To determine the sensitivity and accuracy of direct MR arthrography in the diagnosis of intra-articular lesions associated with femoroacetabular impingement.
Material and methodsWe used direct MR arthrography to study 51 patients with femoroacetabular impingement who underwent arthroscopic hip surgery. Surgery demonstrated 37 labral tears, 44 lesions in the labral–chondral transitional zone, and 40 lesions of the articular cartilage. We correlated the findings at preoperative direct MR arthrography with those of hip arthroscopy and calculated the sensitivity, specificity, positive predictive value, negative predictive value, and validity index for direct MR arthrography.
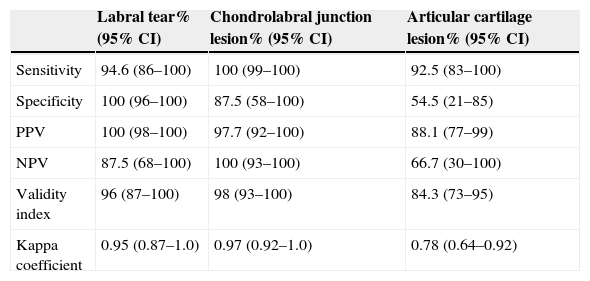
ResultsThe sensitivity and specificity of MR arthrography were 94.5% and 100%, respectively, for diagnosing labral tears, 100% and 87.5%, respectively, for diagnosing lesions of the labral–chondral transition zone, and 92.5% and 54.5%, respectively, for diagnosing lesions of the articular cartilage. The negative predictive value of MR arthrography for lesions of the labral–chondral transitional zone was 100%. MR arthrography accurately defined extensive lesions of the cartilage and the secondary osseous changes (the main factor in poor prognosis), although its diagnostic performance was not so good in small chondral lesions.
ConclusionIn patients with femoroacetabular impingement, direct MR arthrography can adequately detect and characterize lesions of the acetabular labrum and of the labral–chondral transitional zone as well as extensive lesions of the articular cartilage and secondary osseous changes.
Determinar la sensibilidad y la precisión de la artrografía mediante resonancia magnética (artro-RM) directa para diagnosticar lesiones intraarticulares asociadas al pinzamiento femoroacetabular.
Material y métodosEstudiamos con artro-RM directa a 51 pacientes con pinzamiento femoroacetabular que se operaron mediante artroscopia de la cadera la cual demostró 37 roturas del labrum, 44 lesiones en la unión condrolabral y 40 lesiones del cartílago articular. Correlacionamos los hallazgos de la artro-RM directa preoperatoria con los de la artroscopia de la cadera y calculamos la sensibilidad, especificidad, valor predictivo positivo, valor predictivo negativo e índice de validez de la artro-RM directa.
ResultadosLa sensibilidad y la especificidad de la artro-RM directa para diagnosticar la rotura labral fueron del 94,5 y del 100%, para la lesión de la unión condrolabral del 100 y del 87,5%, y para la lesión del cartílago articular del 92,5 y del 54,5%, respectivamente. El valor predictivo negativo de la artro-RM fue del 100% para las lesiones de la unión condrolabral. La artro-RM definió con precisión las lesiones extensas del cartílago y los cambios óseos secundarios, principal factor pronóstico desfavorable, mientras que su rentabilidad diagnóstica fue menor en pequeñas lesiones condrales.
ConclusiónLa artro-RM directa detecta y caracteriza adecuadamente las lesiones del labrum acetabular, de la unión condrolabral, lesiones extensas del cartílago articular y los cambios óseos secundarios en pacientes con pinzamiento femoroacetabular.
The hip is a complex anatomic region that has historically been a therapeutic challenge for trauma-orthopedic surgeons. The introduction of the secure hip luxation technique in 2001 allowed us to treat it securely.1 The interest for hip arthroscopy during the last years has improved our knowledge on the anatomy, biomechanics, and pathology of coxofemoral joint.
