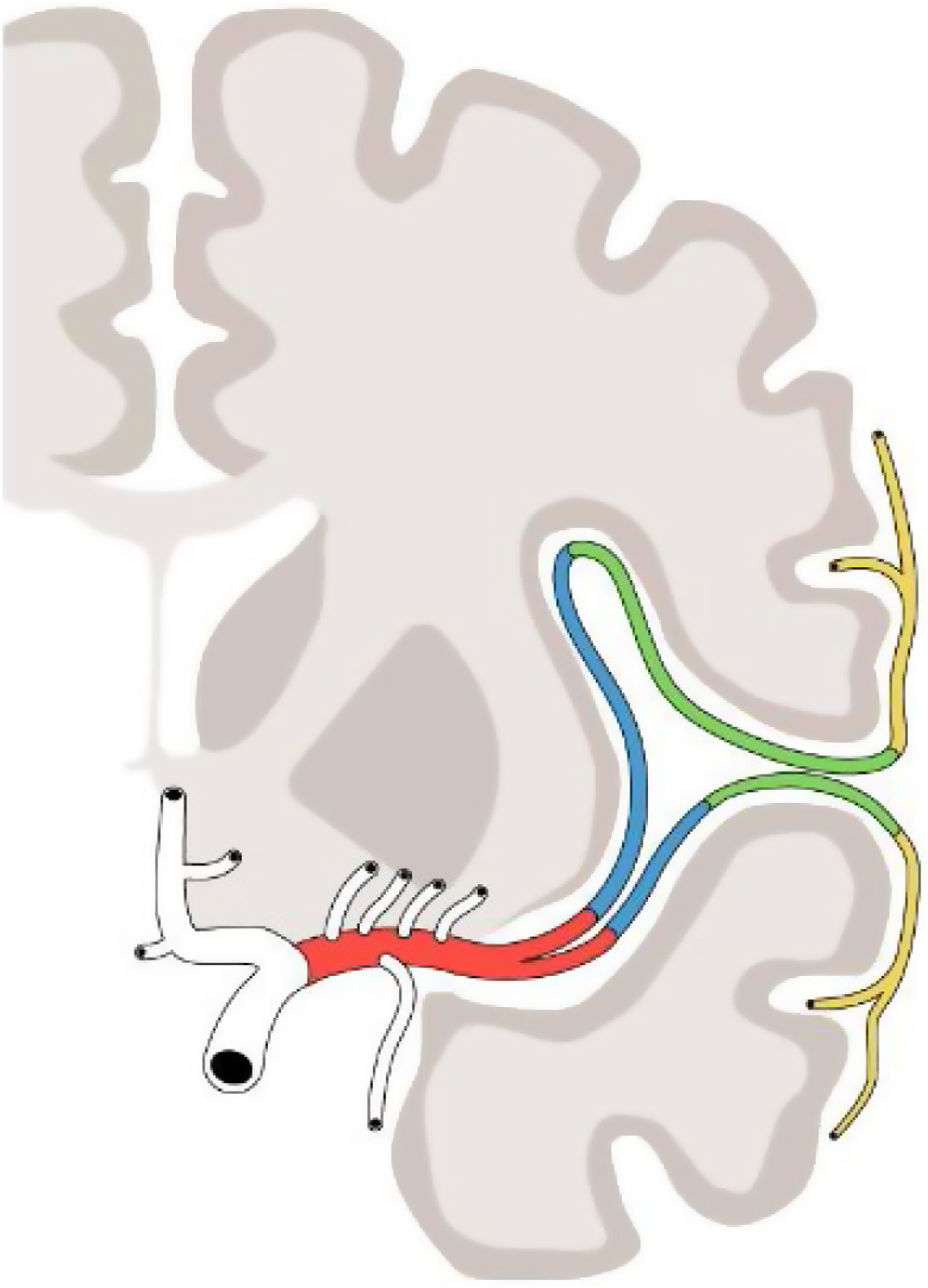
MCA: segmentsClassic anatomical terminology establishes two MCA segments (M1 and M2) delimited by the bifurcation of the main trunk.5 In practice, however, for the surgical and radiological approach, four segments are distinguished (M1, M2, M3 and M4), described in the early 1980s by Gibo et al.6 and determined by the spatial distribution of the main trunk and successive branches (Fig. 1):
- •
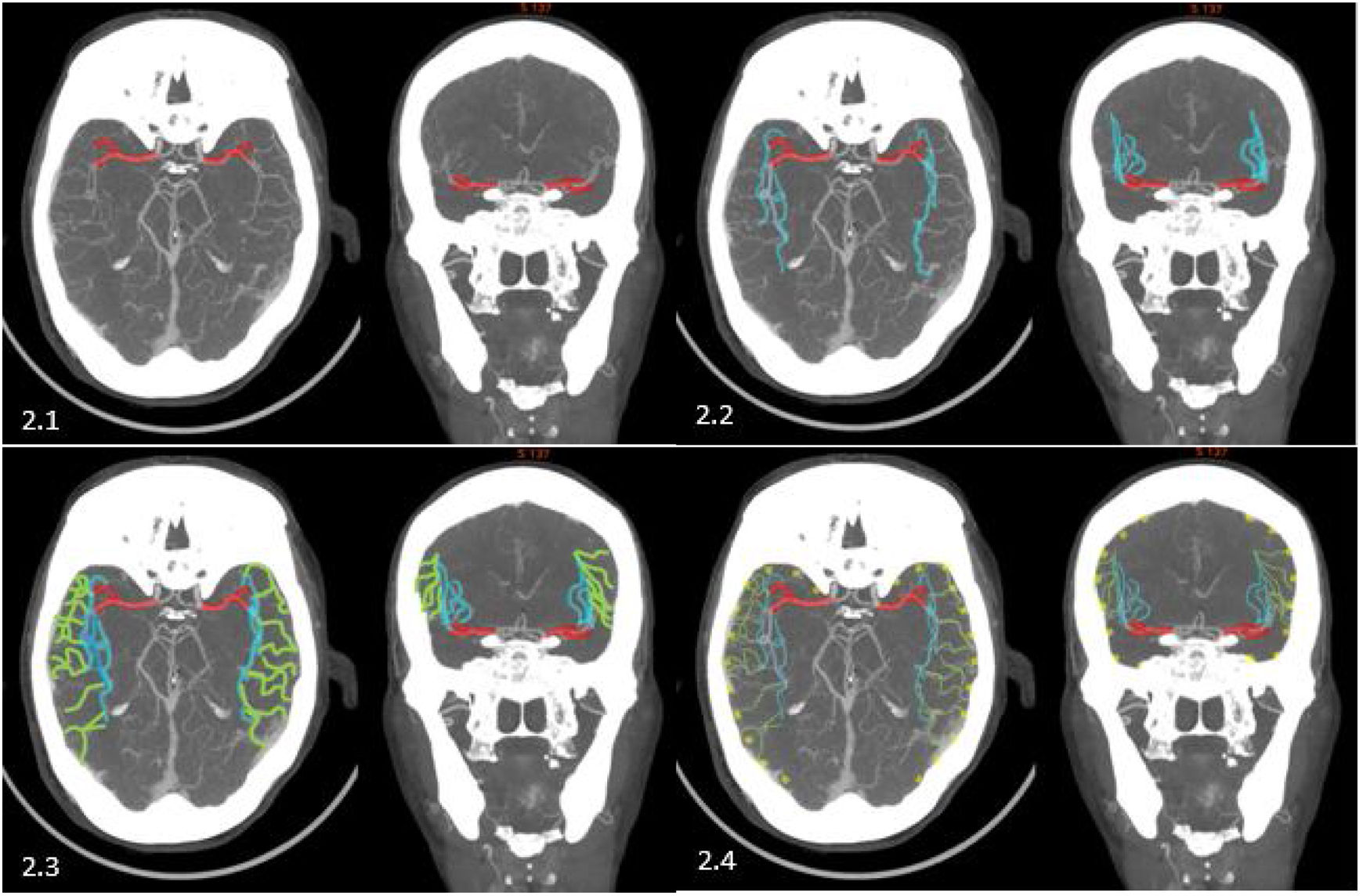
M1: horizontal or sphenoidal segment. This originates at the bifurcation of the internal carotid artery and runs laterally on an axial plane, under the anterior perforated substance and parallel to the sphenoid wing, towards the Sylvian fissure. Its trajectory it can be divided into two or more trunks, such that there are two parts to the M1: the pre-bifurcation M1 segment and the post-bifurcation M1 segment (made up of the horizontal segments of each of the two or more corresponding trunks in each case). When the post-bifurcation segment trunks reach the limen insulae, they make a 90-degree turn known as the genu, terminating the M1 segment (Fig. 2.1).
- •
M2: insular segment. This originates at the genu of the main trunks of the MCA and is comprised of these and their successive branches which circulate on the insulae, along the Sylvian fissure, on a vertical plane towards the most distal part of the insular circular sulcus. Here, they make another, sharper turn, forking to surround the opercula, where the M3 segment begins (Fig. 2.2).
- •
M3: opercular segments: from the most distal part of the circular sulcus, the branches run along the frontoparietal and temporal opercula towards the most lateral/superficial edge of the Sylvian fissure, where the M4 segments begin (Fig. 2.3).
- •
M4: cortical segments. From the lateral/superficial edge of the Sylvian fissure, the branches turn again, moving away from the edge and running in a superior or inferior direction on the cortical surface until terminating; these constitute the M4 segments (Fig. 2.4).
