Cervical spine trauma encompasses a wide of injuries, ranging from stable, minor lesions to unstable, complex lesions that can lead to neurologic sequelae or vascular involvement.
The Canadian C-Spine Rule and the NEXUS criteria aim to identify individuals with a low risk of cervical spine trauma who can safely forgo imaging tests. In high-risk patients, an imaging test is indicated. In adult patients the imaging test of choice is multidetector computed tomography. Complementary imaging tests such as CT angiography of the supra-aortic vessels and/or magnetic resonance imaging are occasionally necessary.
It can be challenging for radiologists to diagnose and classify these lesions, because some of them can be subtle and difficult to detect. This paper aims to describe the most important imaging findings and the most widely used classification systems.
Las consecuencias de un traumatismo de columna cervical pueden variar desde lesiones menores estables hasta lesiones complejas e inestables con posibles secuelas neurológicas o afectación vascular.
Los criterios canadienses (Canadian C-Spine Rule) y los criterios NEXUS tratan de identificar a aquellos individuos con bajo riesgo de presentar lesiones por traumatismo cervical y en quienes se puede prescindir con seguridad de la exploración radiológica. En pacientes con alto riesgo, está indicada una prueba de imagen, siendo la técnica de elección, en adultos, la tomografía computarizada multidectector. En ocasiones son necesarios estudios complementarios como angio-TC de troncos supraaórticos o la resonancia magnética.
Diagnosticar y clasificar estas lesiones pueden ser un desafío para el radiólogo, ya que algunas de ellas pueden ser sutiles y difíciles de detectar. Este trabajo tiene como objetivo describir los hallazgos radiológicos más relevantes y las clasificaciones más utilizadas.
Cervical spine injuries occur in 5–10% of multiple trauma patients. Although the incidence is not high, they account for more than half of spinal cord injuries, causing both significant neurological impairment and emotional impact.1 The subaxial region accounts for 65% of cervical spine fractures, due to its greater mobility and proximity to the rigidity of the thoracic spine.2 However, craniocervical junction fractures are associated with higher morbidity and mortality rates and risk of vascular lesions.
There is a notably higher prevalence in the young population, as the main causes are road traffic accidents, with falls, assaults and sports injuries also common.2 In older adults with spondylitis, they should be suspected even after low-energy trauma. In children, there is a greater risk of atlantoaxial dislocations in the absence of fracture.1
These injuries are increasingly detected due to the optimisation of diagnostic imaging tests, with the implementation of comprehensive protocols for multiple trauma patients in Accident and Emergency departments (A&E).
The aim of this study is to review the indications and the type of radiological examination appropriate for cervical trauma, the systems in place for reading the images, and the main radiological findings, in order to highlight the most common classifications and the associated vascular complications.
Imaging tests in cervical spine traumaThe radiologist plays a key role in the early diagnosis of traumatic cervical spine injuries, which enables appropriate therapeutic management to be put in place and helps avoid permanent neurological and cerebrovascular damage and deformity.3,4
Conventional X-rays miss 20–57% of cervical spine fractures.3,4 Nevertheless, they continue to be widely used in A&E, despite their indications not being clearly defined. There are clinical guidelines that recommend computed tomography (CT) only if cervical X-rays show abnormalities or if the patient’s level of consciousness is affected, and there is consensus on obtaining at least three views: anteroposterior, lateral and odontoid.3
Since 2008, and with a review in 2019, the American College of Radiology has rated CT as the diagnostic technique of choice in patients over 15 years of age with cervical spine trauma, and magnetic resonance imaging (MRI) when neurological or discoligamentous injury is suspected.3,5,6
There is some consensus in not recommending MRI systematically if the cervical spine CT reveals nothing, as the rate of CT scan false negatives according to the literature ranges from 0.3% to 5.2%, and the estimated incidence of ligament injuries detected on MRI in these cases is very low and without therapeutic implications.4,6,7
The National Emergency X-Radiography Utilization Study (NEXUS) criteria and the Canadian Cervical Spine Rule are clinical guidelines used to select patients who do not require imaging tests after cervical spine trauma.3 With a specificity of 45.1%, the Canadian Cervical Spine Rule is more effective in avoiding unnecessary imaging tests.6 These criteria are not applicable to people over 65 years of age or with rigid spines (cervical spondyloarthritis, ankylosing spondylitis, Forestier disease and spinal arthrodesis), because they tend to suffer severe neck injuries from low-energy trauma, making a cervical spine CT necessary (Table 1). In patients over 15 years of age with cervical spine trauma and intermediate-to-high-risk clinical criteria, CT is the method of choice.
