To detect and graduate endolymphatic hydrops or endolymphatic space dilations in patients with suspected Meniere's disease or immune-mediated inner ear disease by magnetic resonance imaging.
Material and methodsA prospective study was performed including all the patients with clinical suspicion of Meniere's disease or immune-mediated inner ear disease treated at the Otolaryngology department during a one year period. In all cases, magnetic resonance imaging (MRI) was performed in a 3T scanner. IR sequence was performed after 24–28h prior intratimpanic injection of gadolinium on both ears. Two neurorradiologist graduated endolymphatic space volume as agreed on normal, moderate and significant in the obtained images.
ResultsThe presence of hydrops was documented by MRI in six patients with definite or probable Meniere's disease. In two of the four cases without vertigo hydrops was not demonstrated. In the other two cases with a high clinical suspicion of immune-mediated disease but with negative autoimmune tests hydrops was proved. There was only disagreement on cochlear hydrops presence on two patients.
ConclusionThe detection of endolymphatic hydrops in patients with definite or probable Meniere's disease served to confirm the final diagnosis. Moreover, hydrops was detected in patients with suspected immune-mediated inner ear disease, which could have an impact on the diagnosis and treatment of these patients. Therefore, we suggest that this test could be included for the diagnosis of these inner ear diseases.
Detectar la dilatación del espacio endolinfático o hidrops endolinfático (HE) con resonancia magnética (RM) en pacientes con sospecha de enfermedad de Ménière (EM) o enfermedad inmunomediada del oído interno (EIOI).
Material y métodosIncluimos prospectivamente todos los pacientes con sospecha clínica de EM (seis pacientes) o EIOI (cuatro pacientes) atendidos en el servicio de otorrinolaringología en el último año. En todos los casos se realizó una RM con un equipo de 3T y se adquirió una secuencia 3D real IR tras la inyección de gadolinio intratimpánico en ambos oídos 24–28 horas antes. Dos neurorradiólogos graduaron el volumen del espacio endolinfático según convenio en normal, moderado y significativo en las imágenes obtenidas.
ResultadosSe documentó la presencia de HE mediante RM en seis pacientes con EM definida o probable. En dos de los cuatro casos que no presentaban vértigo no se demostró hidrops. En los otros dos casos, con alta sospecha clínica de EIOI, pero con pruebas autoinmunitarias negativas, sí se demostró hidrops. Solo hubo discordancia sobre la presencia de hidrops coclear en dos pacientes.
ConclusiónLa detección de HE en los pacientes con EM definida o probable sirvió para confirmar el diagnóstico definitivo. Por otro lado, se detectó hidrops en pacientes con sospecha de EIOI, lo cual podría tener repercusión sobre el diagnóstico y el tratamiento de estos pacientes. Por ello, habría que valorar la necesidad de incluir esta prueba en el diagnóstico de dichas enfermedades.
Ménière's disease (MD) was reported for the first time in 18611 and it is characterized by recurrent vertiginous attacks, fluctuating hearing loss in deep frequencies, feeling of optical fullness and tinnitus. It is more common in the fouth and fifth decades of life and its incidence ranges between 10 and 157 cases for every 100,000 people. Its etiology is still unknown. With the passing of time ENT (ear, nose and throat) medical societies have reached different consensus for the clinical diagnosis of this condition based on vertiginous attacks and hearing fluctuations confirmed through functional tests. However the dilation of the endolymphatic space or endolymphatic hydrops (EH) at least present in one ear in the post mortem studies conducted on patients diagnosed with MD is suggestive of positive diagnosis of this disease.2–4
On the other hand more recent is the consideration of the autoimmune inner ear disease (AIED) defined as a bilateral sensorineural hearing loss – usually asymmetric and starting at high frequencies, of a sudden onset (days) or rapidly progressing (weeks or months) which in its progression can fluctuate and be accompanied by vertigo which would make it almost clinically undistinguishable from MD but that responds to the administration of immunosuppressant drugs.5
The autoimmune reactions could be the cause of some types of MD.3 Histologic studies and MRIs suggest that there is a relation with EH with mechanisms of autoimmunity: EH has been observed in Cogan's syndrome (prototype of autoimmune disease leading to lesions of the inner ear,6 autoimmune inner ear diseases, post-surgical trauma side effects in patients with cochlear implants, unoperated acoustic neuromes7 and recurring peripheral vestibulopathy.8
During the last years MRI sequences have been conducted in an attempt to see the perilymphatic and endolymphatic spaces separately. These are inversion-recovery sequences that take advantage of the fact the gadolinium does not reach the endolymphatic space but it does reach the perilymphatic space. So after the administration of gadolinium, the median canal (endolymph) can be seen without a signal due to the absence of gadolinium while the vestibular and tympanic ducts (perilymph) can be seen with a signal due to the presence of gadolinium in turn which allows us to establish the degree of EH.9,10 The inversion-recovery sequences used are the 3D FLAIR sequences – the first ones to be implemented and are considered the most sensitive ones to gadolinium in the perilymphatic space and the 3D real IR that shows a greater contrast between the endolymphatic space and the bone.10,11
The route of contrast administration can be intratympanic (24–28 h before conducting the image study) or intravenous (4h before). In the intratympanic route contrast is introduced in the inner ear10 and it reaches the inner ear perilymphatic space through a round or oval window. The patency variability of these windows can constrain the passage of contrast towards the perilymphatic space. We can achieve a greater concentration of contrast in the perilymphatic space through the intratympanic route than through the IV one.12–14
The goal of this study is to analyze the appearance of EH in patients with a clinical diagnosis of MD, and AIED through MRIs and intratympanic gadolinium.