Hip pain is a common clinical issue in patients of all ages. The role of acetabular labrum and cartilage in pain and hip degenerative change is very well established2–5 especially in hip dysplasia.6 In femoroacetabular impingement (FAI) certain acetabular morphologic or proximal femur anomalies condition contact or “ahead” touch usually between the anterior–superior region and the femoral head–neck joint and the acetabular ring causing chondral and labrum lesions. Recent studies claim that the FAI is an important cause of early onset hip arthrosis especially in young active populations.7–12 Even though the diagnosis of FAI is clinical the role of image tests is essential. X-rays allow us to adequately diagnose the morphological anomalies characterizing FAI, bone dysplasia and arthrosis.13 MRIs allow us to exclude other causes of inguinal pain and arthrosis in early stages and the magnetic resonance arthrography (MR-arthro) clearly outlines lesions at labrum-level.14 Since 1996 several studies have established that direct MR-arthro is better than conventional MR15,16 to find and characterize lesions at the labrum acetabular and articular capsule-level by comparing the direct MR-arthro with hip arthroscopy that until that moment was the standard diagnosis.1,17 Recently the pathogenic role of the chondrolabral joint or transition in labrum and acetabular cartilage lesions in patients with FAI18 has been highlighted. In this article we tried to study the lesions at labrum and chondrolabral joint-level by correlating the arthroscopic findings with those of direct arthro-MR. The goal was to determine both the sensitivity and accuracy of direct arthro-MR for the diagnosis of lesions at labrum and chondrolabral joint and articular cartilage-level in patients who underwent arthroscopies to treat their FAI.
Material and methodsPatientsWe studied retrospectively patients that underwent arthroscopy at the Hospital Universitario Puerta de Hierro Majadahonda between October 2009 and July 2012. These patients had FAI criteria in their X-rays, according to the radiological report. We excluded patients with previous interventions above the hip and with other inguinal or hip pain causes shown by conventional MR, such as avascular necrosis, transitory osteoporosis, bone lesions (tumors, tears, including those due to failure), synovial disease (villonodular synovitis, synovial chondromatosis) tendinopathy, iliopsoas bursitis and extra-articular disease. In the cases of patients who had undergone surgery in both hips, only the first one was included. The final sample consisted of 51 FAI patients (25 males 19–61, mean age 43±9 years) who underwent direct arthro-MR examination between April 2009 and June 2012. All of them sought medical assistance due to slow onset inguinal pain without a clear traumatic history and presented with a typical limitation of hip flexion, adduction and internal rotation. The FAI was classified, according to the radiological findings, into “cam”, (28; 54.9%), “pincer” (14; 27.5%) and mixed types (9; 17.6%).