NEXUS criteria and Canadian Cervical Spine Rule.
| NEXUS criteria |
|---|
| Do not perform imaging tests if all of the following criteria are met: |
| 1) No midline spinal tenderness |
| 2) No focal neurological deficit |
| 3) No altered level of consciousness |
| 4) Not intoxicated |
| 5) No distracting injury |
| Canadian Cervical Spine Rule |
|---|
| Do not perform imaging tests if the patient is alert with a Glasgow Coma Scale score of 15 and all of the following criteria are met: |
| 1) No high risk factors are identified |
| - Age 65 years or over |
| - Paraesthesia in extremities |
| - Mechanism of the accident: fall from height of more than 3m/5 steps, axial load to the head, high-speed collision between vehicles, bicycle crash |
| 2) Presence of any low-risk factors |
| - Rear-end collision between vehicles excluding head-on collision, hit by bus/truck, rollover and hit by high-speed vehicle |
| - Sitting position in A&E |
| - Ambulatory at any time |
| - Delayed onset of neck pain |
| - No midline spinal tenderness |
| 3) Able to rotate neck 45° to the left and the right |
The Canadian Cervical Spine Rule asks three questions: (1) Are there high-risk factors?; (2) Are there any low-risk factors; and (3) Is the patient able to rotate their neck 45º? If the answer is "NO" to the first question and "YES" to the last two and the patient has a normal level of consciousness (15 points on the Glasgow Coma Scale), radiographic studies are not necessary and cervical spine injury can be ruled out clinically (3). These criteria are not applicable in people over 65 years of age or with rigid spines (cervical spondyloarthritis, ankylosing spondylitis, Forestier disease and spinal columns with arthrodesis).
On cervical spine CT, bone and soft tissue reconstruction should be obtained in orthogonal planes with a slice thickness of less than 2mm.
System for readingFollowing a system for reading is recommended in order to avoid missing injuries that are not very evident8; the images are displayed schematically and examination is made of the ligamentous structures of the cervical spine (Figs. 1 and 2).
System for reading images. Normal CT of cervical spine, bone window. (A) Sagittal reconstruction, midline. Anterior vertebral (line 1), posterior vertebral (line 2) and spinolaminar (line 3) lines. Basion-dens interval (line 4). Basion-posterior axial line interval (line 5). Atlanto-dens interval (line 6). C1-C2 spinolaminar distance (line 7). (B) Left parasagittal reconstruction. Joint congruency between the occipital condyle (OC) and the condylar fossa of C1 (lines 8). Correct alignment of the facet joints (arrows 9). (C) Coronal reconstruction. Atlanto-occipital (lines 1) and atlantoaxial (lines 2) joints. Relationship dens-lateral masses of the atlas (line 3). Relationship of the lateral masses of the atlas with the axis (line 4). (D) Axial C1 reconstruction. Diameter of the spinal canal (crossed lines). Left transverse foramen (arrow). (E) Axial reconstruction, C3-C4 facet joint (circle), joint space (line).
Anatomy of the cervical spine ligaments. Magnetic resonance imaging of the cervical spine with T2-weighted sequences (TSE), 3-mm slices, sagittal (A), axial (B) and coronal (C and D) planes. Anterior longitudinal ligament (ALL) is continuous with the anterior atlanto-occipital membrane. Posterior longitudinal ligament (PLL) is continuous with the tectorial membrane. Yellow ligament (Lig.) is continuous with the posterior atlanto-occipital membrane. Interspinous and supraspinous ligaments are continuous with the nuchal ligament. Cruciform ligament (CL): made up of horizontal and other vertical fibres (crossed). Its horizontal component is called the transverse ligament, which is inserted into the lateral tubercles of C1, passing behind the dens; it is one of the main stabilisers in the region. The vertical component (superior extension) of the CL is formed by fibres that extend from the clivus to the posterior aspect of the dens. Alar ligaments: two structures that extend from the dens towards the most internal sector of the occipital condyles. Apical ligament: a thin structure that extends from the tip of the dens to the basion of the skull.