Material and methodsWe conducted a study that prospectively included all patients that in the last year (from October 2015 through March 2016) received medical attention in the ENT unit with a clinical suspicion of MD or AIED. These patients were part of a clinical trial approved by the hospital ethics committee (PI 148-14, Acta 306, 12-01-2015). After fully explaining to each participant the nature, goals and proceedings of the study they all signed a written informed consent.
We gathered 10 patiens with clinical suspicion of MD (six) or AIED (four) with an average age at disease onset of 43.7 years (21–67 years). In the ENT unit all patients received an injection of 0.45–0.9ml of intratympanic contrast (gadoteric acid, Dotarem® 0.5mmol/ml injection vial, Guerbet, Aulnay-sous-Bois, France) with a 1/8 concentration (1ml gadolinium in 7ml of serum) bilaterally after anaesthesia of the tympanic duct and the tympanic membrane.
The examination was conducted 24–48h later using a Philips ACHIEVA 3T machine (Best, The Netherlands) with an 8-channel SENSE antenna and a 3D real IR sequence with repetition time of 6000ms, echo time of 107ms, inversion time of 1650ms, a 180° inversion angle, NSA 1, 1.5×1 SENSE factor, field of vision of 160×160×18mm, voxel size 0.55×0.63×1mm/pixel. The sequence was conducted in the axial plane and lasted 12.42min.
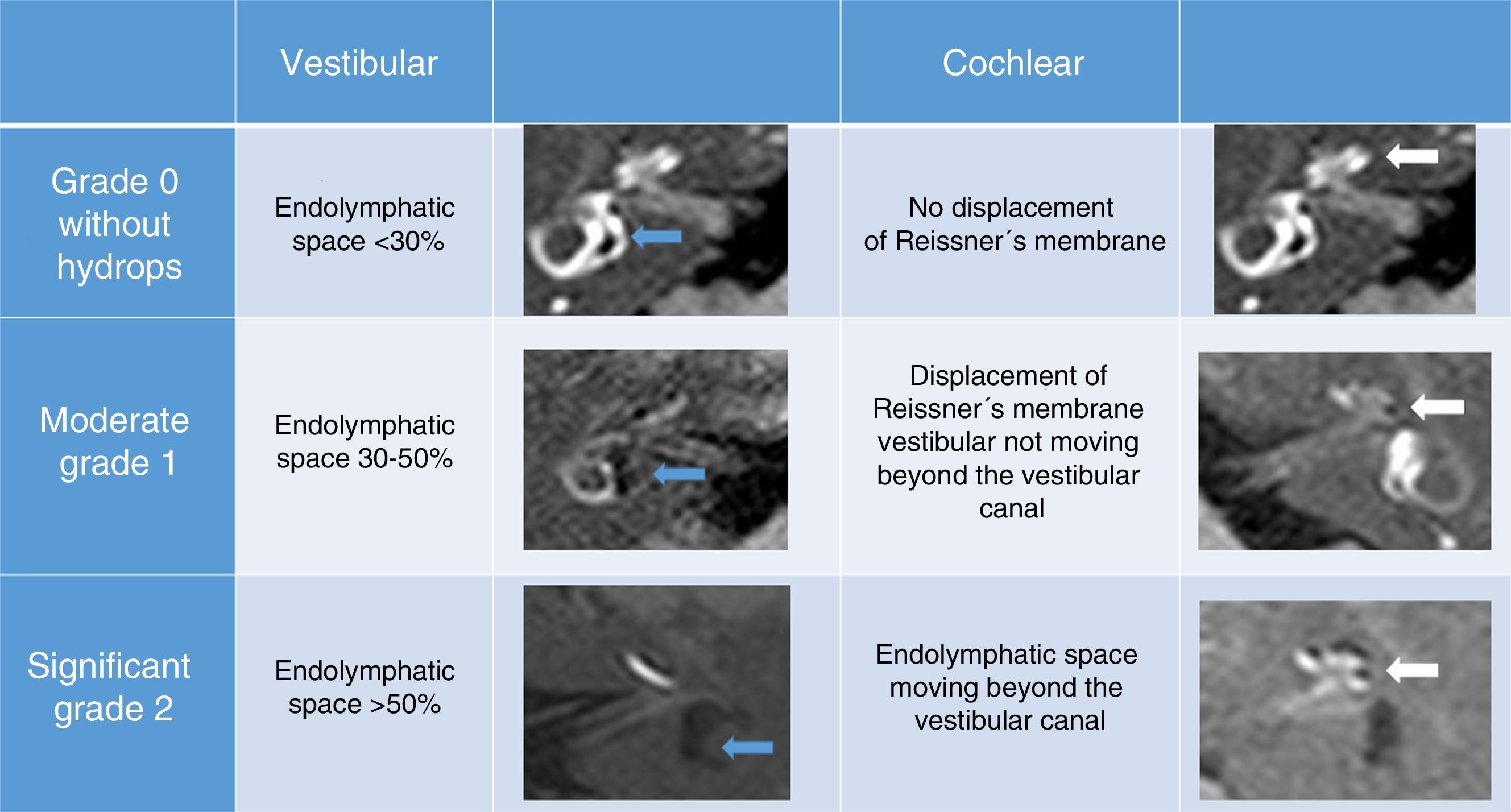
Two radiologists with 6 and 15 years of experience in neuroradiology analyzed the images separately unaware of the symptoms of each patient. The degree of HE was established visually both in the cochlea and the vestibule. As the anatomic reference to measure the