The MCA has two groups of branches: the perforating or lenticulostriate arteries and the cortical arteries.7
The perforating arteries are very low-calibre vessels that emerge in variable numbers, between eight and 20; most of them run along the M1 segment of the MCA and some of them also run from the anterior cerebral artery. Their limited calibre makes it difficult to fully identify them on angiography. These branches run superiorly through the anterior perforated substance to supply blood to the basal ganglia and deep structures of the brain. They are divided into a medial group and a lateral group, depending on whether they form before or after the division of the main trunk of the MCA. The medial group primarily supply the lentiform nucleus, part of the caudate nucleus and internal capsule; the lateral group ascend in a more superior direction to supply the external capsule and the caudate nucleus.8
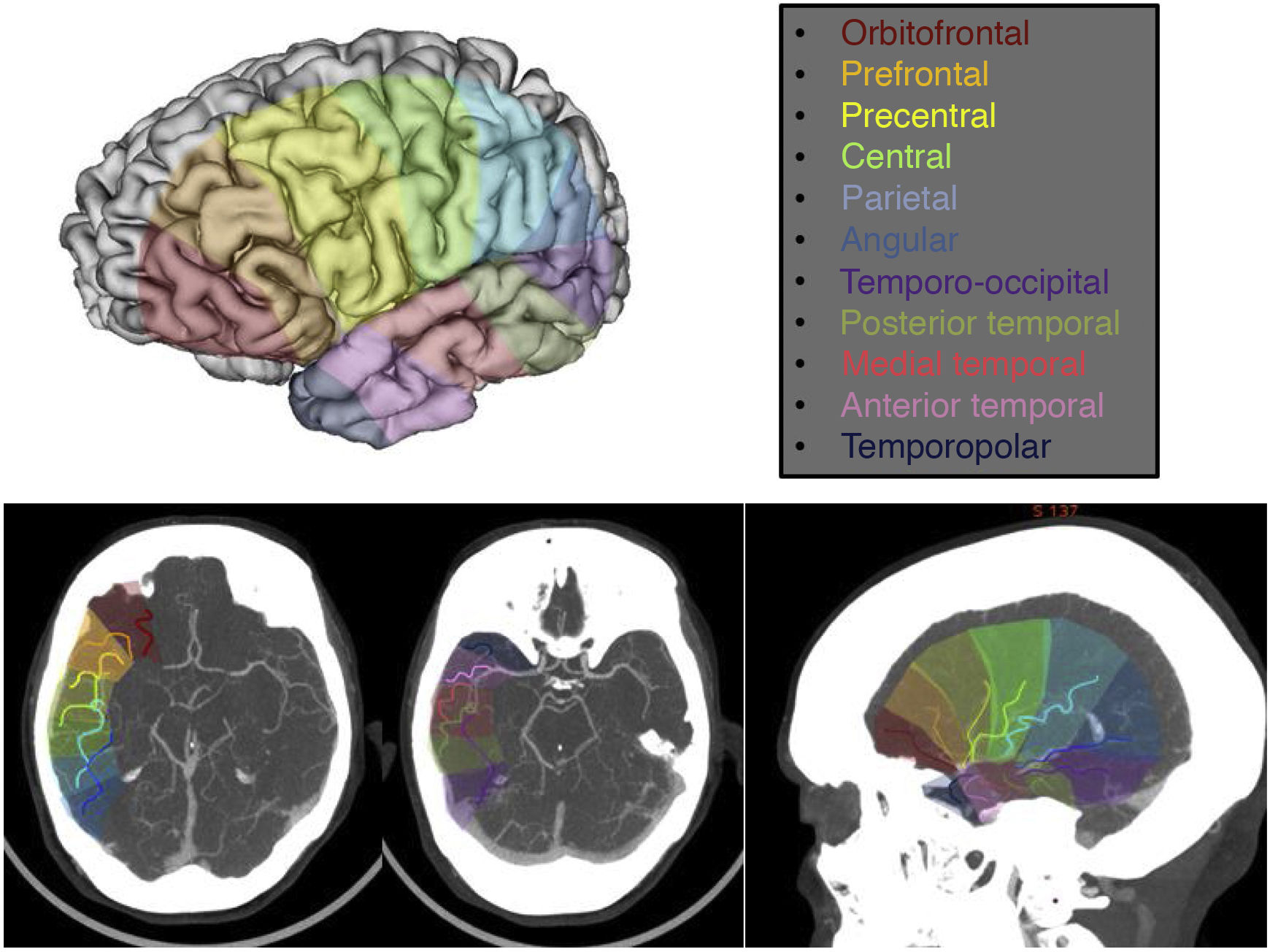
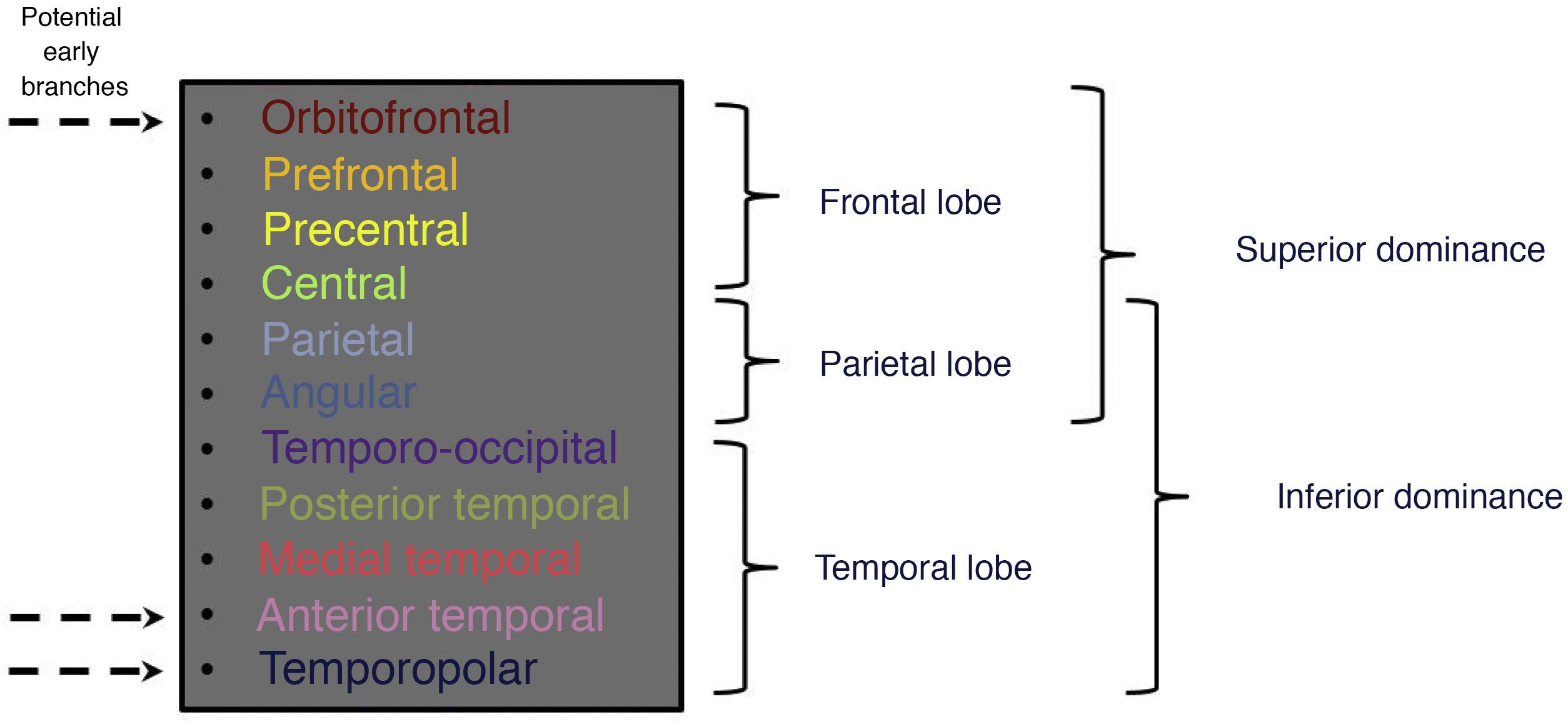