The diagnostic approach to craniocervical junction trauma has advanced in recent years, with classifications changing over time. The most commonly used by anatomical region are described below.
In 2018, AO Spine proposed a new classification system for craniocervical junction injuries, similar to those for subaxial, thoracolumbar and sacral injuries, which uses morphological patterns of injuries combined with clinical factors, and whose use is becoming more and more widespread.9,10
Craniocervical dissociationSeparation of the occipital relative to C1-C2; the term ranges from complete dissociation to subluxations, and is usually associated with high-energy trauma, due to a distraction mechanism combined with flexion or extension. It is more common in children and is considered to be an unstable injury with ligamentous rupture (tectorial membrane and alar ligaments). In most cases it is life-threatening, as it can cause spinal cord injury and injury to the cranial nerves and vertebral arteries. Subluxations can be subtle and less often fatal.11
According to Traynelis et al.,12 they are classified as:
–Type I: more common. Anterior displacement of the condyles.
–Type II: more unstable. Separation in the longitudinal plane.
–Type III: posterior displacement of the condyles.
Radiological findings (Fig. 3A and B)11,13:
–Articular incongruity between the occipital condyles and the condylar fossae of C1.
–Increased joint distance between the occipital condyles and the lateral masses of the atlas: greater than 2mm or the sum greater than 4mm.
–Basion-dens interval: greater than 10mm.
–Basion-posterior axial line interval: greater than 12mm.
CT of cervical spine, bone window. (A–C) 40 year-old male, road-traffic accident. Atlanto-occipital dislocation with anterior displacement of the skull (Traynelis classification type I). (A) Sagittal reconstruction, midline. Increased basion-dens intervals greater than 10mm (solid line) and basion-posterior axial line greater than 12mm (2-pointed arrow), posterior axial line (dashed line). (B) Left parasagittal reconstruction. Joint incongruity between the condylar fossa of C1 and the occipital condyle (OC) showing anterior displacement (arrow). (C) Coronal reconstruction. Avulsion fracture of the right occipital condyle (Anderson and Montesano classification type III) (arrowhead), with a displaced fragment invading the foramen magnum (thick arrow). D-F) 77-year-old male, fall from standing height. Jefferson fracture. (D) Axial slice. Bilateral fracture of the anterior arch of the atlas and left posterior arch (arrows) (type III of the Jefferson classification adapted by Gehweiler). (E) Left parasagittal reconstruction. Posterior joint subluxation of C1-C2 (arrow). (F) Coronal reconstruction. Associated fracture of the dens (Anderson and D'Alonzo classification type II) (arrows).
Fractures of the occipital condyles occur in 3% of patients with severe blunt neck trauma.3 They indicate a high-energy mechanism and are usually associated with other craniocervical fractures and injuries to the vertebral and carotid arteries or lower cranial nerves. There are three types according to the Anderson and Montesano classification14:
- −
Type I: comminuted fracture without/with minimal displacement, due to axial overload.
- −
Type II: fracture at the base of the skull extending to the occipital condyle, due to direct trauma.
- −
Type III (most common): avulsion fracture of the alar ligament insertion, due to hyperflexion and lateral rotation (Fig. 3C).
Type I and II injuries are usually stable, with preservation of the alar ligaments. Type III fractures are unstable, the alar ligament is torn or is functionally incompetent due to the avulsion. It is important to measure the displacement of the condyle fragments and determine whether or not they are lodged in the foramen magnum.15 With CT it can be difficult to differentiate between types I and III.
Atlas fracturesFractures of the first vertebra occur in 2–13% of cervical injuries, usually as a result of falls, direct impact with hyperextension mechanisms or axial compression of the cervical spine.16 A bimodal distribution by age can be seen, with a peak in young adults and another in older adults.17
The classic Jefferson fracture is a four-part "burst" fracture of C1, which compromises the anterior and posterior arch of the vertebra bilaterally, although two- or three-part fractures are more common (Fig. 3D and E).18 They are usually associated with other cervical fractures, particularly of C2 (44%) (Fig. 3F), and rarely result in neurological injury because they tend to widen the spinal canal.
Jefferson classification (adapted by Gehweiler et al.19):
–Type I: isolated uni/bilateral fracture of the posterior arch.
–Type II: isolated uni/bilateral fracture of the anterior arch.