vestibular hydrops the axial plane was the chosen one including almost the whole lateral semicirculal duct. Based on Bárath's criteria,9 grade 1 is one hyperintense signal of perilymphatic space around the dilated endolymphatic space in which it is impossible to distinguish between the utriculum and the saculum; grade 2 means that this peripheral signal is not visible. However in those cases where the utriculum and the saculum can be outlined and enhanced separately the volumes were measured by outlining the area free-hand and graded based on the scheme percentages shown in Fig. 1.10 For the assessment of the cochlear hydrops the axial projection was used centered in the mid-modiolar plane in such a way it would allow us to see the cochlear twists and turns, and the cochlear duct in order to be able to establish grades based on the scheme shown in Fig. 1.
Findings were categorized as grade 0 (no hydrops data), grade 1 (moderate grade) and grade 2 (significant grade).
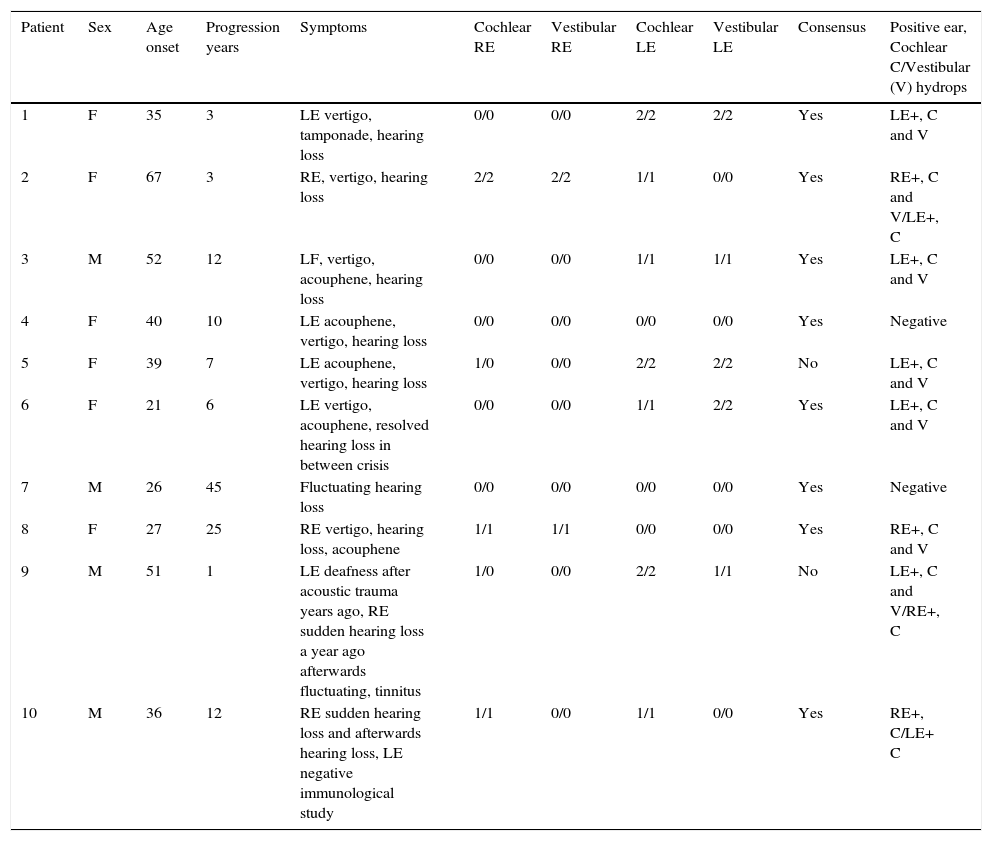
ResultsThe time of clinical progression was 12.4 years of average (interval: 1–45 years). The clinical data, the MRI findings and the inter-observer concordance can be seen in Table 1.
In columns 1 through 5 the clinical data from each patient are shown. In columns 6 through 9 the grades reported by observer #1 and observer #2 are shown in the cochlear and vestibular right ear (RE), and in the cochlear and vestibular left ear (LE). In column 10 we can see if there is inter-observer consensus. In column 11 the findings from the MRI can be seen too: RE+/LE+ pathologic ear, cochlear (C) and vestibular (V) hydrops.
