The pandemia caused by the SARS-CoV-2 virus has triggered an unprecedented health and economic crisis. Although the diagnosis of infection with SARS-CoV-2 is microbiological, imaging techniques play an important role in supporting the diagnosis, grading the severity of disease, guiding treatment, detecting complications, and evaluating the response to treatment. The lungs are the main organ involved, and chest X-rays, whether obtained in conventional X-ray suites or with portable units, are the first-line imaging test because they are widely available and economical. Chest CT is more sensitive than plain chest X-rays, and CT studies make it possible to identify complications in addition to pulmonary involvement, as well as to suggestive alternative diagnoses. The most common radiologic findings in COVID-19 are airspace opacities (consolidations and/or ground-glass opacities), which are typically bilateral, peripheral, and located primarily in the lower fields.
La pandemia por el virus SARS-CoV-2 ha desencadenado una crisis económica y sanitaria sin precedentes. Aunque el diagnóstico es microbiológico, las técnicas de imagen tienen un papel importante para apoyar el diagnóstico, graduar la gravedad de la enfermedad, guiar el tratamiento, detectar posibles complicaciones y valorar la respuesta terapéutica. La afectación es principalmente pulmonar. La radiografía de tórax en sala convencional o portátil es el primer método de imagen por su amplia disponibilidad y bajo coste. La tomografía computarizada torácica tiene una mayor sensibilidad que la radiografía de tórax y permite valorar tanto la afectación pulmonar como posibles complicaciones, además de proporcionar diagnósticos alternativos. Los hallazgos radiológicos más frecuentes son las opacidades del espacio aéreo en forma de consolidaciones y/u opacidades en vidrio deslustrado, con distribución típicamente bilateral, periférica y de predominio en los campos inferiores.
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by a coronavirus strain called severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The first cases were seen in Wuhan, China, in late December 2019. From there, it quickly spread to virtually the entire world. It was officially recognised as a pandemic by the World Health Organization (WHO) on 11 March 2020. The rapid international spread of the virus has had enormous social, economic and health repercussions and has forced the adoption of extraordinary social confinement measures to halt its dissemination, as well as the structuring of healthcare to prevent its collapse. In late October 2020, the number of confirmed cases of COVID-19 worldwide reached 46 million, and the death toll exceeded 1,140,000.1
The infection is transmitted predominantly through contact with droplets of secretions from the upper respiratory tract of infected individuals.2 Contaminated droplets deposited on objects can facilitate transmission of the virus.3 Currently, other routes of transmission such as faecal-oral, sexual, blood and vertical transmission are not well understood.4
Infection generally occurs within 14 days of exposure and in most cases within 4–5 days.5 Although it can occur at any age, it is most common in middle-aged and elderly male adults.
The novelty of the disease and the initial lack of knowledge about it spurred huge amounts of scientific output in biomedical journals. This update features a compendium of the most significant findings in radiological diagnosis of COVID-19.
Clinical signsClinical presentationIn many cases, SARS-CoV-2 infection is asymptomatic.6 A review of the scientific literature estimated the proportion of asymptomatic patients at 30–40%.7
In symptomatic individuals, COVID-19 typically presents with systemic and/or respiratory symptoms, although here have also been reports of gastrointestinal, cardiovascular and, less commonly, dermatological and neurological symptoms.
The signs and symptoms of COVID-19 are non-specific and cannot be clinically distinguished from other viral respiratory infections, though the development of dyspnoea several days after the onset of symptoms is suggestive of COVID-19.8,9
The most common associated symptoms include: cough (50%), subjective fever or fever higher than 38 °C (43%), myalgia (36%), headache (34%), dyspnoea (29%), sore throat (20%), diarrhoea (19%), nausea/vomiting (12%), anosmia, ageusia, dysgeusia (<10%), abdominal pain (<10%) and runny nose (<10%).8–10 It should be noted that fever is not a universal finding, even among hospitalised cohorts.
Smell and/or taste abnormalities have been reported primarily in patients with mild to moderate COVID-19, at rates ranging from 34% to 87%.11
Gastrointestinal symptoms are less common, though they may be the first sign. A prevalence of gastrointestinal symptoms of 18% (diarrhoea, 13%; nausea/vomiting, 10%; and abdominal pain, 9%) has been reported.12
Skin alterations similar to erythema pernio (chilblains) have also been reported, especially in the fingers and toes and generally in children and young adults. These sometimes occur without other associated symptoms and with negative polymerase chain reaction (PCR) results. In most cases, they are self-limiting, with gradual spontaneous resolution.13
Spectrum of severityThe clinical spectrum of COVID-19 ranges from asymptomatic and paucisymptomatic forms to severe forms characterised by respiratory failure, sepsis, shock and organ dysfunction syndromes that require mechanical ventilation and intensive care unit (ICU) admission. In a Chinese study of 44,500 patients with confirmed infection, 81% were mildly ill, 14% were severely ill (dyspnoea, hypoxia or pulmonary involvement in excess of 50% on imaging) and 5% were critically ill (respiratory failure, shock or multiple organ dysfunction syndrome).14
Among patients admitted for COVID-19, the proportion of critical or fatal illness is higher. In a study of 2741 hospitalised patients,15 24% died and 27% required intensive care, of which 60% died.
Risk factorsAdvanced age is associated with a higher mortality rate. A fatality rate of 8–12% has been reported among people 70–79 years of age, and a fatality rate of 15–20% has been reported in those over 80 years of age. By contrast, the overall fatality rate is 2.3%.14,16 In another study, 80% of deaths occurred in people 65 years of age or older.17 Men have a higher mortality rate than women.14,16,17
An increased risk of severe disease has also been reported in patients with medical comorbidities such as cardiovascular disease, diabetes mellitus, arterial hypertension, chronic lung disease, cancer (especially haematologic neoplasms, lung cancer and metastatic disease), chronic kidney disease, obesity and smoking.4,14
Laboratory abnormalities linked to a worse prognosis include: lymphopenia, elevated liver enzymes, elevated lactate dehydrogenase (LDH), elevated inflammatory markers such as C-reactive protein (CRP) and ferritin, elevated D-dimers (>1 μg/ml), elevated troponin and creatine phosphokinase (CPK) levels, prolonged prothrombin time, and acute kidney injury.18 Abnormalities in coagulation tests have also been observed, with a state of hypercoagulability leading to a tendency towards thrombosis.
DiagnosisThe standard test for the detection of SARS-CoV-2 is reverse transcription-polymerase chain reaction (RT-PCR), usually done on a sample of nasopharyngeal or respiratory secretions. RT-PCR is believed to be highly specific, but its sensitivity can range from 60–70%19 to 95–97%,20 so false negatives are a real clinical problem, especially in the early stages. Sensitivity varies by time elapsed since exposure to SARS-CoV-2. The rate of false negatives is 100% on the first day after exposure, then decreases to 38% on the day of onset of symptoms and drops to 20%, its lowest level, on the third day of symptoms.21
Imaging tests play an important role in detection in and management of these patients, and have been used to help diagnose the disease, determine its severity, guide treatment and assess treatment response. The current recommendation of the vast majority of scientific and radiological associations is that imaging tests should not be used as screening tools for detecting COVID-19. Rather, they should be reserved for evaluating complications.22
Chest X-rayRooms and projectionsChest X-ray is generally the first-line imaging test in patients with suspected or confirmed COVID-19 due to its usefulness, availability and low cost, though it is less sensitive than computed tomography (CT).23 The optimal chest X-ray includes posteroanterior (PA) and lateral projections with the patient standing.24
Taking chest X-rays in conventional rooms puts uninfected patients and diagnostic imaging staff at risk, given the potential for disease transmission through droplet-contaminated surfaces.25 This means that the room must be disinfected after each use.25,26 Establishing a dedicated conventional radiology room for all COVID-19 patients can be useful for reducing transmission,27 though not all centres are able to allocate their resources in this way.
Performing a chest X-ray in an anteroposterior (AP) projection using a portable system helps reduce the spread of the infection, as this system can be easily cleaned and placed in designated facilities for patients with COVID-19. This limits the need for moving around potentially infected patients within the hospital and reduces the use of personal protective equipment (PPE).25–28 It is the first-line radiological test recommended by the American College of Radiology (ACR).24 It is also the only one that can be performed in critically ill and ICU patients. Its interpretation is often limited by the lower degree of inspiration and by the magnification of the cardiomediastinal silhouette resulting from the AP projection. However, despite its limitations, it enables assessment of catheter and device placement, detection of possible complications (such as pneumothorax, subcutaneous emphysema and pneumomediastinum) and serial monitoring of the course of the disease.
SensitivityOne limitation of chest X-ray, like PCR, is the high rate of false negatives. Possible causes are: the prematurity of the imaging test and the absence of pulmonary disease at the time of presentation; the limitations of the X-ray technique, especially in portable X-ray systems;24 and the fact that the ground-glass opacities and reticular pattern typical of COVID-19 can be difficult to detect on chest X-ray.