The study did not require the Hospital Ethical Commission's approval since all the patients in our study had signed the informed consent form for the direct arthro-MR and the arthroscopy where it is specified that their demographic data will be reviewed with scientific purposes.
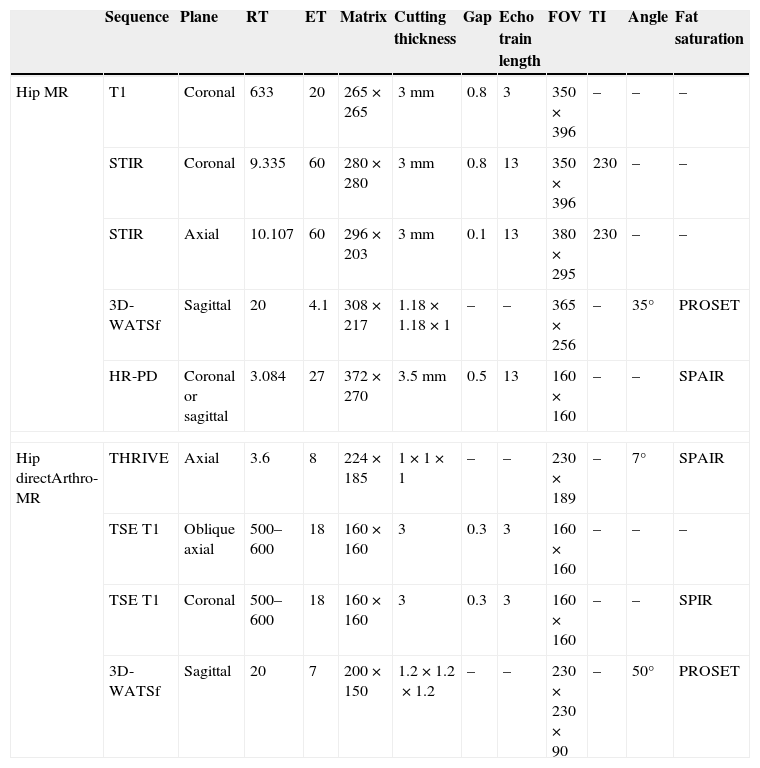
Radiological studiesAll patients underwent pelvis anterior–posterior X-ray19–21 and a modified Dunn–Rippstein22 axial projection with bone radiological technique (80kV, 12mAs), since the FAI radiological signs were one of the inclusion criteria. The conventional MR was performed with a 3T machine (Achieva dual quarsart 3T Philips, Edinhoven, The Netherlands) with a 6Ch-Torso-coil body coil to exclude other inguinal pain causes. The protocol (Table 1) included T1, STIR and 3D-WATSf-weighted sequences. Occasionally (14 patients) a high-resolution protonic density sequence was performed. The direct arthro-MR was performed with a 1.5T machine (Achieva nova 1.5T Philips, Edinhoven, The Netherlands) with a 5Ch-Cardiac-coil heart coil. To this end, ultrasound-guided contrast fluid was injected in the hip joint through one 22G, 10cm-long Chiva needle (Chiba echo-tip, Cook® Medical, USA), one delay <30min always and soft traction with a 5kg weight. The 20cc contrast solution contained gadoterate meglumine (DOTAREM® 0.5mmol/ml, Guerbet, France), 5cc of iodized iobitridol contrast (Xenetix® 300 Sol. inj. 6581g/100ml, Guerbet, France), 3cc of 1% lidocaine and 12cc of saline solution. Our protocol included the injection of iodine, except in allergic patients, just in case it was necessary to perform some radiological monitoring or complementary arthro-CTs.
Hip MR protocol in the 3T MR equipment and hip direct arthro-MR in the 1.5T MR equipment.
| Sequence | Plane | RT | ET | Matrix | Cutting thickness | Gap | Echo train length | FOV | TI | Angle | Fat saturation | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hip MR | T1 | Coronal | 633 | 20 | 265×265 | 3mm | 0.8 | 3 | 350×396 | – | – | – |
| STIR | Coronal | 9.335 | 60 | 280×280 | 3mm | 0.8 | 13 | 350×396 | 230 | – | – | |
| STIR | Axial | 10.107 | 60 | 296×203 | 3mm | 0.1 | 13 | 380×295 | 230 | – | – | |
| 3D-WATSf | Sagittal | 20 | 4.1 | 308×217 | 1.18×1.18×1 | – | – | 365×256 | – | 35° | PROSET | |
| HR-PD | Coronal or sagittal | 3.084 | 27 | 372×270 | 3.5mm | 0.5 | 13 | 160×160 | – | – | SPAIR | |
| Hip directArthro-MR | THRIVE | Axial | 3.6 | 8 | 224×185 | 1×1×1 | – | – | 230×189 | – | 7° | SPAIR |
| TSE T1 | Oblique axial | 500–600 | 18 | 160×160 | 3 | 0.3 | 3 | 160×160 | – | – | – | |
| TSE T1 | Coronal | 500–600 | 18 | 160×160 | 3 | 0.3 | 3 | 160×160 | – | – | SPIR | |
| 3D-WATSf | Sagittal | 20 | 7 | 200×150 | 1.2×1.2×1.2 | – | – | 230×230×90 | – | 50° | PROSET | |
HR-PD: high-resolution protonic density; FOV: field of view; Gap: degree of separation among cuts; PROSET: PRinciple Of Selective Excitation Technique; MR: magnetic resonance; SPAIR: SPectral Attenuated Inversion Recovery; SPIR: SPectral Presaturation with Inversion Recovery; STIR: Short inversion-Time Inversion Recovery; ET: echo time; THRIVE: T1 High-Res Isotropic Volume Excitation; TI: investment time; RT: repetition time; 3D-WATSf: 3D WATer Selective fluid.