| Patient | Sex | Age onset | Progression years | Symptoms | Cochlear RE | Vestibular RE | Cochlear LE | Vestibular LE | Consensus | Positive ear, Cochlear C/Vestibular (V) hydrops |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 35 | 3 | LE vertigo, tamponade, hearing loss | 0/0 | 0/0 | 2/2 | 2/2 | Yes | LE+, C and V |
| 2 | F | 67 | 3 | RE, vertigo, hearing loss | 2/2 | 2/2 | 1/1 | 0/0 | Yes | RE+, C and V/LE+, C |
| 3 | M | 52 | 12 | LF, vertigo, acouphene, hearing loss | 0/0 | 0/0 | 1/1 | 1/1 | Yes | LE+, C and V |
| 4 | F | 40 | 10 | LE acouphene, vertigo, hearing loss | 0/0 | 0/0 | 0/0 | 0/0 | Yes | Negative |
| 5 | F | 39 | 7 | LE acouphene, vertigo, hearing loss | 1/0 | 0/0 | 2/2 | 2/2 | No | LE+, C and V |
| 6 | F | 21 | 6 | LE vertigo, acouphene, resolved hearing loss in between crisis | 0/0 | 0/0 | 1/1 | 2/2 | Yes | LE+, C and V |
| 7 | M | 26 | 45 | Fluctuating hearing loss | 0/0 | 0/0 | 0/0 | 0/0 | Yes | Negative |
| 8 | F | 27 | 25 | RE vertigo, hearing loss, acouphene | 1/1 | 1/1 | 0/0 | 0/0 | Yes | RE+, C and V |
| 9 | M | 51 | 1 | LE deafness after acoustic trauma years ago, RE sudden hearing loss a year ago afterwards fluctuating, tinnitus | 1/0 | 0/0 | 2/2 | 1/1 | No | LE+, C and V/RE+, C |
| 10 | M | 36 | 12 | RE sudden hearing loss and afterwards hearing loss, LE negative immunological study | 1/1 | 0/0 | 1/1 | 0/0 | Yes | RE+, C/LE+ C |
In all cases studied the images obtained were valid and of enough quality to be able to assess the endolympthatic space. The validity of the test was considered when comparing with asymptomatic ears and without EH of the patients studied.
There were no complications associated with intratympanic injections.