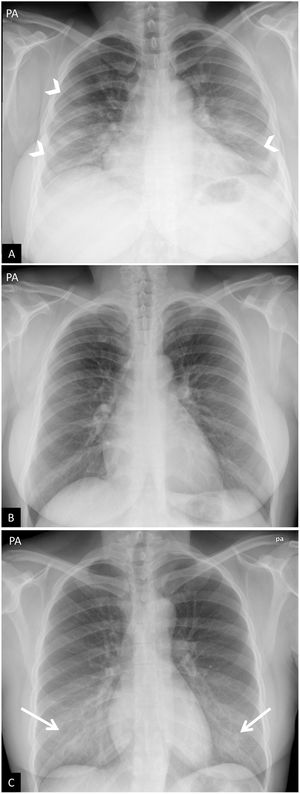
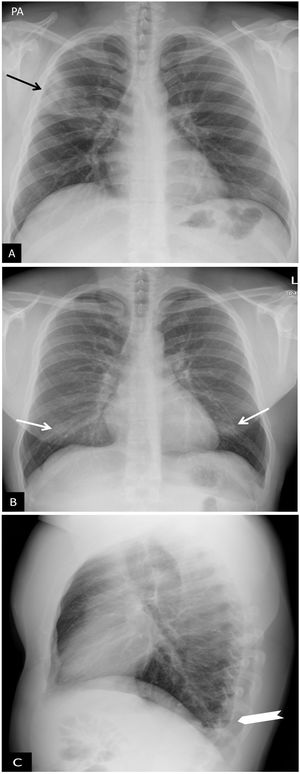
False positives on chest X-rays may be caused by lack of inspiration, breast prominence and poor positioning of the patient, which can lead to the scapulae and soft tissues projecting onto lung fields, thus increasing the density of the lung periphery and simulating ground-glass opacities (Fig. 1). The sensitivity of portable chest X-ray in the detection of COVID-19 in patients compared to PCR has been the subject of numerous studies. Initially, these did not show very high figures for sensitivity,24 though it has improved up to 89% in settings with a very high disease prevalence.29
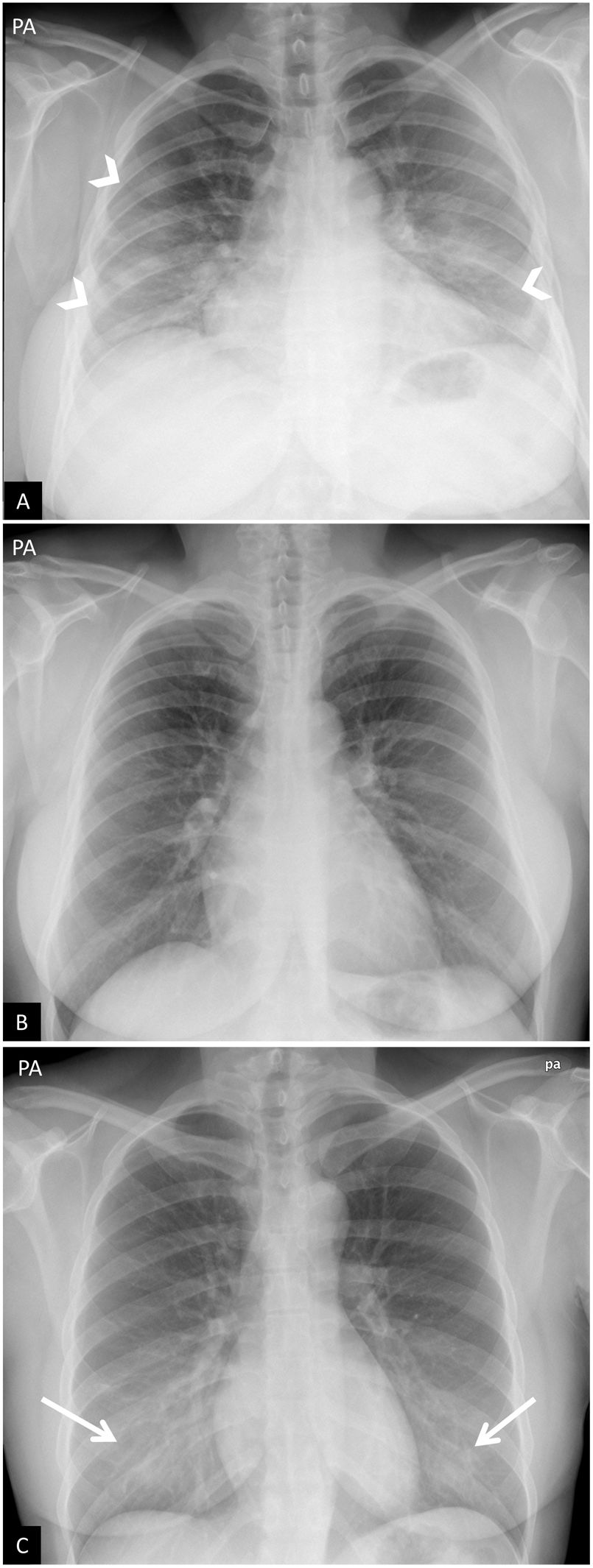
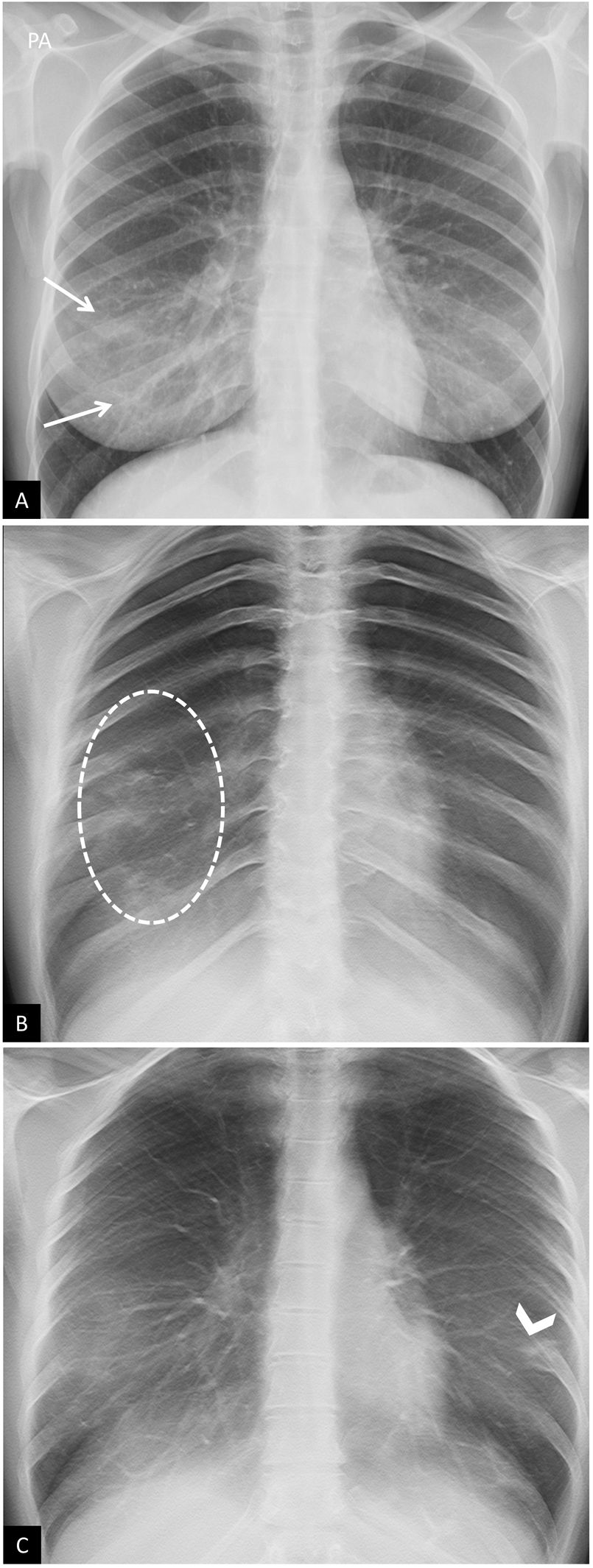
False positives or pitfalls. (A and B) Chest X-ray with poor inspiration. A 38-year-old woman with signs and symptoms raising suspicion of COVID-19. (A) Posteroanterior chest X-ray. Bilateral increase in density, predominantly in the middle and lower fields, raising suspicion of COVID-19 pneumonia (arrow tips). Poor inspiration (7 posterior costal arches are identified) and voluminous breasts. (B) Same patient. Repeat chest X-ray a few minutes after forced inspiration, wherein all above-mentioned findings are no longer seen (note the change in the morphology of the cardiac silhouette). (C) Artefact due to high breast density. An 18-year-old woman with signs and symptoms raising suspicion of COVID-19. Bilateral symmetrical opacities in lower fields due to highly dense breast tissue (arrows). Negative PCR results for SARS-CoV-2.
The sensitivity of portable chest X-ray is lower than that of CT (69% versus 97–98%),28 but in some publications they are the same.29
Although there are significant differences in sensitivity between PCR, CT and portable X-ray, it is accepted that the latter can be used as a triage method in certain scenarios:25,26,28,29 environments where there is a high prevalence of COVID-19 (community transmission); centres with limited access to PCR, CT and rapid tests, but with availability of portable chest X-ray systems; and patients with severe symptoms, so as to accelerate their classification, hospital admission and treatment.
Chest X-ray findingsThe chest X-ray may be normal in mild cases or early-stage disease, but patients with moderate to severe symptoms are unlikely to have a normal chest X-ray.28,30 Most are pathological in patients requiring hospitalisation (69% at admission and 80% at some point after admission).23 Findings are more extensive 10–12 days after the onset of symptoms.23
The most common findings are airspace opacities, which may be consolidations or, less frequently, ground-glass opacities.23
Chest X-ray findings in patients with suspected COVID-19 have been divided into four categories to facilitate diagnosis:26,30–32
- •
Normal chest X-ray. It is not uncommon for the chest X-ray to be normal early in the disease, so a normal X-ray does not rule out infection.28,30
- •
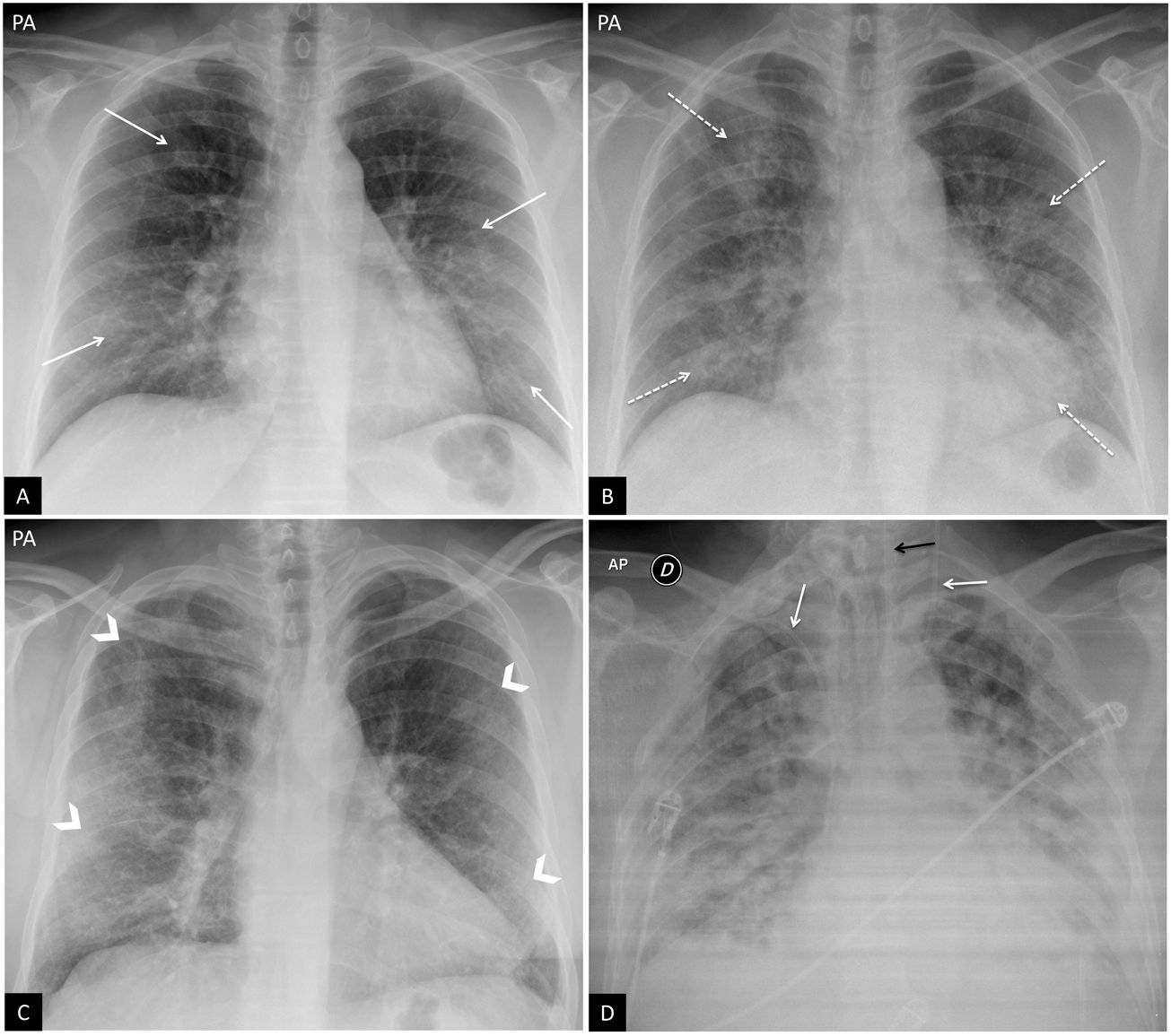
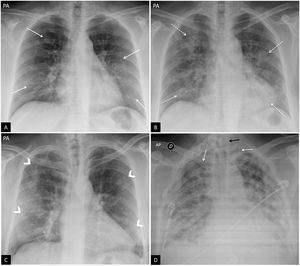
Typical findings or findings commonly associated with COVID-19 in the scientific literature (Fig. 2). These include a reticular pattern, ground-glass opacities and consolidations, with rounded morphology and a confluent or patchy multifocal distribution. The distribution is usually bilateral and peripheral, with a predominance in the lower fields23 (Fig. 2). The differential diagnosis includes organising pneumonia, drug toxicity and other causes of acute lung damage. Between the first and third week from the onset of symptoms, typical X-ray findings may progress to diffuse disease. This is related to a severe clinical hypoxaemia situation, and the main differential diagnosis is acute respiratory distress syndrome (ARDS).