–Type III (Jefferson burst fracture): unilateral or bilateral fracture of both arches.
–Type IV: fracture of the lateral mass.
–Type V: transverse fracture through the anterior arch. Secondary to avulsion of the long neck muscle or the atlantoaxial ligament.
The transverse atlas ligament is one of the main stabilisers of the atlantoaxial joint. MRI is more sensitive than CT in assessing its integrity, although there are indirect signs on CT to make us suspect injury:
- −
Predental space greater than 3mm in adults and 5mm in children.
- −
Cranially divergent predental angle greater than 12° ("V" sign).
- −
The sum of the displacement of the lateral masses of the atlas with respect to the external margins of the axis greater than 7mm.
- −
Avulsion of the tubercle of C1 at the insertion of the transverse ligament.
- −
C1-C2 spinolaminar distance greater than 8mm.
In some cases there may be an isolated rupture of the transverse ligament of the atlas, with no associated fracture. These lesions are classified, according to Dickman et al.,20 as:
–Type I: disruption of the substance of the ligament.
–Type II: fracture/avulsion of the bony tubercle for the insertion of the transverse ligament into the lateral mass of the atlas.
The main determining factors for surgical treatment are the associated cervical fractures and the integrity of the transverse ligament, the most common rupture being in types III and IV of the Jefferson classification (adapted by Gehweiler et al.19).
Axis fracturesFractures of the densFractures of the dens (also known as odontoid process) represent 10–20% of cervical spine fractures, the most common being of the axis. The highest incidence is also in young people and people over the age of 65.4,5 Anderson and D'Alonzo classified them into three types5,16:
–Type I: consists of a fracture line at the tip of the dens and may be associated with injury to the alar ligaments.
–Type II: these are the most common, with a fracture line between the body of the axis and the dens. If it is not displaced, it can easily go unnoticed.
–Type III: the fracture is located in the body of the axis.
Type I and III fractures are usually managed conservatively. There is a lack of consensus on the therapeutic approach for type II, but consolidation rates are significantly higher with surgical treatment than with conservative treatment.16
Hangman's fracture or traumatic spondylolisthesis of the axisThis represents 4% of cervical spine fractures and approximately 22% of axis fractures.4,16 It is a bilateral fracture of the pars interarticularis, although it also includes fractures that go through the pedicles, posterior body of the axis and laminae.4,5,21 They do not usually cause neurological impairment. Levine's classification subdivides them into three types4,5,16,21:
–Type I: displacement <2mm, without angulation. Management is usually conservative (Fig. 4A and B).
Figure 4.CT of cervical spine. (A) Cervical sagittal reconstruction showing a displaced Hangman type I fracture <2mm, without angulation (arrow). (B) Sagittal volumetric reconstruction of the same patient. (C) Normal postural rotation C1-C2, axial: a normal rotation angle of 40° is shown, between the transverse axes of C1 and C2 traced through the medial joint area of the lateral masses of the atlas and the articular facets superior to the axis. The rotational angle is obtained in the axial plane, evaluating C1 and C2 simultaneously in the same image using the maximum intensity projection (MIP) post-processing technique. (D) C1-C2 normal postural rotation, sagittal reconstruction in the midline: there is no anterior displacement of C1 with respect to the dens (arrow). (E) Fielding classification. Anterior displacement of C1 (arrows). Type I: unilateral displacement of one of the C1 masses without displacement of the anterior arch of the atlas with respect to the dens (3mm, normal in adults). Type II: unilateral anterior displacement of one of the C1 masses with displacement of the anterior arch of the atlas with respect to the dens of 3–5mm. Type III: anterior displacement of both lateral masses of the atlas with displacement of the anterior arch with respect to the dens >5mm. Type IV: posterior displacement of C1, pathological or insufficient dens (os odontoideum, hypoplastic or fractured dens).
(0.2MB).–Type II: characterised by anterior angulation >11° with displacement >2mm. Treatment may be conservative or surgical.
–Type III: the most uncommon, characterised by fracture-dislocation or bilateral facet dislocation, they are unstable and require surgery.