The cortical arteries are the branches that emerge along the MCA to supply the different cortical regions with blood. These are vessels of a considerably larger calibre, allowing them to be properly independently assessed using regular angiographic imaging techniques. The number of these branches also varies, and their pattern of emergence from the MCA is variable too, giving rise to wide anatomical variation. It is normal to have 10–12 cortical branches. The most common are the following: orbitofrontal, prefrontal, precentral, central, anterior parietal, posterior parietal, angular, temporopolar, anterior temporal, medial temporal, posterior temporal and temporo-occipital6 (Fig. 3).
Three-dimensional image of the brain with the regions of blood supply corresponding to each cortical branch and representation of the spatial/anatomical arrangement of the different cortical branches in axial and sagittal CT slices with their corresponding regions of blood supply.
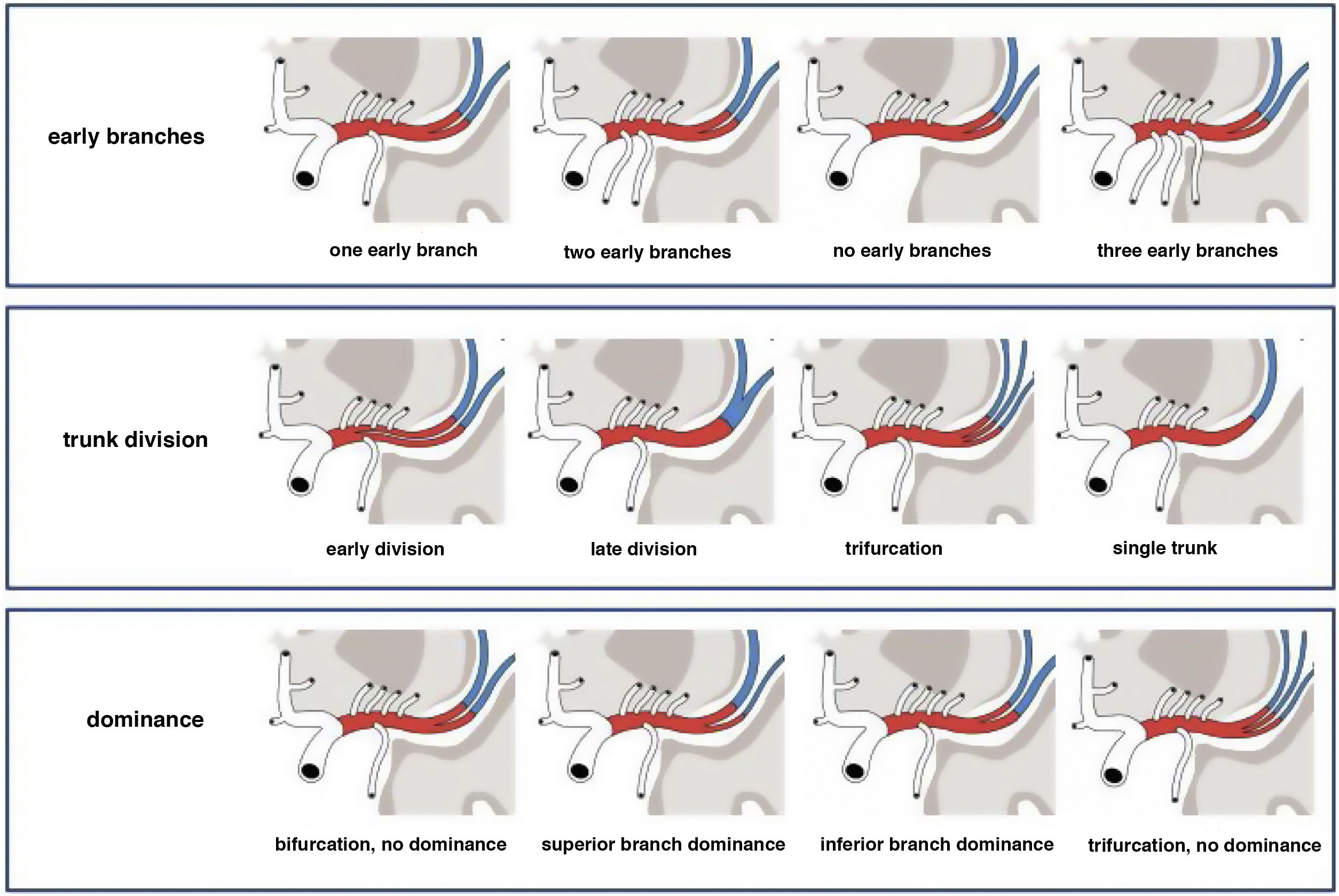