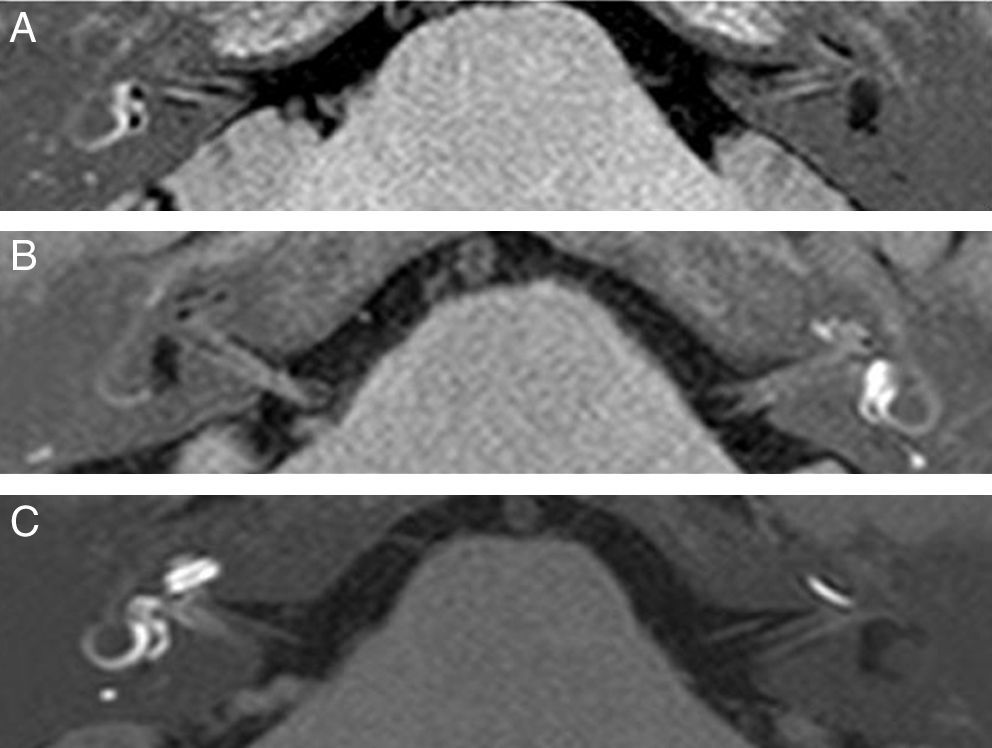
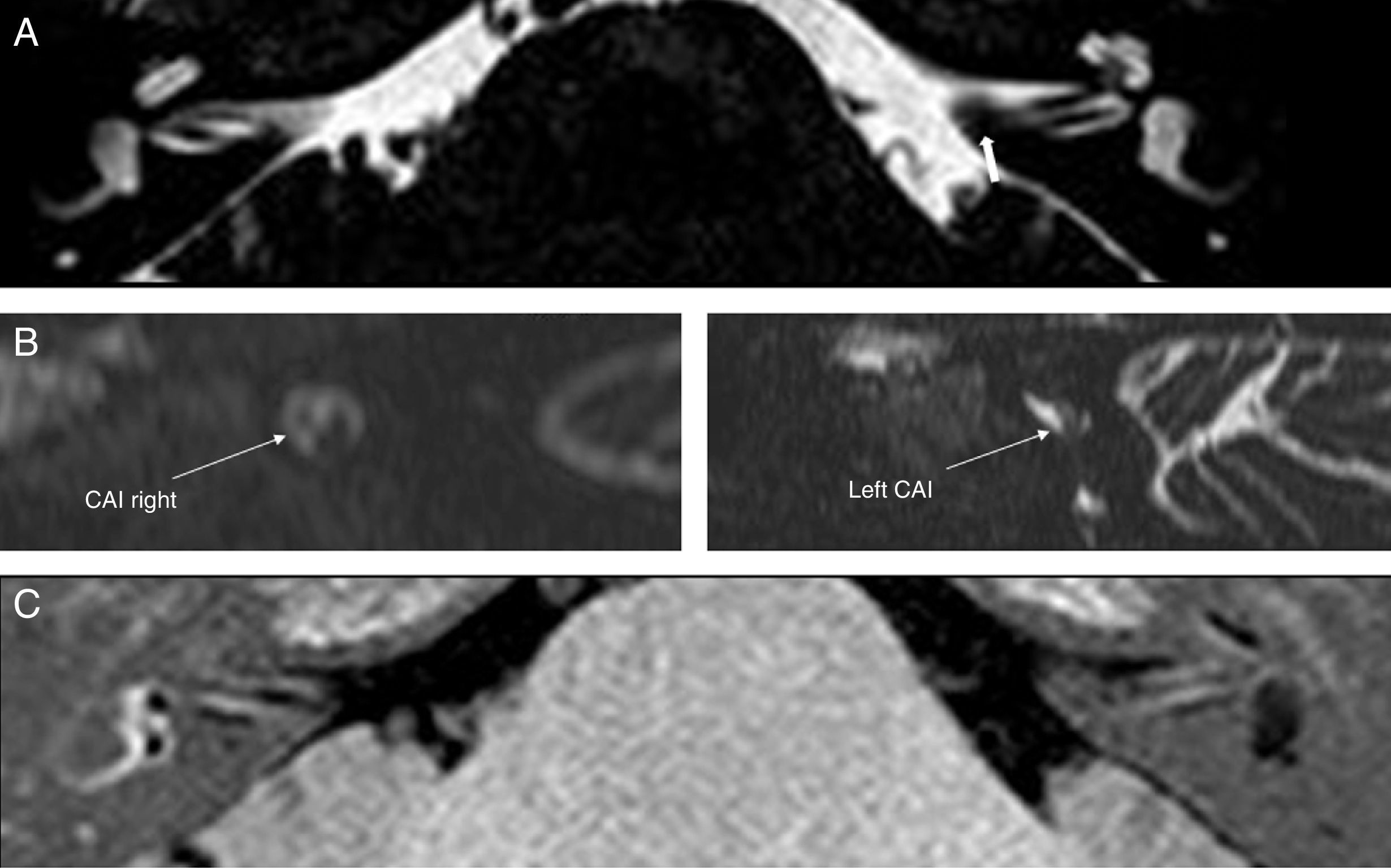
In all patients with vertiginous attacks associated with hearing loss and acouphenes (cases 1, 2, 3, 5, 6 and 8) with defined pro probable MD,4 hydrops was confirmed (Fig. 2).
3D real IR sequence after the administration of intratympanic gadolinium – axial projections. (A) Right ear: normal. Left ear: cochlear hydrops grade 2 and vestibular hydrops grade 2. (B) Right ear: cochlear hydrops grade 2 and vestibular hydrops grade 2. Left ear: cochlear hydrops grade 1 and vestibular hydrops grade 0. (C) Right ear: normal. Left ear: cochlear hydrops grade 1 and vestibular hydrops grade 2.
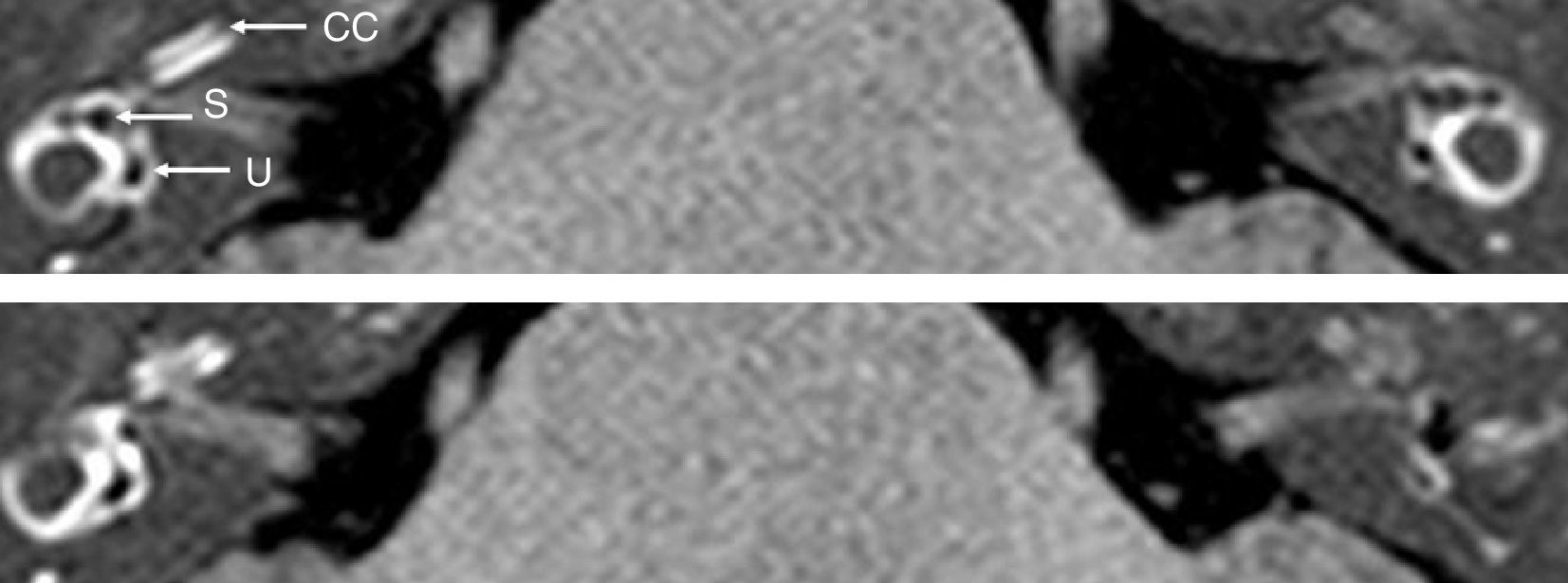
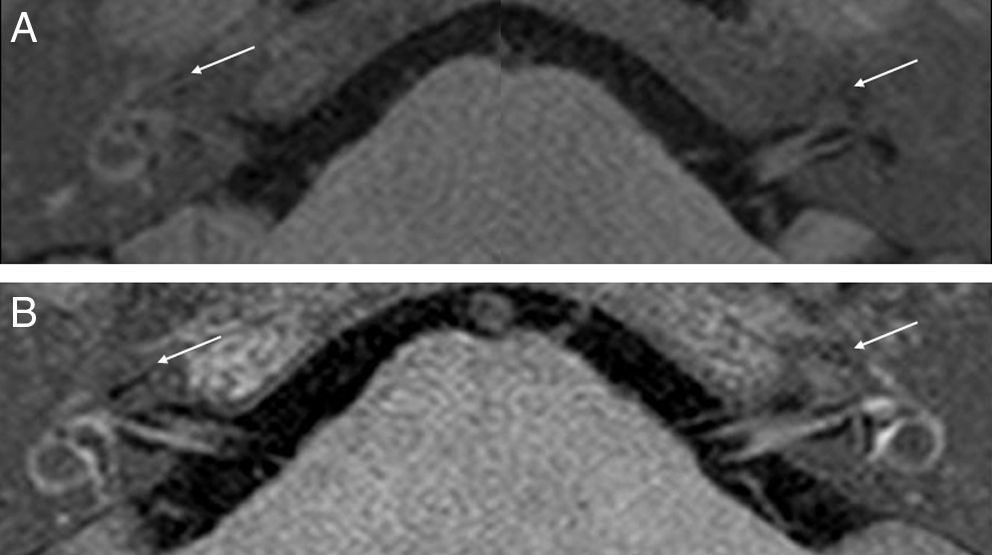