The third most common type, they are a heterogeneous group of fractures that includes lateral mass fracture. Treatment is usually conservative.4
Atlantoaxial rotatory subluxationTraumatic subluxation in adults is unusual.22 The atlantoaxial joints allow a wide normal axial rotation with an estimated maximum of 48–52°.4,5,16
Bilateral facet subluxation is estimated to occur at around 64° and if it is greater there is more chance that the rotatory subluxation will transform into a chronic atlantoaxial rotatory fixation, also called rigid atlantoaxial rotatory subluxation, which cannot usually be reduced.4,5,16,22 Early diagnosis is essential but cannot be established exclusively with a CT, and it can be misdiagnosed simply because the patient's head is rotated during the test.16 MRI shows the ligamentous lesions and confirms the diagnosis.22,23 Fielding classifies this disease based on the displacement of C1 with respect to the dens in the sagittal plane (Fig. 4C and E)4,16:
–Type I: the most common, occurring in the normal rotational range between C1-C2, without anterior displacement of the atlas (3mm, normal in adults), with ligament intact. It includes pathological and normal conditions, misnamed subluxations and, to differentiate between them, it may be useful to consider the clinical context, the presence of other associated cervical spine injuries, whether traumatic or not, rotational angle >52° and performing a dynamic CT/MRI.
–Type II: unilateral anterior displacement of one of the C1 masses of 3−5mm, means transverse ligament injury.
–Type III: lesion of the alar and transverse ligaments, which causes anterior displacement of both lateral masses of the atlas >5mm.
–Type IV: uncommon, characterised by a pathological or insufficient dens (os odontoideum, hypoplastic or fractured dens), which causes a posterior displacement of C1.
Types II and IV can compromise the spine.4,16 Although there is a lack of consensus as to the most appropriate treatment,22 surgery is recommended if there is significant angulation between C1 and C2 (>30°), focal neurological deficits, displacement >2mm with focal neurological deficits or unstable C1-C2 dislocation in symptomatic patients.16
Subaxial injuriesSubaxial injuries include any lesion, whether bony or ligamentous, of the subaxial cervical skeleton, involving C3 to C7. Multiple attempts to classify them have fallen into disuse due to the complexity of integrating different injury mechanisms, positions and force vectors, which combine with each other to bring about high intra- and inter-observer variability.24
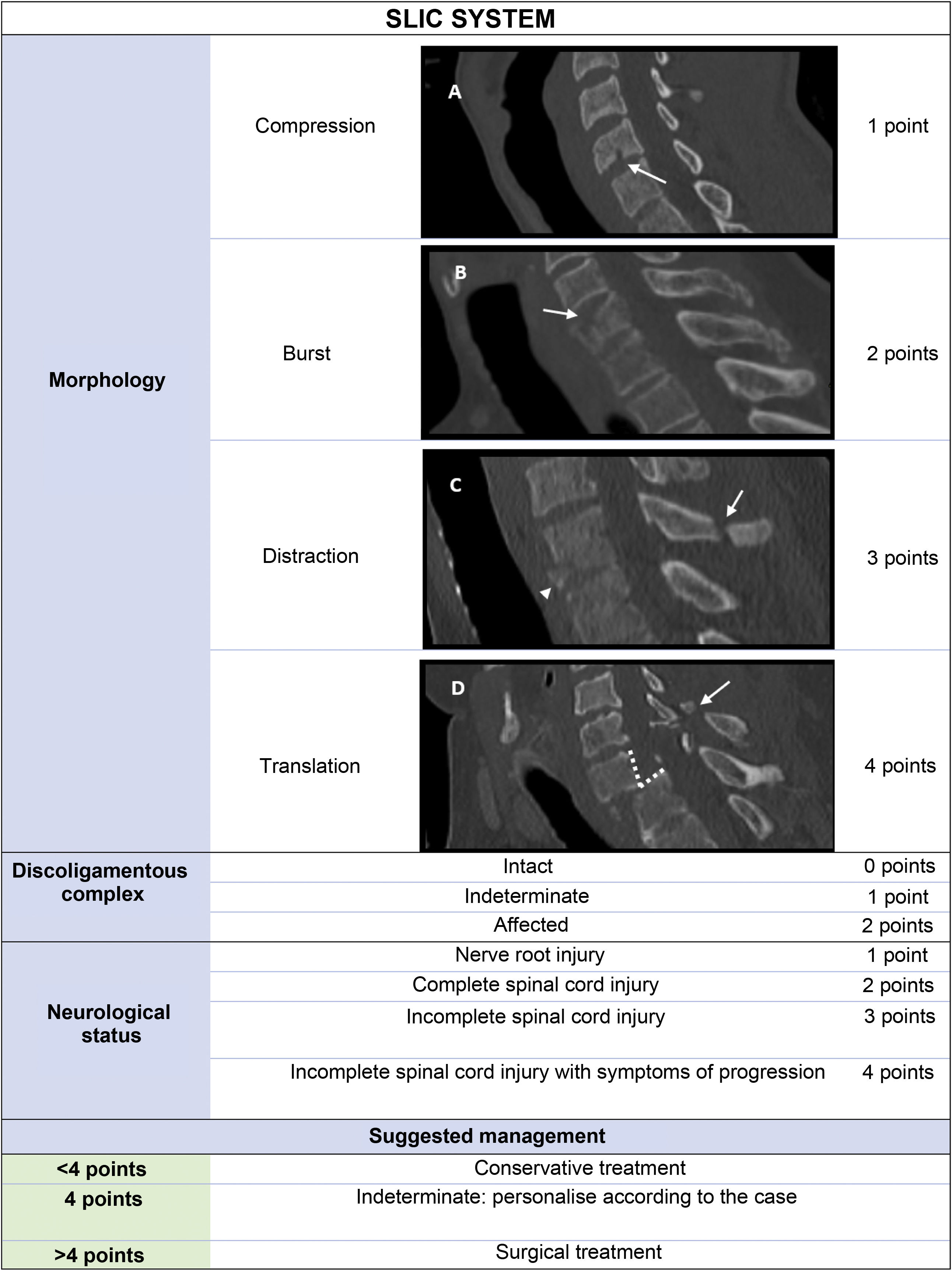