Figure 2.Typical findings in COVID-19 pneumonia. (A) A 47-year-old woman with signs and symptoms raising suspicion of COVID-19. Posteroanterior (PA) chest X-ray. Reticular interstitial pattern with peripheral predominance (arrows). (B) Same patient as in image A. PA chest X-ray taken 3 days later. Positive PCR for SARS-CoV-2. Despite being taken with poorer inspiration, the X-ray shows faint rounded bilateral peripheral alveolar opacities (dotted arrows). (C) A 57-year-old male with dyspnoea and positive PCR for SARS-CoV-2. Bilateral peripheral opacities in upper, middle and lower fields (arrow tips). (D) A 45-year-old male with dyspnoea and COVID-19 confirmed by PCR. Anteroposterior chest X-ray showing multiple bilateral diffuse confluent areas of consolidation with extensive involvement of both lungs. Note the presence of two central venous lines, one left jugular and the other right subclavian (white arrows), and a gastrointestinal tube (black arrow).
(0.13MB). - •
Indeterminate findings and findings that may present in cases of COVID-19 pneumonia can have other causes. These include consolidations and ground-glass opacities with a unilateral, central or upper-lobe distribution (Fig. 3A). The differential diagnosis includes other infections and alveolar oedema.
Figure 3.Atypical findings in COVID-19 pneumonia. (A) Lobar pneumonia. A 28-year-old male with signs and symptoms consistent with COVID-19 and positive PCR for SARS-CoV-2. Chest X-ray in posteroanterior (PA) projection. Right upper lobe involvement (arrow). (B and C) Bilateral involvement and pleural effusion. A 17-year-old male with fever and positive PCR for SARS-CoV-2. PA (B) and lateral (C) chest X-ray. Faint bilateral infiltrates in lower fields (arrows) with minimal pleural effusion in the left posterior costodiaphragmatic sinus (arrow tip).
(0.21MB). - •
Atypical findings, uncommon findings or findings not reported in COVID-19 pneumonia. These include lobar consolidation, lung nodules or masses, miliary pattern, cavitation and pleural effusion, reported in only 3% of patients23 and more typical of advanced disease (Fig. 3B and C).
A correlation has been discovered between the progressive chest X-ray findings and the onset of symptoms: in the first few days, reticular involvement predominates over ground-glass opacities, then, after an overlap period, the ground-glass pattern becomes the dominant one, while consolidations are more typical of later stages.32
Disease gradingA multitude of publications have emerged seeking to establish criteria to grade the severity of the involvement seen on chest X-rays in patients with COVID-19. Their objectives are:
- •
To establish a common language to classify disease severity in these patients.30
- •
To correlate severity of radiological involvement with clinical and demographic parameters.33,34
- •
To aid in monitoring the clinical progression.28
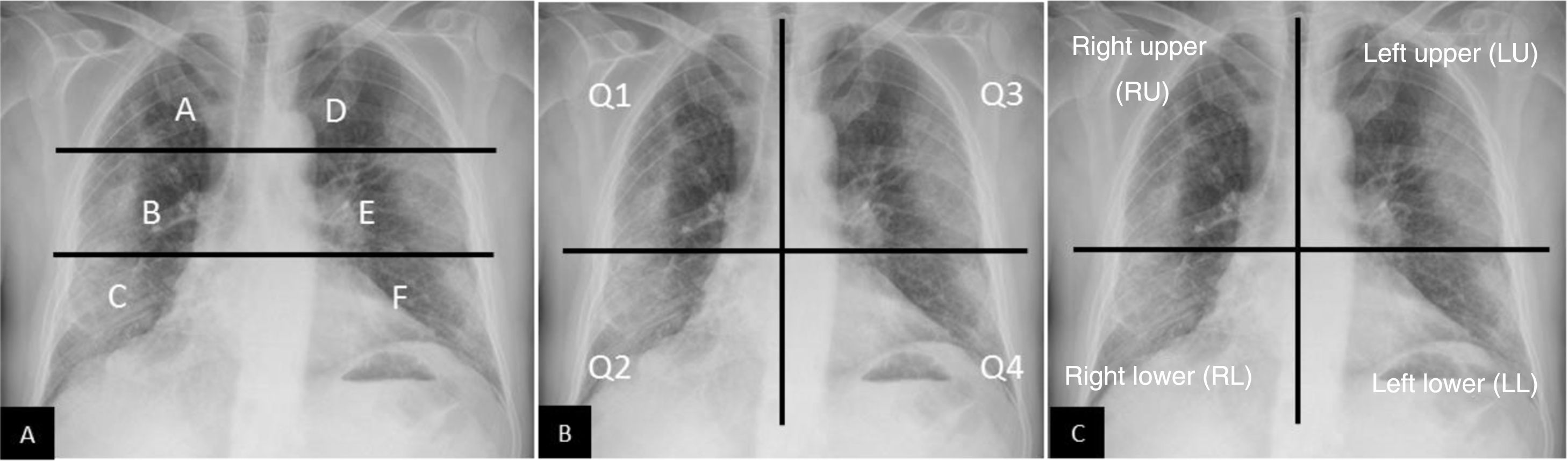
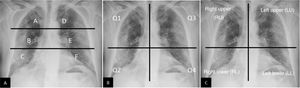
All authors use AP or PA projections28 and divide them into various regions: some based on anatomical boundaries30,33 and others dividing the lung fields into two or three equal parts33,35 (Fig. 4). To determine the severity, some authors assign a quantitative value to type of involvement33,36 and/or number or percentage of affected fields,28,30 and finally obtain a severity score.
Methods for grading severity of pulmonary involvement secondary to COVID-19 by chest X-ray. (A) Grading method suggested by Borghesi et al.33,34 Using an upper horizontal line (lower edge of the aortic arch) and a lower horizontal line (lower edge of the right inferior pulmonary vein), 6 lung fields are obtained. Each field is assigned a score based on radiological findings: 0 if there are no findings; 1 if there are interstitial infiltrates; 2 if there are interstitial and alveolar infiltrates with an interstitial predominance; and 3 if there are interstitial and alveolar infiltrates with an alveolar predominance. The maximum score is 18. According to this grading system, in the case presented, the score would be: A = 2, B = 3, C = 3, D = 3, E = 3 and F = 3. Total score = 17/18. (B) Adaptation of the “Radiographic Assessment of Lung Edema” (RALE) method proposed by Warren et al.35, initially devised to grade the severity of acute pulmonary oedema. Using a vertical line (along the spine) and a horizontal line (along the lower edge of the left main bronchus), 4 quadrants are obtained. Each quadrant is assigned a score of 0–4 depending on the extent of consolidation or ground-glass opacities (0 = no findings; 1 < 25%; 2 = 25%–50%; 3 = 50%–75%; 4 > 75%). These scores must be multiplied by another score assigned to consolidation density (1 = incipient, 2 = moderate, 3 = dense). The maximum score is 48. According to this grading method, the example presented would be scored as follows: Q1 = 2 × 1 = 2; Q2 = 4 × 3 = 12; Q3 = 2 × 3 = 6, and Q4 = 2 × 3 = 6. Total score = 26/48. (C) Grading method used by Schalekamp et al.78. This divides the thorax into 4 quadrants. Each quadrant is assigned a score of 0–2, where 0 = no involvement; 1 = medium/moderate involvement (0–50% of the lung parenchyma); and 2 = severe impairment (>50% of the parenchyma). Maximum score of 8. This example would be scored as follows: right upper quadrant = 1; right lower quadrant = 2; left upper quadrant = 1; left lower quadrant = 1. Total score = 5/8. This study found that scores averaging 4.4 ± 1.9 and bilateral involvement were associated with critical illness.
Some studies have reported higher severity scores in patients who died with COVID-19 compared to those who were discharged from hospital33 and an association between, on the one hand, serious lung disease and, on the other, specific age groups and sex.34
For the moment, international organisations have not recommended using any of the existing systems systematically.