Of the four cases without vertiginous attacks no hydrops was confirmed in two of them (cases 4 and 7) (Fig. 3); however hydrops could be confirmed in cases with clinical manifestations of fluctuating hearing loss and a high clinical suspicion of AIED (cases 9 and 10) but with negative autoimmune tests (Fig. 4).
3D real IR sequence after the administration of intratympanic gadolinium—axial projections. No hydrops data. In the vestibule we can see that both the utriculum (U) and the saculum (S) are of normal morphology and size. The cochlear duct (CC) shows no dilation in the basal end included in this image.
3D real IR sequence after the administration of intratympanic gadolinium—axial projections. (A) This study achieves a slight enhancement of the perilymphatic space—explained maybe by the lower patency of membranes or swallowing 30min after the administration of contrast. Right ear: cochlear hydrops grade 1 (arrow) and vestibular hydrops grade 0. Left ear: cochlear hydrops grade 2 (arrow) and vestibular hydrops grade 1. (B) Right ear: cochlear hydrops grade 1 (arrow) and vestibular hydrops grade 0. Left ear: cochlear hydrops grade 1 (arrow) and vestibular hydrops grade 0.
There were inter-observer mismatches in the assessment of the presence or not of cochlear hydrops (grade 0 or grade 1) in cases 5 and 9.
DiscussionYet despite the fact that we have only recruited ten (10) cases the results herein illustrate the utility of this modality. In the six study patients with defined or probable MD based on the clinical criteria of the last consensus,4 the demonstration of EH could establish the positive diagnosis of MD same as Naganawa et al.15 who in their work found EH in the three cases with clinical suspicion of MD but could not confirm EH in the case without suspicion of MD.