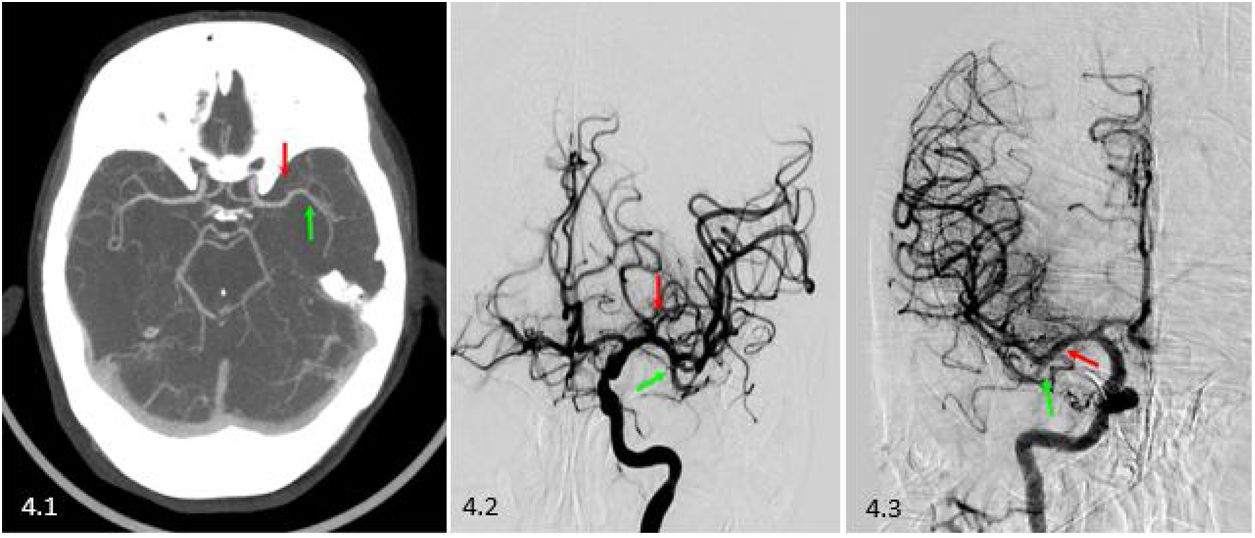
The variability of the branching patterns is determined by three main factors: the presence of early branches, the division of the main trunk of the MCA and the dominance of the trunks6 (Fig. 4).
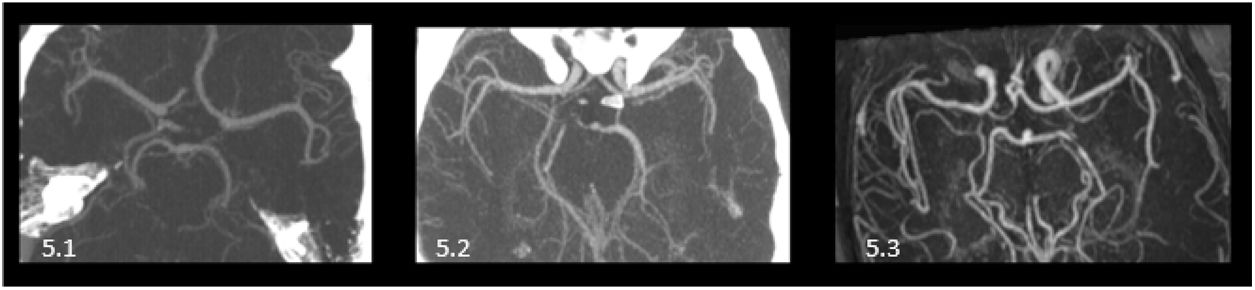
Early branchesThe majority of the cortical branches emerge from the MCA once their main trunk has divided, along those divisions or from other cortical branches. However, it is also possible for cortical branches to form prior to that division, emerging from the pre-bifurcation M1 segment; these are so-called early branches. These early branches may be temporal or frontal, with the temporopolar, anterior temporal or orbitofrontal arteries appearing as such. The most typical variant is the presence of one of these early branches, generally an early temporal branch.9 The next most typical variants are, in order of frequency: having two early branches; then having none; then, finally and less commonly, having three of these early branches10 (Fig. 5).
