Alveolar adenoma is a rare lung neoplasm initially described by Yousem and Hochholzer in 19861. In most cases, they are described incidentally in radiological studies on middle-aged, asymptomatic women2. Although their course is benign, surgical resection and histological study are required for the definitive diagnosis.
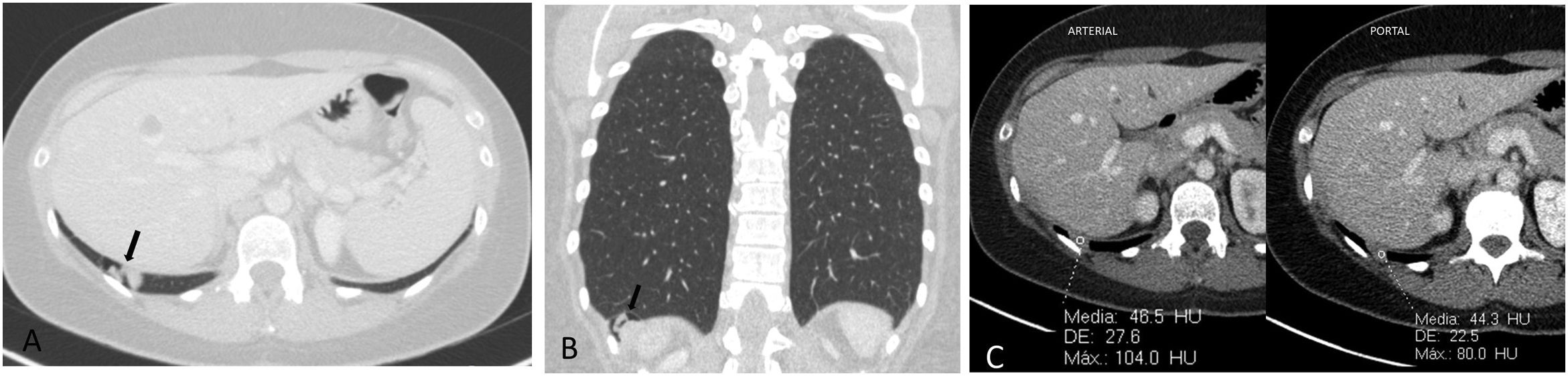
We present the case of a 48-year-old woman with a history of pneumonia associated with environmental dust, treated with antibiotics and bronchodilators. During the investigations related to this episode, a computed tomography (CT) scan conducted after the administration of intravenous contrast (IVC) (Fig. 1) identified a nodular formation in the posterior segment of her right lower lobe (RLL), 30×12mm in size. It had an aerial component and a lobulated soft tissue density component (Fig. 1A and B), with mean attenuation values of around 45 Hounsfield units (HU) and no significant variations between the arterial and portal phases (Fig. 1C).
Computed tomography with intravenous contrast. Lung parenchyma window in axial (A) and coronal (B) planes. In the posterior segment of the right lower lobe, a nodular formation can be seen with components of both lobulated and aerial soft tissue density (black arrow). Mediastinal window in the axial plane (C), where the attenuation values of the soft tissue component in the arterial (left) and portal phase (right) are compared, showing that there is no significant variation in the density of the lesion.
As this was an indeterminate pulmonary nodule not accessible to transthoracic biopsy, an atypical segmental resection of the RLL was performed using video-assisted thoracoscopic surgery. There were no complications in the immediate postoperative period. The CT scan performed six months after surgery showed no radiological data of recurrence.