However in patients without complete criteria of MD the revelance to this modality is much more important and this is why including it in selected patients can be decisive like we could see in case 1. Those were very disabling vertiginous attacks and in the morphological study the existence of a vascular loop with slight bone stenosis of the internal auditory canal (Fig. 5) was proposed as the possible cause for the disabling positional vertigo which led to considering surgery as one of the options. However the positive finding of EH allowed us to establish the ultimate diagnosis of MD and consequently reconsider therapy. Also it is important to know the possible bilaterality of this disease – that could be asymptomatic in the contralateral ear. This is how we achieved a 25% of bilateral cases of MD—percentage slightly higher than that achieved by Wu et al.16 (16.7%). In cases with strong suspicion of AIED we confirmed bilaterality (cases 9 and 10).
(A) DRIVE sequence. Axial reconstruction showing one bone protrusion at the beginning of the left internal auditory canal (IAC) (thick arrow). (B) DRIVE sequence. Sagittal plane reconstruction of both IAC showing focal stenosis secondary to bone ridge. (C) 3D real IR sequence after the administration of intratympanic gadolinium. Axial projection showing endolymphatic vestibuar and cochlear hydrops grade 2 in left ear.
In the four cases where the symptoms were no clearly suggestive of MD this modality was useful to be able to discard hydrops in two cases (cases 4 and 7) and modify therapy (withdrawing for instance diuretics).
The biggest advantage of this modality is that the interpretation of images is easy and the learning process is short. Inter-observer mismatches consisted of establishing grade 0 or grade 1 in the non-pathologic ear (case 5) or of a short time of clinical progression (case 9). This may be explained because grade 1 can produce nodular focal endolymphatic dilations inside the cochlea4—this is why the location of largest dilations should be taking into account before establishing the grade. To obtain objective measurements different groups use various softwares of volume automatic estimate.17
The most important setbacks of this modality are the lower availability of the intratympanic route of administration and the long sequence duration (almost 13min) both of which make it highly sensitive to movement artifacts.
The advantage of the intratympanic route of administration is that it uses a lower contrast dose since usually 0.9ml of diluted contrast are injected so toxicity is lower. Until now no adverse events following the administration of intratympanic diluted gadolinium on the inner ear have been reported.18,19
For our study and after numerous tests we obtained optimal images through the intratympanic route. However in the future we wish to implement one sequence after the administration of IV contrast to be able to add it to conventional studies thus opening up the possibility of radiological exploration. The election of the route of administration would depend on the availability of each institution; if collaboration with the ENT unit is possible for the administration of intratympanic gadolinium it would be possible to obtain sequences of a better quality with less advanced machines. The route of IV administration is fairly available but it needs more advanced technical requirements in MRI machines.
The MRI provides a very precise anatomic approach to the endolymphatic space that is almost an overlapping approach to the direct histological assessment. In the last consensus guidelines4 it was said that the finding of EH in cases of probable or definitve MD allows us to arrive at an ultimate diagnosis of MD. Thus including this modality in this type of patients can be very useful.
In the histological and radiological studies the presence of EH in more inner ear disorders6–8 have been confirmed. The confirmation of EH through the MRI can be very useful for the diagnosis of inner ear disorders presenting with vertigo and fluctuating hearing loss, and in the cases of MD it is possible.
In light of all this we suggest that in the future this modality should be included in the diagnostic protocol of MD. Also its use should be taken into consideration in cases of AIED without analytic confirmation when the differential diagnosis of MD is suggested to be able to confirm the presence or absence of hydrops – which in turn may have repercussions on the correct management of these patients.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments with human beings or animals have been performed while conducting this investigation.
Confidentiality of dataThe authors confirm that in this article there are no data from patients.
Right to privacy and informed consentThe authors confirm that in this article there are no data from patients.
Authors- 1.
Manager of the integrity of the study: MTG
- 2.
Study Idea: MTG, DRLD, JRGB
- 3.
Study Design: MTG, DRLD, JRGB
- 4.
Data Mining: MTG, BBA, JRGB
- 5.
Data Analysis and Interpretation: MTG, BBA
- 6.
Statistical Analysis:
- 7.
Reference: MTG, DRLD, JRGB.
- 8.
Writing: MTG, BBA, DRLD, JRGB.
- 9.
Critical review of the manuscript with intellectually relevant remarks: MTG, BBA, DRLD, JRGB.
- 10.
Approval of final version: MTG, BBA, DRLD, JRGB.
The authors declare no conflict of interests associated with this article whatsoever.
Please cite this article as: Tuñón Gómez M, Lobo Duro DR, Brea Álvarez B, García-Berrocal JR. Diagnóstico del hidrops endolinfático mediante resonancia magnética de 3T tras administración de gadolinio intratimpánico. Radiología. 2017;59:159–165.