Division of the main trunkThe main trunk of the MCA is divided into smaller trunks, generally along its M1 segment. The location of this division gives rise to variants. An early division corresponds to one that occurs very close to the formation of the MCA, with a very short pre-bifurcation segment (generally, less than 5mm). A late division corresponds to a division seen to be proximal to the M2 segment.
Division itself may vary as well. Most commonly, the main trunk divides into two trunks—that is to say, it bifurcates (in around 70% of cases) to form an anterosuperior trunk and a posteroinferior trunk.11,12
The next most common case would be trifurcation (in approximately 20% of cases), with the formation of a superior trunk, an intermediate trunk and an inferior trunk.11,12
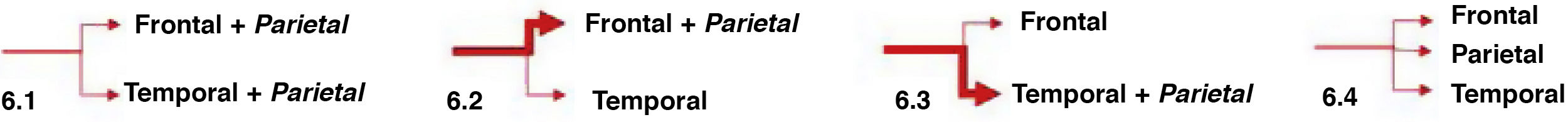
The medical literature also features reports of less common possibilities, such as division into multiple trunks or even no divisions at all, with a single MCA trunk (each in less than 10% of cases)12,13 (Fig. 6).
Dominance of the divisionsThe dominance of a division is determined by its supplying blood to a larger region of the brain, which in turn is determined by its having a larger number of cortical branches emerging from it. Amounting to the same, some cortical branches form in one division or another depending on dominance.
In the most typical case, bifurcation, the temporal branches form in the inferior division and the frontal branches form in the superior division. The parietal branches, for their part, may emerge from the superior trunk, the inferior trunk or some combination of both; this is determined by dominance of the anterosuperior division in the first case, dominance of the posteroinferior division in the second or no dominance in the third.6
In the case of trifurcation, in general, the temporal branches form from the inferior division, the parietal branches from the middle division and the frontal branches from the superior division. If any division shows itself to be dominant, this means that from it will emerge in addition a branch of an adjacent region that does not form in its corresponding division11 (Figs. 7 and 8).
Diagram of the most common cases with respect to dominance of the divisions of the MCA, with the region of blood supply corresponding to each division. 6.1) No dominance (the branches that supply blood to the parietal lobe arise from the two divisions). 6.2) Anterosuperior dominance (the blood supply to the parietal lobe comes from the anterosuperior branch, along with the blood supply to the frontal lobe). 6.3) Posteroinferior dominance (the blood supply to the parietal lobe comes from the posteroinferior branch, along with the blood supply to the temporal lobe). 6.4) Trifurcation with no dominance (each lobe is supplied with blood by one of the three divisions).
Abnormalities of the MCA are less common than abnormalities in other large intracranial arteries. They are due to abnormal fusion of primitive vascular networks. The following are considered as such: an accessory MCA, MCA duplication and, much less commonly, a duplicated MCA origin and MCA fenestration.13
An accessory MCA refers to the formation of an additional trunk parallel to the main MCA with an origin distal to it, from the anterior cerebral artery. It supplies blood to the anterior portion of the frontal lobe. MCA duplication corresponds to the formation of a trunk in addition to the main MCA but proximal to it, with both emerging from the internal carotid artery. It supplies blood to the anterior portion of the temporal lobe.14
A duplicated MCA origin is considered to be present when the proximal portion of an accessory MCA or a duplicated MCA persists and fuses distally with the main MCA. MCA fenestration is the name given to a fusion defect in the main trunk of the MCA after its origin, such that it emerges as a single trunk, branches and then re-fuses.15
Anatomical/radiological tool based on CT angiography and CT perfusionIn clinical practice, CT perfusion can be leveraged to quickly locate the affected branch in a cerebral infarction if it is not possible to locate it on CT angiography.16 This technique identifies the areas of the parenchyma that have been affected in an ischaemic event. Thus, if practitioners know the anatomy of the MCA with its branches and the corresponding regions to which they supply blood, by observing the ischaemic parenchyma on CT perfusion of a particular case, they will be able to sense which branch or branches have been affected. If they know the anatomical variants of the MCA, they can extrapolate the possible points of obstruction amongst the different MCA vascular tree possibilities and confirm which will be obstructed in that case on CT angiography.17 The associated figures show real-world applied cases (Figs. 9 and 10).