Currently, the systems most widely used, for ease in assessing and communicating the severity of these injuries, and for being more applicable in clinical decision-making, are the AO Spine and Subaxial Injury Classification and Scoring (SLIC) systems.25 We will now take a closer look at the SLIC system, in view of the great expansion in its use, and its practicality and simplicity (Fig. 5).4
The SLIC system is based on the assessment of three categories (morphology, discoligamentous complex and neurological status), which include different variables to which a score is assigned based on their severity. Where several coexist, only the one with the highest score will be counted. Conservative or surgical management will be decided on according to the total score obtained. (A) 21-year-old male fall victim. Compression fracture: disruption of the anterior-inferior cortex of the vertebral body (arrow) with a small undisplaced "teardrop" fragment. (B) 56-year-old male with a 6-m fall. Burst fracture: sagittal fracture of the vertebral body (arrow) with retropulsion of the posterior fragment into the spinal canal. (C) 46-year-old male with multiple trauma after falling off a bicycle. Distraction-hyperextension fracture: teardrop fracture with anterior-inferior avulsion of the fragment (arrowhead) and displaced fracture of the spinous process (arrow). (D) 58-year-old male with sports trauma. Translation fracture: marked anterolisthesis (dashed lines) with invasion of the spinal canal and comminuted and displaced fracture of the spinous process (arrow).
Also called wedge fractures, they are caused by an axial compression and hyperflexion injury mechanism. They do not generally cause ligament injury:
- −
Involvement of the anterior superior cortex.
- −
Loss of height of the vertebral body.
- −
The posterior cortex must be intact with no associated retropulsed fragments.
- −
"Teardrop" fractures and fractures of isolated posterior bone elements (facets, laminae and spinous processes) are also included, in the absence of distraction, translation or significant displacement (Fig. 5A).1
Same compression injury mechanism, but to a greater extent:
Distraction fracturesThese always entail ligament involvement due to dissociation in the vertical axis by two mechanisms.4
In the posterior aspect due to hyperflexion:
- −
Spectrum of injuries from facet subluxation (<50% joint congruence and diastasis >2mm) to complete dislocation.
- −
Usually associated with compression of anterior vertebral elements:
- −
Teardrop fractures.
- −
Widening of the posterior aspect of the intervertebral space, with angulation >11°.
- −
Focal kyphotic deformity.
In the anterior aspect due to hyperextension:
- −
Common with falls in older adults with spondylitis/osteoporotic spines or intoxicated patients who suffer accidents with sudden deceleration.
- −
They result in "teardrop" fractures, with anterior-inferior avulsion of the fragment (Fig. 5C).