The images were exported to a commercial working station (Extended MR Workspace 2.6.3.2. HF3 2010 Philips, Edinhoven, The Netherlands) where the images were post-processed to obtain multiplanar reconstructions from the T1 High-Res Isotropic Volume Excitation (THRIVE) sequence.
Image analysisThe radiological studies were reviewed by three expert radiologists in the musculoskeletal system (AMCR with 5 years of experience, MAPL with 20 years of experience and AHJ with 3 years of experience) and when they would disagree post-consensus agreement was reached. The radiologists did not know the findings of the arthroscopy when analyzing the images. Three (3) anatomical structures were analyzed in detail: (A) the labrum acetabular, (B) the chondrolabral joint and (C) the articular cartilage. Alterations in these structures were analyzed based on the type of FAI (D). Other morphologic findings associated with FAI (E) were also included in the study.
- A.
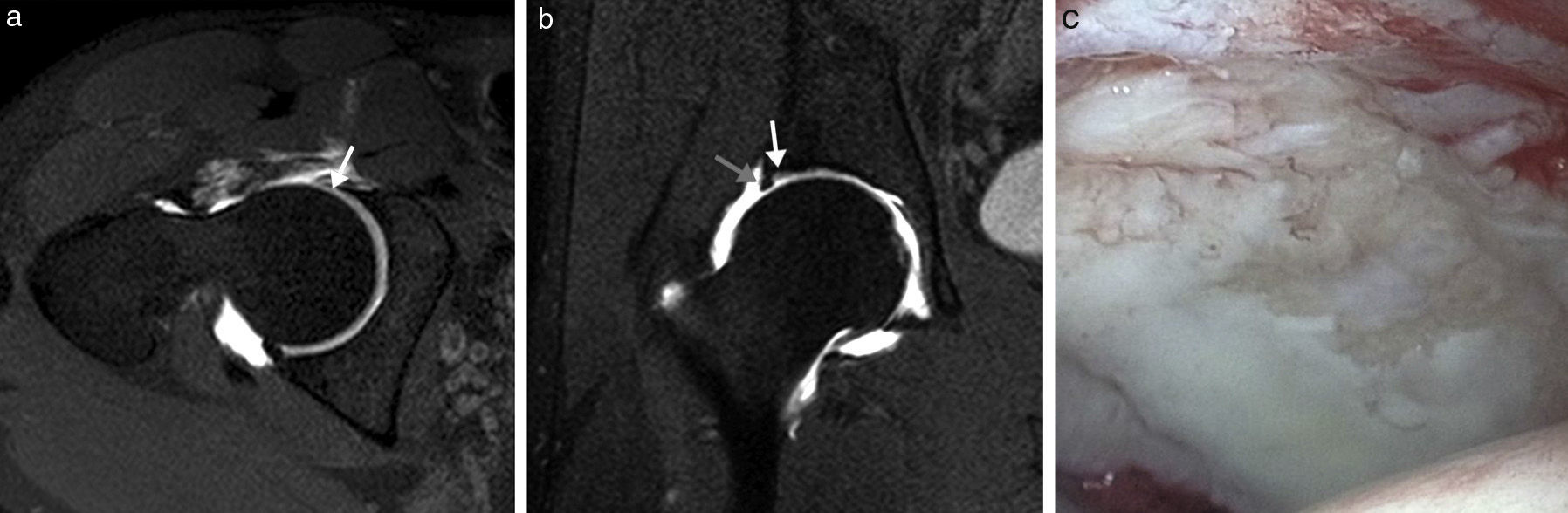
Labrum acetabular. It is a triangular structure with a low signal intensity in all MR sequences (Fig. 1). In the direct arthro-MR the perilabral recess can be seen too, that is, the space between the articular capsule and the labrum acetabular that distends itself after injecting a solution with a contrast agent (Fig. 1). We assessed the morphological alteration and the signal intensity like the main parameters.15 The presence of inter-substance contrast material in continuity with the labral surface was regarded as a tear.15 The displacement, absence or truncated shape of the labrum was regarded as indirect signs of tear.15 The presence of contrast in the chondrolabral junction associated with one signal alteration of the adjacent cartilage was regarded as tear/disinsertion (Fig. 2). The labrum thickening with intermediate signal inter-substance areas and margin irregularity was regarded as degenerative changes.23
Figure 1.Twenty-eight-year-old female with right inguinal pain. (a) The sagittal fat-saturated proton density-weighted 3T MRI shows the normal triangular, hypointense acetabular labrum (white arrow), the normal chondrolabral joint (hollow arrow), the normal femur head cartilage (white arrow) with discrete hyperintensity and the acetabular cartilage (gray arrow) with a slight normal intensity loss. (b) The sagittal fat-saturated proton density-weighted 3T MRI shows the normal acetabular labrum (gray arrow), the normal chondrolabral junction (white arrow) and the acetabular cartilage (hollow arrow) with a slight normal intensity loss. (c) The coronal THRIVE T1-weighted arthro-MR image shows the normal acetabular labrum (white arrow), the perilabral recess distended by the intraarticular contrast (gray arrow) and the acetabular cartilage (hollow arrow) with a slight signal intensity loss.