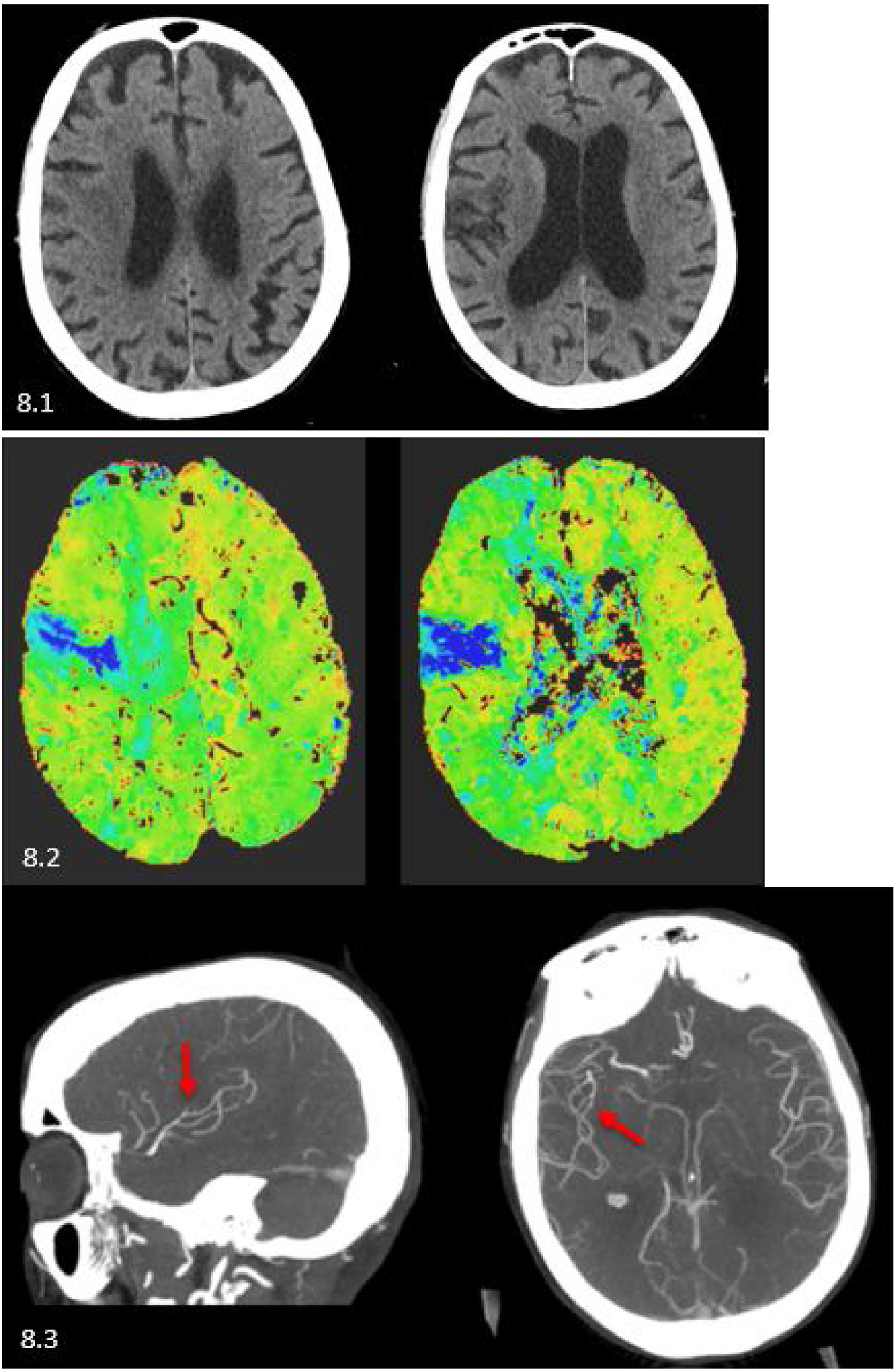
Case 1: an 87-year-old man with a right partial anterior circulation infarction (PACI). 8.1) Baseline CT with hypodensity in left M2 and M5 areas, Alberta stroke programme early CT score (ASPECTS) 8. 8.2) CT perfusion (Tmax map) with time delay in the corticosubcortical area corresponding to left precentral branch. 8.3) CT angiography in axial and sagittal slices: opacification is seen to stop at the left precentral branch (red arrow).