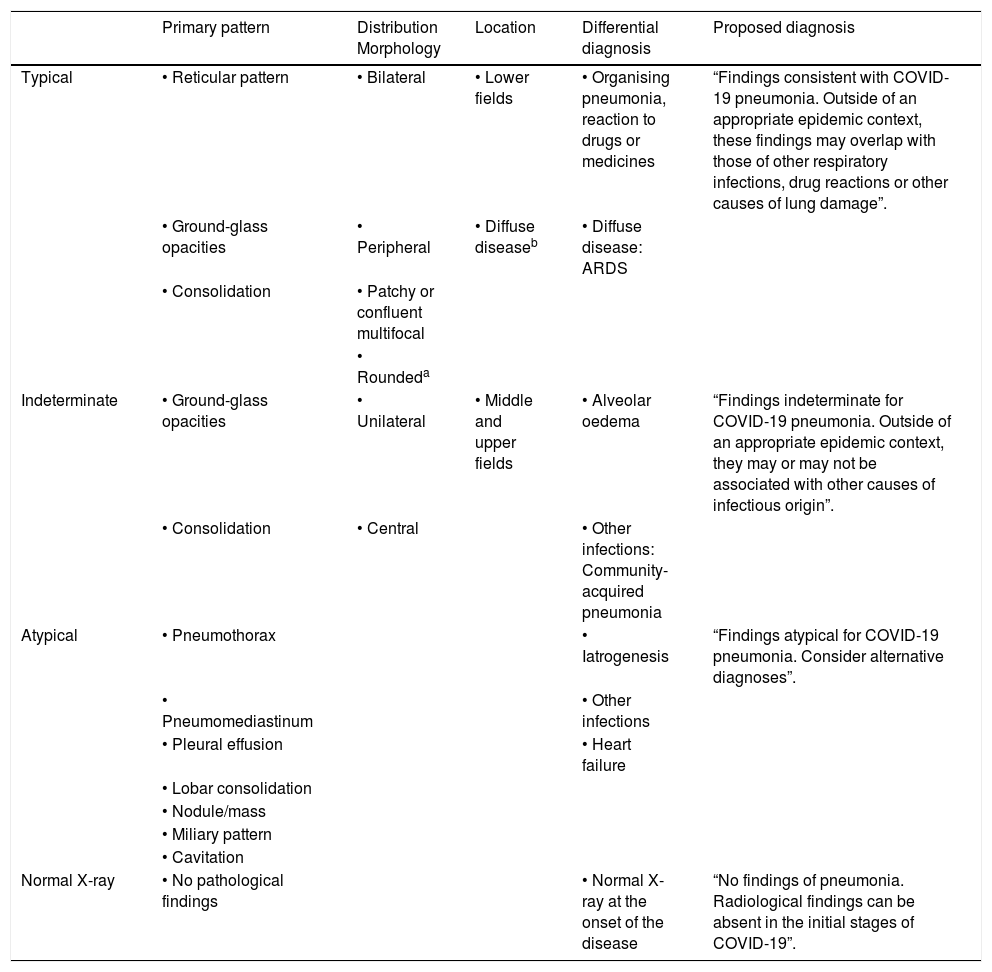
Radiology reportThe large volume of chest X-rays taken during the COVID-19 pandemic requiring a radiology report has represented a challenge for diagnostic imaging departments. Many of these reports have been prepared with no PCR results and scant clinical information.30 This, added to the lack of standardised nomenclature and guidelines, has led to a substantial lack of uniformity among radiological reports. A structured report provides the tools to confidently report findings suggestive of COVID-19, improves communication with ordering physicians, improves patient management and facilitates further analysis for scientific studies.
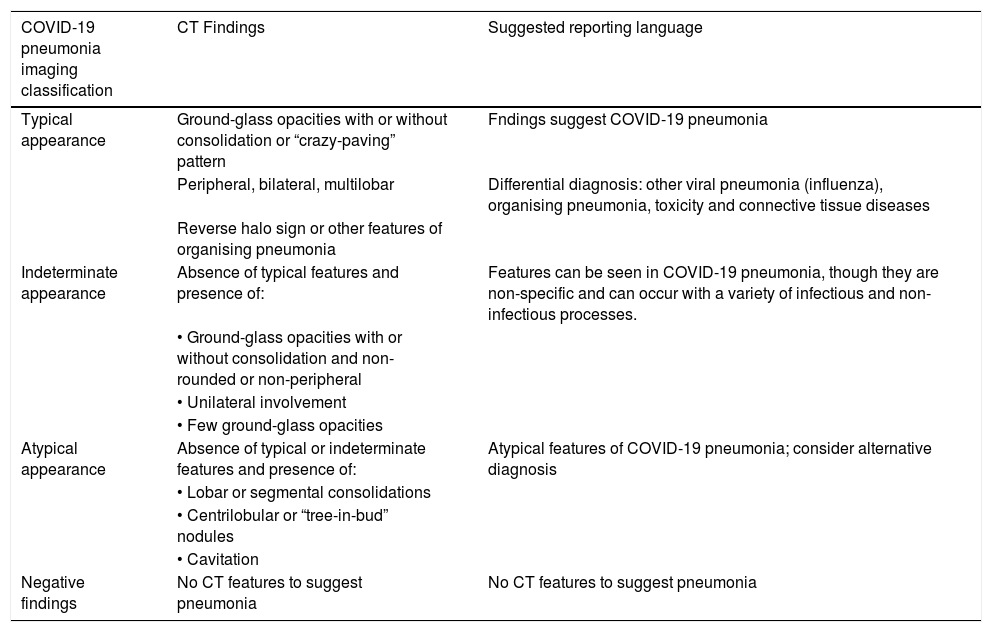
Some publications have proposed standardised language classifying findings as typical, indeterminate, atypical or negative, and conclude that classification should be rooted in the context of the prevalence of COVID-19 and the risk factors of the patient30 (Table 1).
Classification of COVID-19 findings on chest X-ray. The diagnosis proposed in the final column is based on an article by Litmanovich et al.30
| Primary pattern | Distribution Morphology | Location | Differential diagnosis | Proposed diagnosis | |
|---|---|---|---|---|---|
| Typical | • Reticular pattern | • Bilateral | • Lower fields | • Organising pneumonia, reaction to drugs or medicines | “Findings consistent with COVID-19 pneumonia. Outside of an appropriate epidemic context, these findings may overlap with those of other respiratory infections, drug reactions or other causes of lung damage”. |
| • Ground-glass opacities | • Peripheral | • Diffuse diseaseb | • Diffuse disease: ARDS | ||
| • Consolidation | • Patchy or confluent multifocal | ||||
| • Roundeda | |||||
| Indeterminate | • Ground-glass opacities | • Unilateral | • Middle and upper fields | • Alveolar oedema | “Findings indeterminate for COVID-19 pneumonia. Outside of an appropriate epidemic context, they may or may not be associated with other causes of infectious origin”. |
| • Consolidation | • Central | • Other infections: Community-acquired pneumonia | |||
| Atypical | • Pneumothorax | • Iatrogenesis | “Findings atypical for COVID-19 pneumonia. Consider alternative diagnoses”. | ||
| • Pneumomediastinum | • Other infections | ||||
| • Pleural effusion | • Heart failure | ||||
| • Lobar consolidation | |||||
| • Nodule/mass | |||||
| • Miliary pattern | |||||
| • Cavitation | |||||
| Normal X-ray | • No pathological findings | • Normal X-ray at the onset of the disease | “No findings of pneumonia. Radiological findings can be absent in the initial stages of COVID-19”. |
ARDS: acute respiratory distress syndrome.
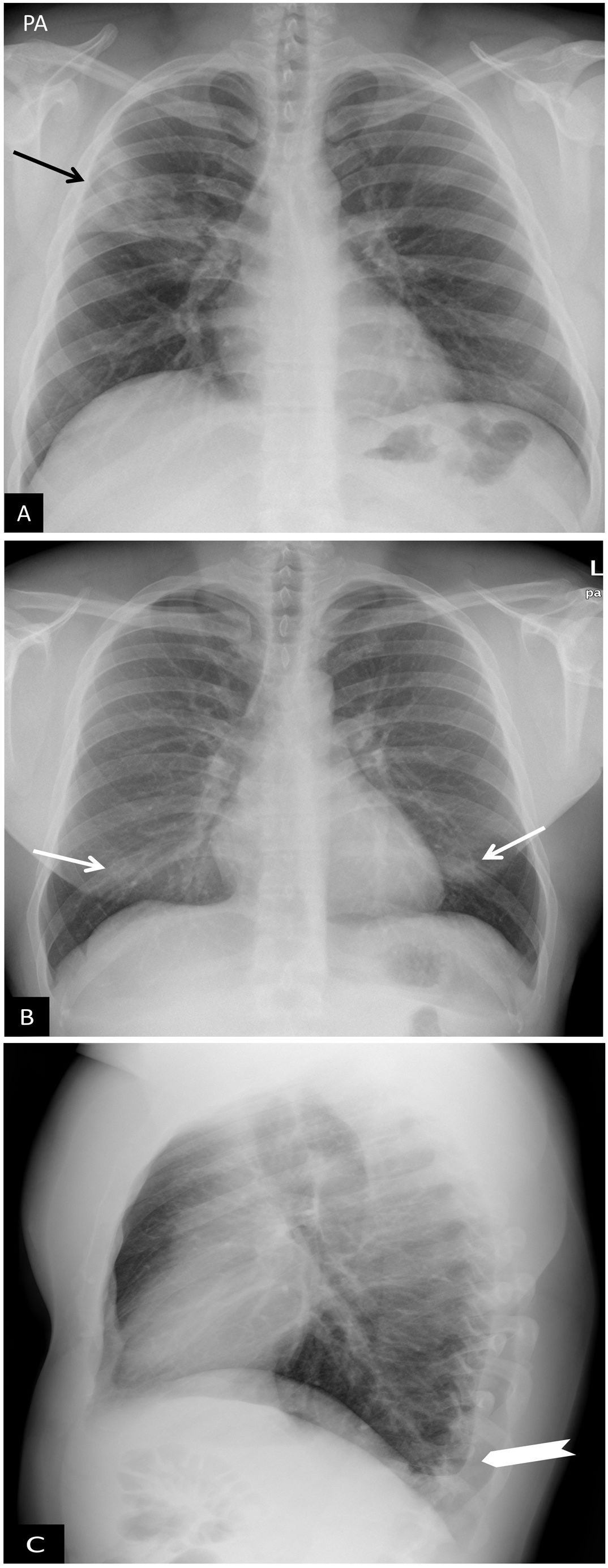
Digital chest tomosynthesis is a technique that uses X-rays in projections with different angles to gather information from different lung sections. This avoids overlapping structures and enables more precise detection of small pulmonary lesions that cannot be visualised on conventional chest X-ray37 (Fig. 5). A series of approximately 50 reconstructed images is obtained with a radiation dose less than twice that of a conventional chest X-ray. Although there are not yet any published studies in patients with COVID-19, the preliminary results of ongoing studies suggest that digital chest tomosynthesis improves sensitivity and specificity in detecting small lung consolidations, as already reported in other lesions.37
Tomosynthesis. A 30-year-old woman with COVID-19. (A) Conventional posteroanterior chest projection. Bilateral opacities in lower fields (arrows) that could correspond to dense breast tissue. Owing to uncertainties around the right hemithorax (arrows), a decision was made to perform a digital tomosynthesis (DT) study. (B and C) DT images. These show extensive consolidation in the right lower lung field (white circle in B), as well as small contralateral consolidations only visualised on DT (arrow tip in C) corresponding to foci of pneumonia.
Reproduced courtesy of Dr J. Plasencia of Hospital General Universitario Morales Meseguer [Morales Meseguer University General Hospital] in Murcia, Spain.
High-resolution chest CT is a quick, accessible test considered to be the most sensitive imaging test for detecting COVID-19, with a reported sensitivity of up to 97%.38 Some studies have found that chest CT findings may precede positive RT-PCR results.38,39
There are disagreements and debates regarding the use of CT as a diagnostic modality since, despite its high sensitivity, it has low specificity (25%), given that COVID-19 findings overlap with findings in other viral infections such as H1N1 influenza, severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS). For this reason, most associations, such as the ACR, consider CT a second-line technique.40 Other associations with PCR testing limitations, such as the Chinese association, use CT as the initial diagnostic modality. They justify it by its higher sensitivity compared to chest X-ray and its lower likelihood of false negatives, especially in early-stage disease.24,38,41
The choice of CT or X-ray in the initial diagnosis of the patient must be made taking into account the attributes of each technique and the resources available at each hospital.25
Indications as a diagnostic testCT is especially useful for guiding management in complex settings, in patients with clinical worsening, and for ruling out alternative diagnoses.