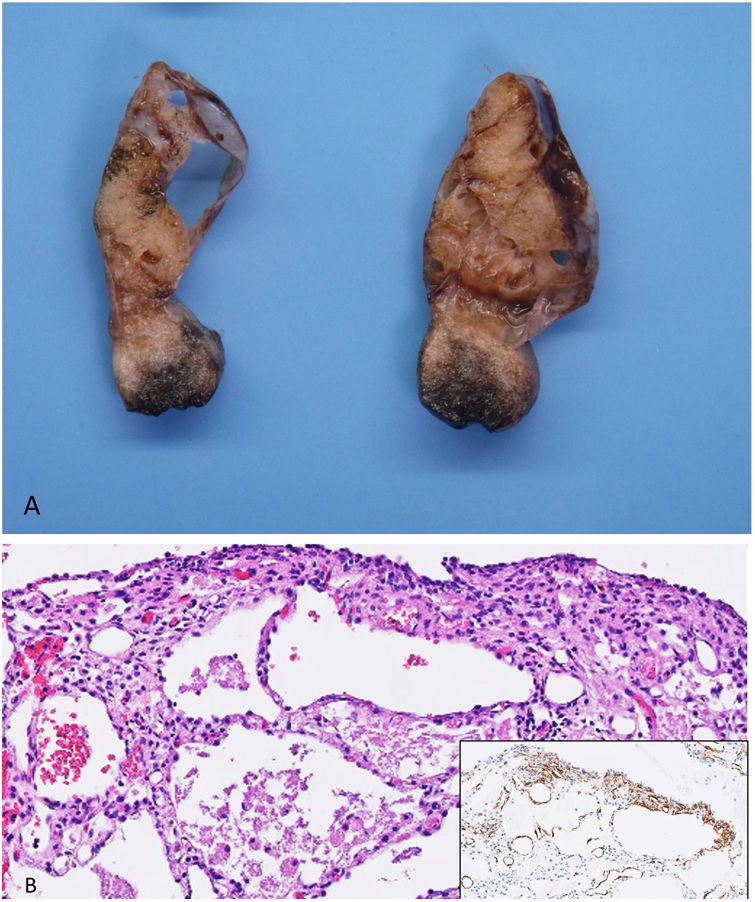
The macroscopic examination of the surgical specimen found a well-defined polypoid subpleural mass with a maximum diameter of about 3cm (Fig. 2A), comprised of multiple cystic cavities filled with a dense gelatinous material.
A) Macroscopic examination reveals a well-defined subpleural lesion of the adjacent lung parenchyma, consisting of multiple cystic cavities filled with a dense gelatinous material. Section stained with HE (100×) B). Cystic cavities filled with dense eosinophilic extracellular material with histiocytes. Immunohistochemistry reveals smooth muscle actin-positive cells within the septa (box with asterisk).
Histopathological examination (Fig. 2B) identified it as a cystic tumour, made up of cavities lined by cuboidal epithelial cells without atypia. The cavities were separated by connective tissue septa, consisting of mesenchymal cells arranged in a fibromyxoid matrix. Inside the cysts was an eosinophilic protein material with histiocytes. In the immunohistochemical analysis, the epithelial cells were positive for TTF-1, pan-CK and napsin, and the mesenchymal cells focally expressed smooth muscle actin.
The lack of an invasive growth pattern and atypia are helpful in the differential diagnosis of adenocarcinoma. It can be distinguished from a lymphangioma by the fact that the cells lining the cystic cavities are positive for epithelial markers and negative for endothelial markers. Stromal cells negative for TTF-1 rule out a cystic pneumocytoma. These factors then lead to the diagnosis of alveolar adenoma.
From a radiological standpoint, alveolar adenomas appear as subpleural nodules with well-defined borders, with a mean diameter of 2.2cm, relatively low attenuation values (around 25 HU) and no enhancement after administration of IVC3. The lack of enhancement is an important factor in the differential diagnosis with pneumocytoma, which also presents as a subpleural nodule in middle-aged women, but which does usually show marked enhancement4. Although one case in the literature had punctiform enhancement areas inside the nodule, this finding was related to the presence of stromal vessels in the interstitium4. There is also a report of a multiseptate, cavitated mass with well-defined borders5. However, we found no imaging descriptions like that of our patient, associating both soft tissue density and air cystic components, and we believe that the interest of our case lies in this distinctive feature.
Lesions studied with positron emission tomography did not show significant avidity for 18FDG2 and the few cases assessed with magnetic resonance imaging3 showed a behaviour consistent with a cystic lesion (signal hypointensity in T1-weighted sequences and marked hyperintensity in T2-weighted sequences), with wall ring enhancement after gadolinium administration.
In conclusion, alveolar adenoma is a rare neoplasm, but one that should be included in the differential diagnosis of incidental pulmonary nodules, especially in middle-aged women. Radiologically, they can be both homogeneous lesions and mixed lesions (as in our case) with a soft tissue and air component. After reviewing the histology of our case, we believe that the dense eosinophilic proteinaceous alveolar content may correspond to the soft tissue density reported in the radiological examination.
FundingThe authors declare that they have not received any type of funding.
Conflicts of interestThe authors declare that they have no conflicts of interest.