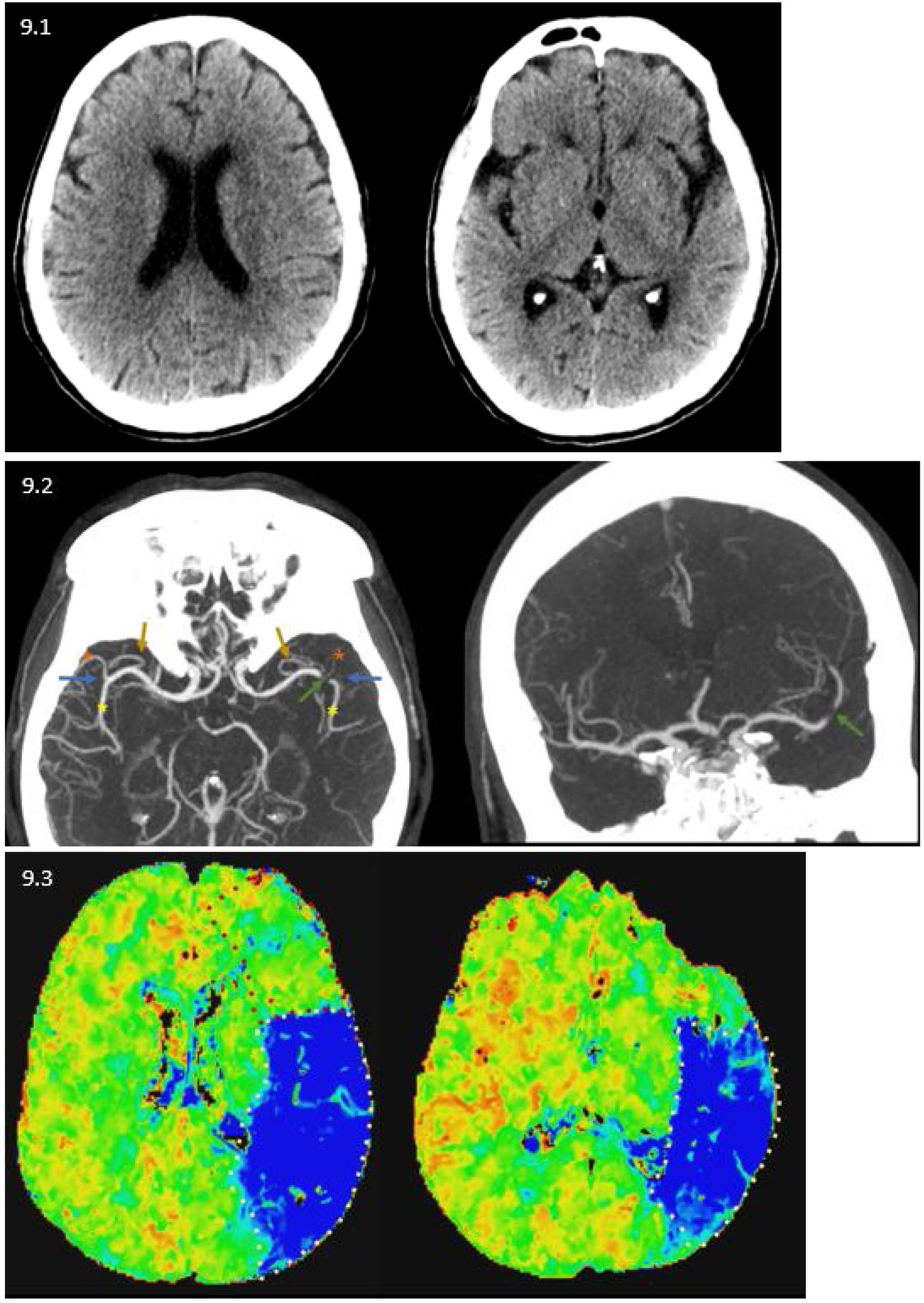
Case 2: a 69-year-old man with a left total anterior circulation infarction (TACI). 9.1) Baseline CT with no abnormalities, ASPECTS 10. 9.2) CT angiography showing bifurcation of the trunks of both MCAs (blue arrows) with their anteroinferior (red asterisk) and posterosuperior divisions (yellow asterisk) and revealing dominance on the part of the latter given its larger calibre compared to the former. Both MCAs, for their parts, have early branches (brown arrows). A filling defect is seen around the bifurcation of the left MCA (green arrow). 9.3) CT perfusion (Tmax map), time delay in parietal, medial temporal and posterior temporal regions, indicating that only the dominant (posteroinferior) division of the left MCA has been affected.
To conclude, we would like to note that endovascular treatment of ischaemic stroke is becoming possible in more and more distal branches. This means that radiologists in emergency settings must possess detailed knowledge of cerebral vascular anatomy so that they may quickly and accurately identify the occluded branch. With this, they not only aid in making a correct diagnosis but also facilitate treatment planning.
Authorship- 1
Responsible for study integrity: SMM, MPP.
- 2
Study concept: SMM, MPP
- 3
Study design: SMM, MPP
- 4
Data collection: SMM, MPP.
- 5
Data analysis and interpretation: SMM, MPP.
- 6
Statistical processing:
- 7
Literature search:
- 8
Drafting of the article: SMM, MPP
- 9
Critical review of the manuscript with intellectually significant contributions: SMM, MPP, SGO, JCF.
- 10
Approval of the final version: SMM, MPP, SGO, JCF.
A review of the anatomy of the middle cerebral artery for the era of thrombectomy: a radiologic tool based on CT angiography and perfusion CT
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Medrano-Martorell S, Pumar-Pérez M, González-Ortiz S, Capellades-Font J. Repaso anatómico de la arteria cerebral media en la era de la trombectomía: una herramienta radiológica basada en la angio-TC y la TC perfusión. Radiología. 2021;63:505–511.