The Sociedad Española de Radiología Médica [Spanish Association of Medical Radiology] (SERAM) recommends its use in the following situations:42
- •
Clinical/analytical/radiological discrepancy: severely ill patients with strong clinical or laboratory suspicion, normal chest X-ray and difficulty to obtain PCR results or negative/inconclusive PCR results.
- •
Patients with confirmed COVID-19 and clinical worsening and/or laboratory results raising suspicion of pulmonary embolism, superinfection or onset of pleural effusion.
- •
Severely ill patients clinically suspected of having COVID-19 for whom a decision must be made as to whether they should be placed in a conventional (clean) ICU or isolation ICU (for COVID-19 patients).
- •
Patients with another critical disease, suspected of having or tentatively diagnosed with COVID-19, who require immediate decision-making with regard to treatment and, therefore, a rapid diagnosis to increase the protection of the professionals involved (surgery, interventional techniques).
For suspicion and initial assessment of COVID-19 with CT, most authors recommend performing a chest study in inspiration without intravenous contrast.43–45 Since many patients present dyspnoea or cough, it is advisable to use faster rotation times (≤0.5 sec) and higher pitch values (>1:1) to prevent motion artefacts.45
Patients with COVID-19 may require multiple studies in short periods of time, leading to an increase in cumulative radiation that must be taken into account, especially in the most sensitive populations.46,47 The use of low-dose protocols with iterative reconstruction has been proposed to reduce radiation exposure. Such protocols have demonstrated comparable efficacy to conventional CT in detecting ground-glass opacities and consolidations,46–48 though further research evaluating their diagnostic accuracy and image quality in the earliest stages of the infection is required.46
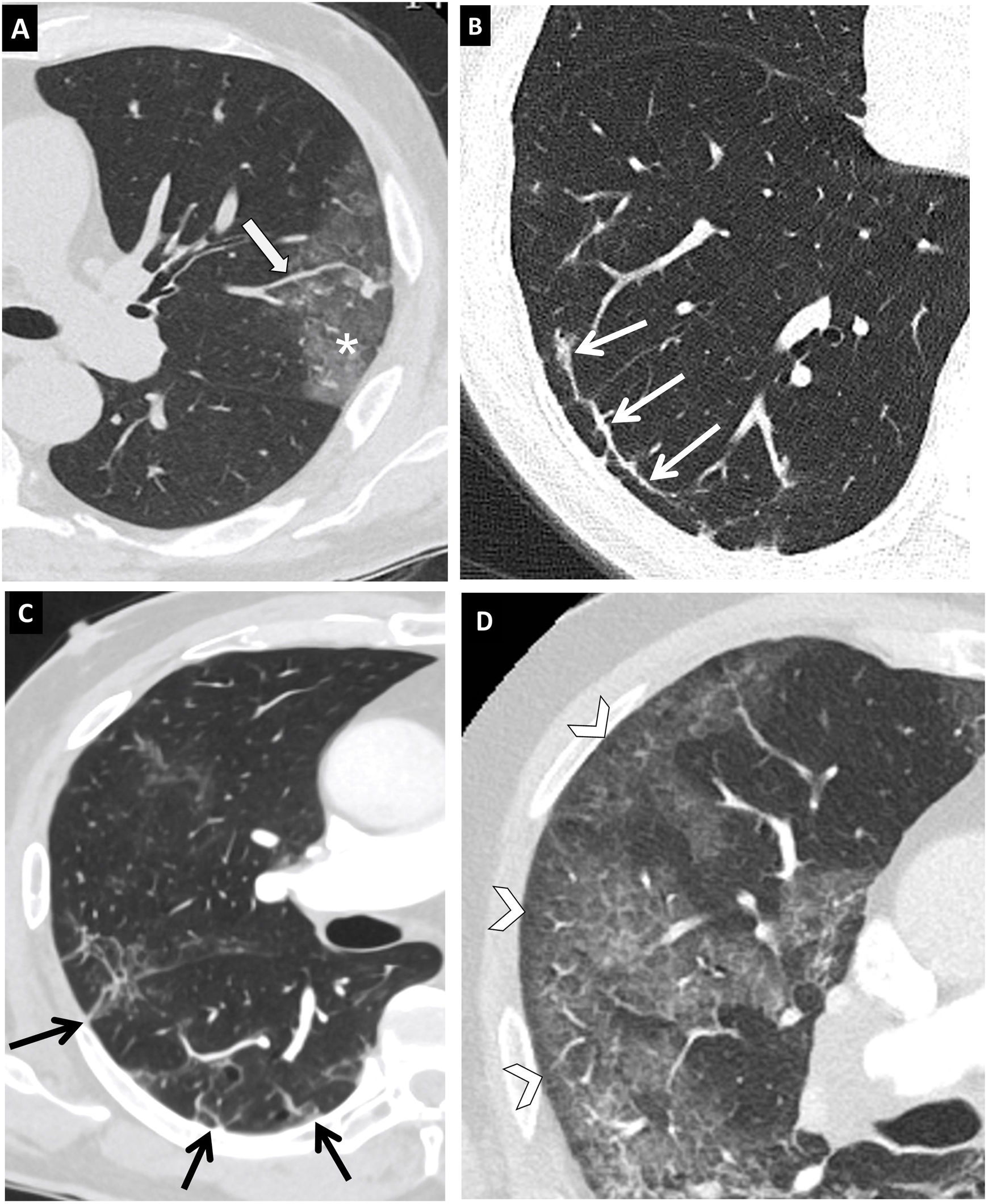
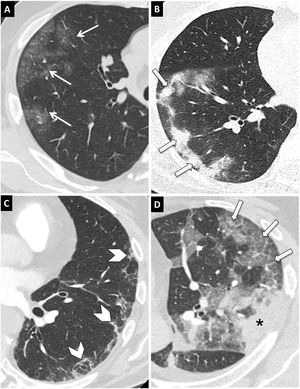
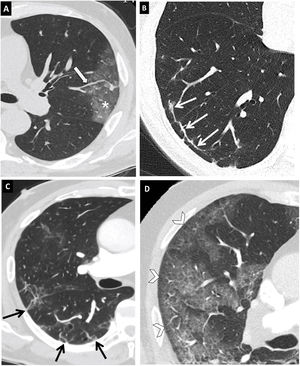
CT findings in patients with COVID-19Typical findings- •
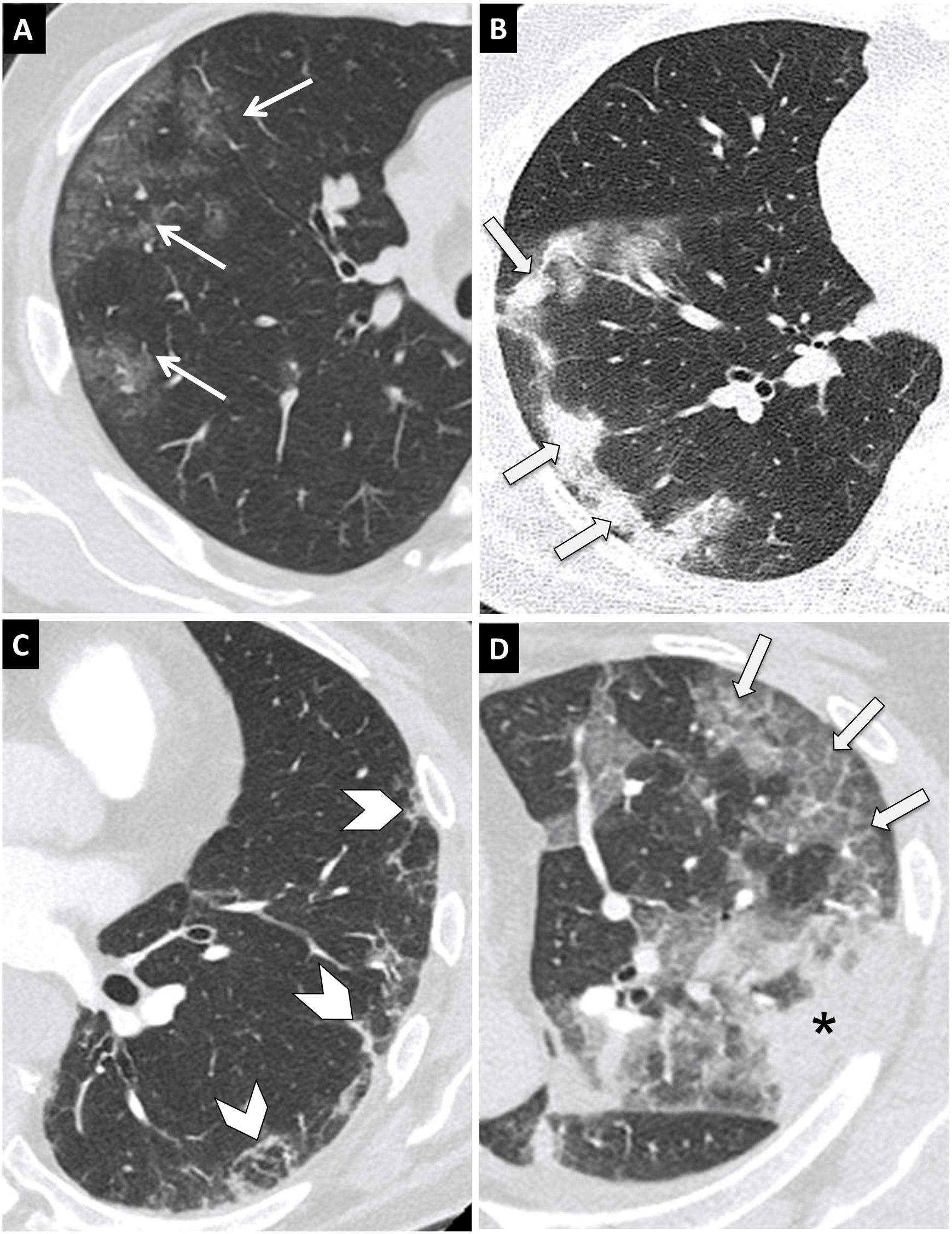
Ground-glass opacities (Fig. 6A): these consist of a slight increase in lung attenuation such that the lungs are semi-transparent without obscuring underlying vascular structures. It is the predominant finding regardless of disease stage, and the earliest.49
Figure 6.Typical findings in COVID-19 pneumonia on computed tomography (CT). Axial chest CT images with 1-mm slices. (A) Ground-glass opacities with rounded morphology and a peripheral and subpleural distribution (arrows). (B) Consolidations with a peripheral and subpleural predominance (arrows). (C) Reticulation with a peripheral and subpleural location (arrow tips). (D) Peripheral ground-glass opacities with overlapping interlobular and intralobular septal thickening in relation to a crazy-paving pattern (arrow). Peripheral consolidation (asterisk) is also seen.
(0.41MB). - •
Consolidation (Fig. 6B): this consists of an increase in lung attenuation that obscures vessels and airway walls. Consolidations represent the second most common pattern and appear in association with ground-glass opacities (44%) or, less frequently, alone (24%).50 They are indicative of disease progression.