- −
They are usually associated with a widening of the anterior aspect of the intervertebral space and disruption of the anterior longitudinal ligament and disc.
Other consequences of hyperextension are facial trauma and compression fractures of the posterior elements.
Translation or rotation fracturesDefined by a dissociation in the horizontal axis: breach of the spinolaminar line, separation of fragments or listhesis >3.5mm (Fig. 5D). They always cause instability:
–The pure translation mechanism occurs due to bilateral ligament disruption and does not occur without a prior distraction component.
–In the rotation mechanism, an intact facet joint unilaterally serves as a pivot, which is why they occur after unilateral or bilateral facet dislocations.
–Teardrop fractures due to hyperflexion with facet dislocation (prior distraction) are common, leading to retrolisthesis and invasion of the spinal canal.4
The discoligamentous complex (DLC) is the set of elements providing stability to the cervical spine. It consists of (Fig. 2):
Anterior ligament complex (ALC): anterior and posterior longitudinal ligaments and intervertebral discs.
Posterior ligament complex (PLC): facet capsules and yellow, interspinous, supraspinous and nuchal ligaments.
Structures of the craniocervical junction: cruciform ligament of the atlas, alar ligaments, apical ligament and anterior, posterior and tectorial atlanto-occipital membranes.
Injury causes instability and severe neurological sequelae without treatment, so it is an independent prognostic factor (Fig. 5).
MRI is the gold standard for assessing DLC injuries. However, CT may also initially show indirect signs of DLC involvement. For example, facet dislocation/subluxation is a marker of capsular injury, whereas asymmetric widening of the anterior aspect of the intervertebral space often results in involvement of the anterior longitudinal ligament. In addition, distraction fractures are invariably associated with ligament injury and require surgery. In all these cases, the DLC is considered to be affected and, even if only one structure is injured, 2 points are awarded for this section of the SLIC system.
In two cases, an indeterminate injury is considered, and 1 point awarded:
- −
Abnormalities in DLC signal intensity on T2-weighted sequences in the absence of bone lesion.
- −
Isolated widening of the interspinous distance with respect to the rest, as the injury of the interspinous ligament provides less instability.
In the event they coexist, the injury with the highest score prevails.
Neurological statusThis is an element of great prognostic importance, but set apart from the radiological work which is the focus of the two previous sections. The clinicians determine the score for this section (Fig. 5) based on the patient's symptoms and neurological examination. Incomplete spinal cord injury has a higher score than complete spinal cord injury because after urgent surgery, it is associated with a better prognosis.4
Knowing the symptoms allows us to focus the radiological interpretation and we must always stress the need to perform an urgent MRI in cases of neurological symptoms indicative of spinal cord compression.24
Emergency CT radiological findings which may particularly indicate a spinal cord injury include narrowing of the spinal canal and abnormalities in vertebral alignment, with retropulsion and invasion of bone fragments into the canal.2 In some cases, hyperdense intracanal collections can be seen, which correspond to spinal haematomas.
ManagementAfter adding the scores of the different sections, conservative management is recommended for up to 3 points and surgical management for 5 points and above. When the score is 4, it is recommended to proceed on a personalised basis by taking into account other patient factors.1,4
Associated vascular lesionsArterial lesionsArterial lesions have high morbidity and mortality rates without early treatment for cerebral ischaemia, especially when they affect the internal carotid arteries (ICA) and the vertebral arteries (VA).26 They are found in 1.5% of patients with multiple trauma, increasing to 8% if there is involvement of C1-C3,27,28 and occur when the vascular wall is subjected to forces of stretching, torsion, compression against bone structures and even laceration by sharp fragments.29
CT angiography of the supra-aortic trunks and circle of Willis is the diagnostic technique of choice due to its availability and speed26, and the main indications according to the recommendations of the Western Trauma Association based on the modified Denver criteria are listed below.30
Signs to raise clinical suspicion:
–Evidence of arterial bleeding from the neck, mouth, nose or ears.
–Expansive neck haematoma.
–Carotid bruits in <50-year-olds.
–Newly appeared focal neurological signs.
Radiological signs to raise clinical suspicion:
- −
Fractures: of the Le Fort II and III facial mass; mandibular; of the base of the skull with involvement of the carotid canal; any at the level of C1, C2 and C3; and fractures of the rest of the cervical vertebral bodies if there is extension to the transverse foramen.