- •
Peripheral reticulation (Fig. 6C) due to thickening of interlobular and intralobular septa. It increases with a prolonged disease course.50
- •
Crazy-paving pattern (Fig. 6D): linear pattern due to thickening of interlobular septa overlapping with an underlying ground-glass pattern. It is due to alveolar oedema and acute interstitial inflammation. It is a sign of disease progression.49
Other less common signs:
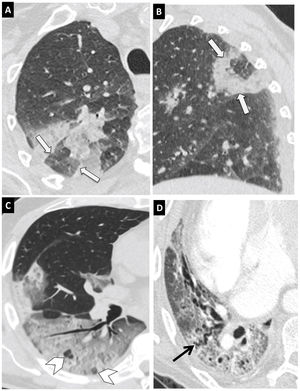
- •
Reversed-halo sign (Fig. 7A and B): this represents a central ground-glass opacity surrounded by a crescent- or ring-shaped consolidation. It is unclear whether it reflects consolidation improvement or glass-ground progression. Although it is not a common finding, it is considered to be among the typical findings.40,49,51
Figure 7.Typical findings in COVID-19 pneumonia on computed tomography (CT). Images from a CT scan of the chest with 1-mm slices. (A and B) Axial (A) and sagittal (B) images showing a lesion in the posterior segment of the right upper lobe with the reversed-halo sign (arrows). (C) Extensive ground-glass involvement with areas of consolidation in the right lower lobe with the vacuolar sign (arrow tips). (D) Abnormal architecture of the right lower lobe with a crazy-paving pattern and bronchial dilation (black arrow).
(0.4MB). - •
Air-bubble (vacuolar) sign (Fig. 7C): this refers to a small hypodense pulmonary space, less than 5 mm, within the ground-glass opacity. It could correspond to pathological dilation of a normal space or a cross-section of bronchiolectasis, or it could be secondary to the resolution of consolidations.50
- •
Airway changes, with bronchial dilations (Fig. 7D) in ground-glass areas and bronchial wall thickening due to inflammation.
- •
Prominent vessels: dilation of the perilesional or intralesional pulmonary vessels (Fig. 8A) due to capillary wall damage in response to inflammatory factors.49
Figure 8.Typical findings in COVID-19 pneumonia on computed tomography (CT). Axial chest CT images with 1-mm slices. (A) Vascular thickening (arrow) associated with an area of ground-glass opacity (asterisk). (B) Subpleural curvilinear line (arrow). (C) Subpleural parenchymal bands (arrows). (D) Hypoattenuating line (arrows) between visceral pleura and ground-glass opacity (arrow tips).
(0.38MB). - •
Pleural and subpleural abnormalities:
- –
Pleural thickening associated with lung parenchyma abnormalities.
- –
Subpleural curvilinear line (Fig. 8B): thin curvilinear opacity, with a thickness of 1–3 mm, parallel to the pleura and less than 1 cm from the pleural surface. It is related to oedema or fibrosis.52
- –
Subpleural parenchymal band (Fig. 8C): linear opacity, usually 1–3 mm thick and up to 5 cm long, perpendicular and usually extending to the visceral pleura. It is often thickened and retracted at the point of contact with the visceral pleura. It reflects parenchymal fibrosis and is usually associated with distorted lung architecture.
- –
A hypoattenuating line between the visceral pleura and the lesion (Fig. 8D).
- –
Pleural effusion, pericardial effusion, lymphadenopathy, cystic changes and pneumothorax are among the rare but possible findings seen with disease progression,53,54 generally associated with severe illness.
Location and distributionInvolvement is usually multifocal and bilateral, with a peripheral and subpleural distribution.54 There may be unilateral ground-glass opacities, primarily in early-stage disease.55 Although all lung segments may be involved, there is a predilection for the lower lobes.50
None of the findings reported are unique to COVID-19 pneumonia, but the typical distribution and combination thereof in the epidemic context are strongly suggestive of its diagnosis.
Indeterminate findingsThese are non-specific forms of presentation, since they may be seen both in COVID-19 pneumonia and in pneumonia caused by other pathogens, and even in non-infectious diseases:
- •
Non-peripheral (central or peribronchovascular) patchy ground-glass consolidations or opacities, with a unilateral distribution, more common in the upper lobes.
- •
Ground-glass fibrosis.
- •
Lymphadenopathy.
- •
Pleural effusion.
- •
Cavitation.
- •
Calcification.
- •
Well-defined solid nodules or masses.
- •
Bronchiolitis—tree-in-bud pattern.
- •
Focal consolidation.
- •
Diffuse ground-glass opacities with a peribronchovascular distribution.
- •
Fibrotic changes (honeycombing and traction bronchiectasis).
These findings point to an alternative diagnosis.53
CT findings according to the evolutionary stage of infectionSome studies have reported abnormal findings on pulmonary CT in asymptomatic patients.55 There have also been reports of negative CT results during the first few days of symptoms. Therefore, negative CT results should not be used to rule out the possibility of COVID-19, particularly in early-stage disease.
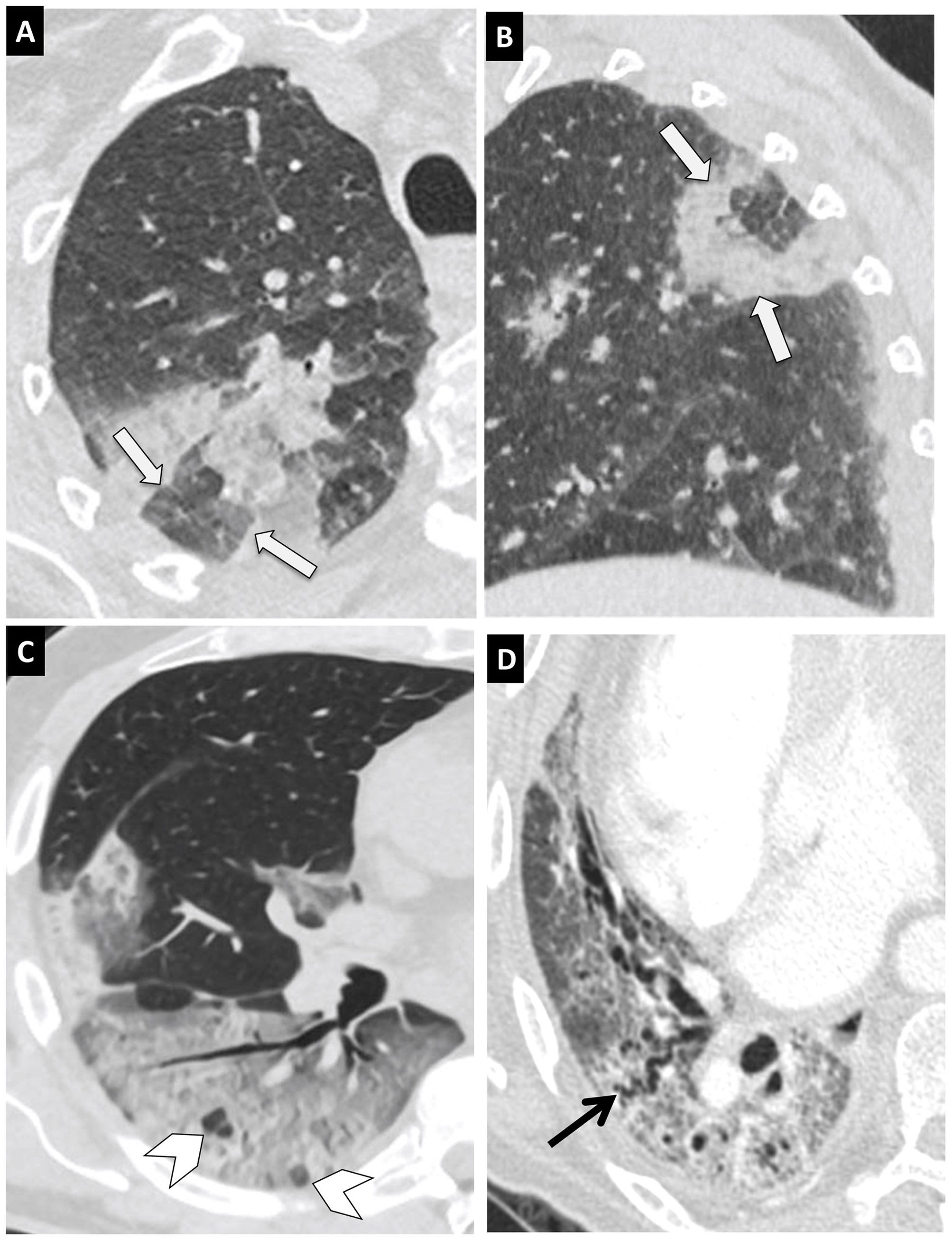
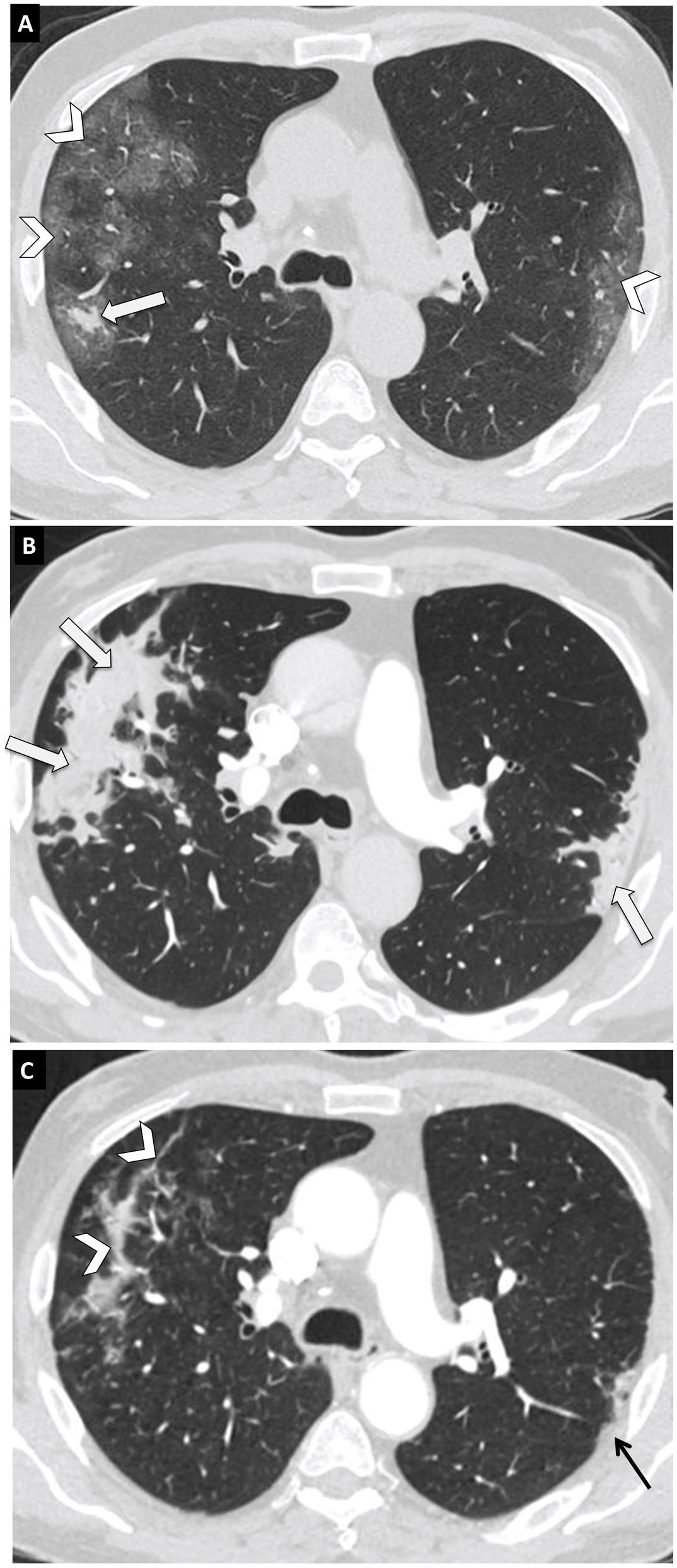
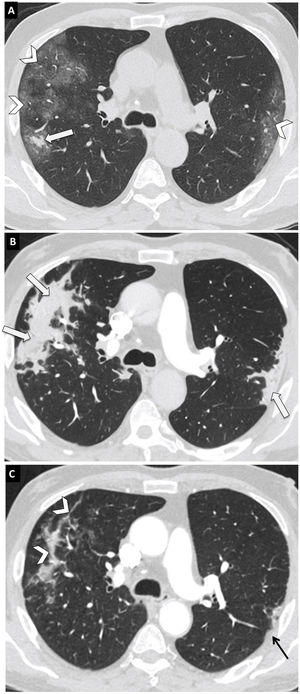
There is a link between radiological findings and time elapsed since the onset of symptoms51,56,57 (Fig. 9). Four evolutionary stages have been reported:
- 1
Early phase (0–4 days after the onset of symptoms): the ground-glass pattern predominates, with unilateral or bilateral and multifocal involvement. It can show a rounded morphology. CT can also be normal (50% in the first two days).
- 2
Progression phase (5–8 days): involvement with a ground-glass pattern progresses rapidly in extent and becomes bilateral and diffuse, with multilobar involvement. In this stage, areas of crazy-paving pattern and consolidations may appear.53
- 3
Peak phase (9–13 days): maximum involvement is seen, with areas of ground-glass pattern transforming into consolidation. Consolidation is the predominant form of involvement. An air bronchogram, crazy-paving pattern and reversed-halo sign may be seen.
- 4
Resolution phase (>14 days): resorption of consolidations manifests again as ground-glass opacities that may be associated with bronchial dilations with subpleural distortion. Both subpleural parenchymal bands and subpleural curved lines might appear. The evolution of the lesions is often asynchronous, with some areas showing resorption and others showing progression.
Progression of COVID-19 pneumonia in a 56-year-old woman. Axial chest computed tomography (CT) images with a thickness of 1 mm at the level of the carina. (A) Study 10 days after the onset of symptoms. Peripheral and bilateral ground-glass opacities (arrow tips) and a small consolidation forming in the posterior segment of the right upper lobe (arrow). (B) CT scan 15 days after the first CT scan. Progression of ground-glass opacities to consolidations (arrows). (C) CT scan 32 days after the first CT scan. Partial resorption of consolidations (arrow tips) and focal pleural thickening in the apicoposterior segment of the left upper lobe (black arrow).
In some patients, interlobular and intralobular septal thickening associated with bronchial dilations gradually increases from the second week. These findings are indicative of interstitial disease, suggesting the development of fibrosis, although the course of the disease is not yet sufficiently understood to classify these changes as irreversible fibrosis.53
Structured reportA structured report offers a standardised language that can be understood by the entire medical community. It must be correlated with the clinical suspicion, duration of symptoms and local prevalence.
The Radiological Society of North America (RSNA) proposes four categories for COVID-19 pneumonia—typical, indeterminate, atypical and negative40 (Table 2).
Classification system for findings of COVID-19 pneumonia on chest computed tomography (CT), a consensus endorsed by the American College of Radiology (ACR) and the Radiological Society of North America (RSNA).40
| COVID-19 pneumonia imaging classification | CT Findings | Suggested reporting language |
|---|---|---|
| Typical appearance | Ground-glass opacities with or without consolidation or “crazy-paving” pattern | Fndings suggest COVID-19 pneumonia |
| Peripheral, bilateral, multilobar | Differential diagnosis: other viral pneumonia (influenza), organising pneumonia, toxicity and connective tissue diseases | |
| Reverse halo sign or other features of organising pneumonia | ||
| Indeterminate appearance | Absence of typical features and presence of: | Features can be seen in COVID-19 pneumonia, though they are non-specific and can occur with a variety of infectious and non-infectious processes. |
| • Ground-glass opacities with or without consolidation and non-rounded or non-peripheral | ||
| • Unilateral involvement | ||
| • Few ground-glass opacities | ||
| Atypical appearance | Absence of typical or indeterminate features and presence of: | Atypical features of COVID-19 pneumonia; consider alternative diagnosis |
| • Lobar or segmental consolidations | ||
| • Centrilobular or “tree-in-bud” nodules | ||
| • Cavitation | ||
| Negative findings | No CT features to suggest pneumonia | No CT features to suggest pneumonia |
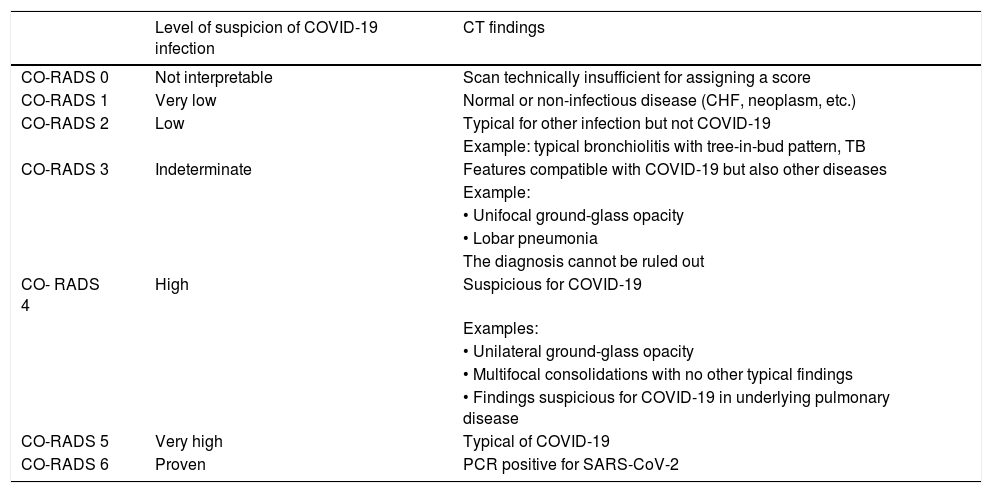
The Nederlandse Vereniging voor Radiologie [Dutch Association of Radiology] proposes a consensus for the structured reporting of findings on chest CT in patients with suspected COVID-19. This association developed the CO-RADS classification, with a five-point scale for suspicion, from very low (CO-RADS 1) to very high (CO-RADS 5), for patients with moderate to severe symptoms in a setting of moderate to high prevalence58 (Table 3).
CO-RADS classification of the COVID Working Group of the Dutch Radiology Society: proposed standardised CT reporting system for patients with suspected COVID-19 in a setting of moderate to high prevalence.58
| Level of suspicion of COVID-19 infection | CT findings | |
|---|---|---|
| CO-RADS 0 | Not interpretable | Scan technically insufficient for assigning a score |
| CO-RADS 1 | Very low | Normal or non-infectious disease (CHF, neoplasm, etc.) |
| CO-RADS 2 | Low | Typical for other infection but not COVID-19 |
| Example: typical bronchiolitis with tree-in-bud pattern, TB | ||
| CO-RADS 3 | Indeterminate | Features compatible with COVID-19 but also other diseases |
| Example: | ||
| • Unifocal ground-glass opacity | ||
| • Lobar pneumonia | ||
| The diagnosis cannot be ruled out | ||
| CO- RADS 4 | High | Suspicious for COVID-19 |
| Examples: | ||
| • Unilateral ground-glass opacity | ||
| • Multifocal consolidations with no other typical findings | ||
| • Findings suspicious for COVID-19 in underlying pulmonary disease | ||
| CO-RADS 5 | Very high | Typical of COVID-19 |
| CO-RADS 6 | Proven | PCR positive for SARS-CoV-2 |
CHF: congestive heart failure; CT: computed tomography; PCR: polymerase chain reaction; TB: tuberculosis.