- −
Subluxations and ligament injuries.
- −
Signs of acute ischaemia or signs of diffuse axonal damage on skull base CT in patients with a low level of consciousness.
- −
Injury to the main thoracic vascular structures.31
It should be noted that in 80% of patients there is an asymptomatic latent period of varying duration. Up to 30% of cervical spine vascular lesions had no suspicious signs.32
Denver scaleThis is widely accepted system with prognostic and therapeutic implications to assess the severity of traumatic vascular injuries33:
- −
Grade 1: minimal intimal lesion (contour irregularity), dissection or intramural haematoma with <25% stenosis.
- −
Grade 2: intraluminal thrombus, dissection or intramural haematoma with >25% stenosis.
- −
Grade 3: pseudoaneurysms.
- −
Grade 4: dissection or thrombus causing complete occlusion of the vessel.
- −
Grade 5: artery transection or arteriovenous fistulas.
These lesions can change over time and even change in grade. Imaging follow-up is recommended in asymptomatic patients after 7–10 days or according to the symptoms and, subsequently, every 3−6months until recovery.30
At times it may be difficult to interpret images that do not strictly meet these criteria, so these are classified as radiologically indeterminate. In such cases, a follow-up CT angiogram is recommended after 48h, as progression to a classifiable lesion has been observed in 25%, while in up to 39% it can be confidently ruled out.34
The type of artery damaged also plays a role; in the case of VA lesion, a higher grade does not always mean a worse prognosis. The incidence of stroke according to the type of lesion when the ICA and VA are affected is, respectively, 3% and 6% in grade 1; 14% and 38% in grade 2; 26% and 27% in grade 3; 50% and 28% in grade 4; and, lastly, 100% for both in grade 5.35
Antithrombotic therapy is indicated in all patients without contraindications and surgical/endovascular treatment is reserved for grades 3, 4 and 5, and for grade 2 when associated with neurological symptoms or progression of the dissection.35
Venous injuriesThe internal jugular veins may be affected by laceration and haematoma or thrombus formation. The “hyperdense sinus” sign should be looked for on non-contrast head CT and the “empty delta” sign in the venous phase in contrast-enhanced CT. With the “empty delta” sign, a sinus filling defect can be seen (usually triangular in shape), which represents the thrombus and is surrounded by an enhancing rim of the dura mater and collateral vessels. As a result of early venographic acquisitions, whether due to poor technique or a patient's pre-existing conditions, such as intracranial hypertension, the sinus may not have had time to fill with contrast and the "false empty delta sign" or "pseudo-delta sign" can occur, with this being a relatively common source of false positives. To avoid this, we have to verify correct filling of the rest of the cerebral veins.
ConclusionsMultidetector CT (MDCT) is the initial technique of choice in cervical spine trauma. X-ray might be indicated when MDCT is not available, but never as a substitute. In fractures of the craniocervical junction (C0-C3), dislocations/subluxations or involvement of the transverse foramen at any level, a CT angiogram of the supra-aortic trunk should be obtained, as vascular lesions can be silent and delayed. MRI is justified when there is suspicion of a neurological or disc-ligament injury. We recommend following a system for reading the images that avoids relevant injuries being overlooked, describing the findings and then attempting to classify the injuries according to the classifications used in each centre. This will ensure that we are speaking a common language and help therapeutic and prognostic decision-making.
Authorship- 1
Responsible for the integrity of the study: SOV, LSC, JMCG, ADT and MMG.
- 2
Study conception: SOV, LSC, JMCG, ADT and MMG.
- 3
Study design: SOV, LSC, JMCG, ADT and MMG.
- 4
Data collection: SOV, LSC, JMCG, ADT and MMG.
- 5
Data analysis and interpretation: SOV, LSC, JMCG, ADT and MMG.
- 6
Statistical processing: not applicable.
- 7
Literature search: SOV, LSC, JMCG, ADT and MMG.
- 8
Drafting of the article: SOV, LSC, JMCG, ADT and MMG.
- 9
Critical review of the manuscript with intellectually relevant contributions: SOV, LSC, JMCG, ADT and MMG.
- 10
Approval of the final version: SOV, LSC, JMCG, ADT and MMG.
The authors declare that they have no conflicts of interest.