Most patients infected with SARS-CoV-2 have mild symptoms and a good prognosis. However, sometimes the virus causes severe disease in the form of pneumonia, pulmonary oedema, ARDS or multiple organ failure that can lead to death. The study of clinical, laboratory and imaging factors associated with disease severity is key to promoting effective treatment strategies that reduce complications and mortality.59
Chest CT is considered one of the main tools for assessing infection severity.59–64 It enables stratification of patients into risk categories and estimation of their prognosis, thus aiding in clinical decision-making.64
The imaging finding most commonly associated with clinical severity is the extent of lung involvement.52,55,59,60,62,63,65–70
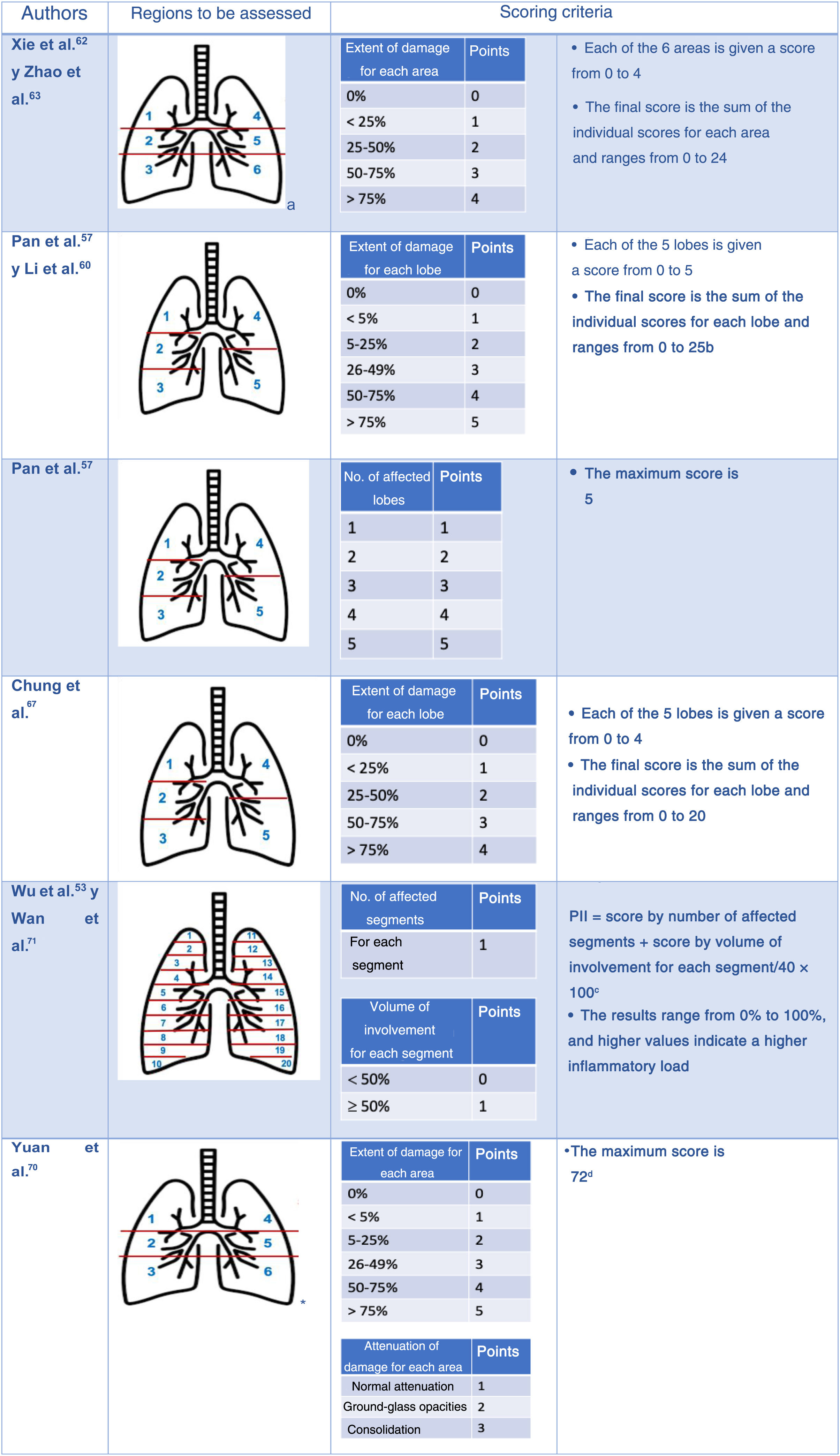
Multiple semi-quantitative scales have been proposed for CT that visually calculate the extent of the abnormalities (Fig. 10). Their disadvantage is their lack of precision. To address this shortcoming, artificial intelligence systems can perform a rigorous quantitative analysis of injured lung volume.71–73
Semi-quantitative scales to assess the extent of lung lesions due to COVID-19 pneumonia with computed tomography.
aUpper regions (1 and 4) above carina; middle regions (2 and 5) between carina and inferior pulmonary vein; lower regions (3 and 6) below inferior pulmonary vein.
bLi et al.59 showed that the classification with a cut-off point of 7 had a sensitivity of 80% and a specificity of 82.8% for distinguishing between severely and mildly ill patients (area under the curve [AUC] 0.87).
cWu et al.52 demonstrated that the pulmonary inflammation index (PII) is an independent indicator of disease progression and severity. The Chongqing Radiology Association of China uses it as an evaluation criterion.
dWith a cut-off point of 24.5, the scale predicts mortality with a sensitivity of 85% and a specificity of 84%.
Other significantly more common pulmonary abnormalities in patients with severe disease are diffuse distribution of lesions,55,62,66,67,69 involvement of middle and central areas,55,60,65 consolidations,59,64,67,69 crazy-paving pattern,59,67 interlobular septal thickening,67 bronchial wall thickening,59 air bronchogram,69 traction bronchiectasis,62 linear opacities,59 atelectasis64 and distorted lung architecture.62 Extrapulmonary lesions such as intrathoracic lymph node enlargement59,62 and pleural and pericardial (60) effusion59,62,64 also appear to be associated with more severe disease (Fig. 10).
Clinical correlation and pathology findingsThe “Guidelines for the Diagnosis and Treatment of Novel Coronavirus (2019-nCoV) Infection by the [Chinese] National Health Commission (Trial Version 5)” clinically distinguishes four levels of severity:74
- 1
Mild. Patients with mild symptoms and no abnormalities on CT. The virus is located in the upper respiratory tract and has not reached the alveoli, so there is no pulmonary reaction.75
- 2
Common. Patients with fever or signs of respiratory infection and pneumonia changes on CT. They usually present areas of ground-glass attenuation representing partial occupation of the alveolar spaces by exudate. The alveolar wall is intact.52,67,75
- 3
Severe. Patients meeting at least one of the following criteria:
- •
Respiratory distress, respiratory rate ≥30/min.
- •
Finger oxygen saturation (SaO2) 93% at rest.
- •
Partial pressure of oxygen (PaO2)/fraction of inspired oxygen (FiO2) 300 mmHg.
CT may show a crazy-paving pattern. According to Wang et al.,67 70% of patients with this abnormality will be classified as severely or critically ill. It is caused by an alveolar pattern plus an interstitial pattern. It reflects an increase in alveolar exudate and dilation with increased permeability of the capillaries of the interlobular septa, leading to interlobular interstitial oedema.67,75
- 4
Critical. Patients meeting at least one of the following criteria:
- •
Respiratory failure requiring mechanical ventilation.
- •
Shock.
- •
Multiple organ failure.
On CT they present extensive diffuse consolidations that may have a “white-out” appearance.55,75 They are caused by alveolar injury with accumulation of exudates and oedema in the alveolar cavity leading to a ventilation-perfusion defect. This, added to an abnormal immune reaction (immune dysregulation), ends up causing ARDS and a severe systemic clinical picture.52,64,75
COVID-19 in pregnant womenPregnancy does not appear to increase susceptibility to SARS-CoV-2 infection. However, pregnant women are at higher risk of severe disease, and those who develop pneumonia are at higher risk of preterm delivery and caesarean birth.76
A chest X-ray, usually the PA projection, is sufficient for initial evaluation of pulmonary complications in most pregnant patients. A single chest X-ray carries a very low fetal radiation dose (0.0005–0.01 mGy).77 If indicated, CT should be performed, because the fetal radiation dose is low (0.01–0.66 mGy) and not associated with an increased risk of fetal abnormalities or pregnancy loss.77
ConclusionImaging tests play an important role in the management of patients with suspected or confirmed COVID-19. The initial imaging test is the chest X-ray. CT, which is more sensitive, is reserved for detecting possible complications and providing alternative diagnoses, in cases of clinical, analytical and radiological discrepancy or when microbiological diagnosis is not possible.
COVID-19 pneumonia is characterised by the presence of ground-glass opacities and/or consolidations, which are typically bilateral and peripheral, often subpleural and more commonly in the lower fields. As regards clinical course, reparative changes appear from the second week of the disease, characterised by subpleural lines, greater subpleural distortion and bronchial dilations.
In addition, imaging tests enable monitoring of the course of the disease and grading of the severity of lung involvement.
AuthorshipResponsible for the integrity of the study: EMC, ADT, LIS, SOV, SBN.
Study conception: EMC, ADT, LIS, SOV, SBN.
Study design: EMC, ADT, LIS, SOV, SBN.
Data collection: EMC, ADT, LIS, SOV, SBN.
Data analysis and interpretation: EMC, ADT, LIS, SOV, SBN.
Statistical processing: N/A.
Literature search: N/A.
Drafting of the manuscript: EMC, ADT, LIS, SOV, SBN.
Critical review of the manuscript with intellectually significant contributions: EMC, ADT, LIS, SOV, SBN.
Approval of the final version: EMC, ADT, LIS, SOV, SBN.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Martínez Chamorro E, Díez Tascón A, Ibáñez Sanz L, Ossaba Vélez S, Borruel Nacenta S. Diagnóstico radiológico del paciente con COVID-19. Radiología. 2021;63:56–73.




![Tomosynthesis. A 30-year-old woman with COVID-19. (A) Conventional posteroanterior chest projection. Bilateral opacities in lower fields (arrows) that could correspond to dense breast tissue. Owing to uncertainties around the right hemithorax (arrows), a decision was made to perform a digital tomosynthesis (DT) study. (B and C) DT images. These show extensive consolidation in the right lower lung field (white circle in B), as well as small contralateral consolidations only visualised on DT (arrow tip in C) corresponding to foci of pneumonia. Reproduced courtesy of Dr J. Plasencia of Hospital General Universitario Morales Meseguer [Morales Meseguer University General Hospital] in Murcia, Spain. Tomosynthesis. A 30-year-old woman with COVID-19. (A) Conventional posteroanterior chest projection. Bilateral opacities in lower fields (arrows) that could correspond to dense breast tissue. Owing to uncertainties around the right hemithorax (arrows), a decision was made to perform a digital tomosynthesis (DT) study. (B and C) DT images. These show extensive consolidation in the right lower lung field (white circle in B), as well as small contralateral consolidations only visualised on DT (arrow tip in C) corresponding to foci of pneumonia. Reproduced courtesy of Dr J. Plasencia of Hospital General Universitario Morales Meseguer [Morales Meseguer University General Hospital] in Murcia, Spain.](https://static.elsevier.es/multimedia/21735107/0000006300000001/v1_202101300735/S2173510721000033/v1_202101300735/en/main.assets/thumbnail/gr5.jpeg?xkr=ue/ImdikoIMrsJoerZ+w96p5LBcBpyJTqfwgorxm+Ow=)
![Semi-quantitative scales to assess the extent of lung lesions due to COVID-19 pneumonia with computed tomography. aUpper regions (1 and 4) above carina; middle regions (2 and 5) between carina and inferior pulmonary vein; lower regions (3 and 6) below inferior pulmonary vein. bLi et al.59 showed that the classification with a cut-off point of 7 had a sensitivity of 80% and a specificity of 82.8% for distinguishing between severely and mildly ill patients (area under the curve [AUC] 0.87). cWu et al.52 demonstrated that the pulmonary inflammation index (PII) is an independent indicator of disease progression and severity. The Chongqing Radiology Association of China uses it as an evaluation criterion. dWith a cut-off point of 24.5, the scale predicts mortality with a sensitivity of 85% and a specificity of 84%. Semi-quantitative scales to assess the extent of lung lesions due to COVID-19 pneumonia with computed tomography. aUpper regions (1 and 4) above carina; middle regions (2 and 5) between carina and inferior pulmonary vein; lower regions (3 and 6) below inferior pulmonary vein. bLi et al.59 showed that the classification with a cut-off point of 7 had a sensitivity of 80% and a specificity of 82.8% for distinguishing between severely and mildly ill patients (area under the curve [AUC] 0.87). cWu et al.52 demonstrated that the pulmonary inflammation index (PII) is an independent indicator of disease progression and severity. The Chongqing Radiology Association of China uses it as an evaluation criterion. dWith a cut-off point of 24.5, the scale predicts mortality with a sensitivity of 85% and a specificity of 84%.](https://static.elsevier.es/multimedia/21735107/0000006300000001/v1_202101300735/S2173510721000033/v1_202101300735/en/main.assets/thumbnail/gr10.jpeg?xkr=ue/ImdikoIMrsJoerZ+w96p5LBcBpyJTqfwgorxm+Ow=)