(0.15MB).Figure 2.Thirty-nine-year-old male with “cam”-type femoroacetabular impingement (FAI) at the right hip level. (a) The axial THRIVE T1-weighted arthro-MR image shows the anterior acetabular labrum tear (arrow). The intraarticular contrast dries the labrum. (b) The coronal THRIVE T1-weighted arthro-MR image shows the normal acetabular labrum in the superior–external region (gray arrow), the perilabral recess distended by the intraarticular contrast and the chondrolabral junction cartilage (white arrow) with normal loss signal intensity. (c) The right hip arthroscopic image shows the extensive articular cartilage lesion–typical of “cam”-type FAI.
(0.14MB).In an attempt to compare our results with those published the lesions of the acetabular labrum were categorized following the criteria set by Czerny16 in the direct arthro-MR specifying for each stage if perilabral recess was normal (subtype A) or if the thickened labrum did not allow us to see the perilabral recess (subtype B): stage 0–homogeneous hypointense triangular labrum and continuous anchorage to the lateral margin of the acetabulum. Normal perilabral recess; stage I–triangular labrum with one hyperintense area or one focal hyperintensity in the middle that does not spread to the margin of the labrum and continuous anchorage to the lateral margin of the acetabulum; stage II: triangular labrum with discontinuity in the margin and intra-substance contrast and continuous anchorage to the lateral margin of the acetabulum; stage III: triangular labrum disinserted or separated from the acetabulum.
- B.
Chondrolabral joint. Also known as chondrolabral transition area, it includes the hyaline cartilage located less than 5mm away from the labrum. In a normal chondrolabral joint (Fig. 1) there is no cleavage plane between the labrum–hypointense in all sequences–and the acetabular cartilage–isointense in short TE sequences and discretely hyperintense in T2-weighted sequences.
Our classification of chondrolabral joint lesion is based on the proposal by James et al.18 to which we add a degree assigned to the decrease of the normal cartilage signal (degeneration)–Degree I. This way we can distinguish cartilage degeneration from chondrolabral joint separation. We say that there are 5 degrees in direct arthro-MR: Degree 0, normal chondrolabral joint characterized by an intermediate signal of the acetabular cartilage adjacent to the labrum; Degree I, cartilage degeneration, with hypointensity of the cartilage adjacent to the labrum; Degree II, labrum separation, the groove filled with contrast between the labrum and the acetabular hyaline cartilage, which shows some focal alteration or normal signal loss; Degree III: labrum separation and cartilage degeneration–groove filled with contrast between the labrum and the acetabular cartilage (the latter shows thinning areas or partial or complete thickness tears); Degree IV: absence of cartilage, articular cartilage loss seen with bone exposure immediately adjacent to the labrum.
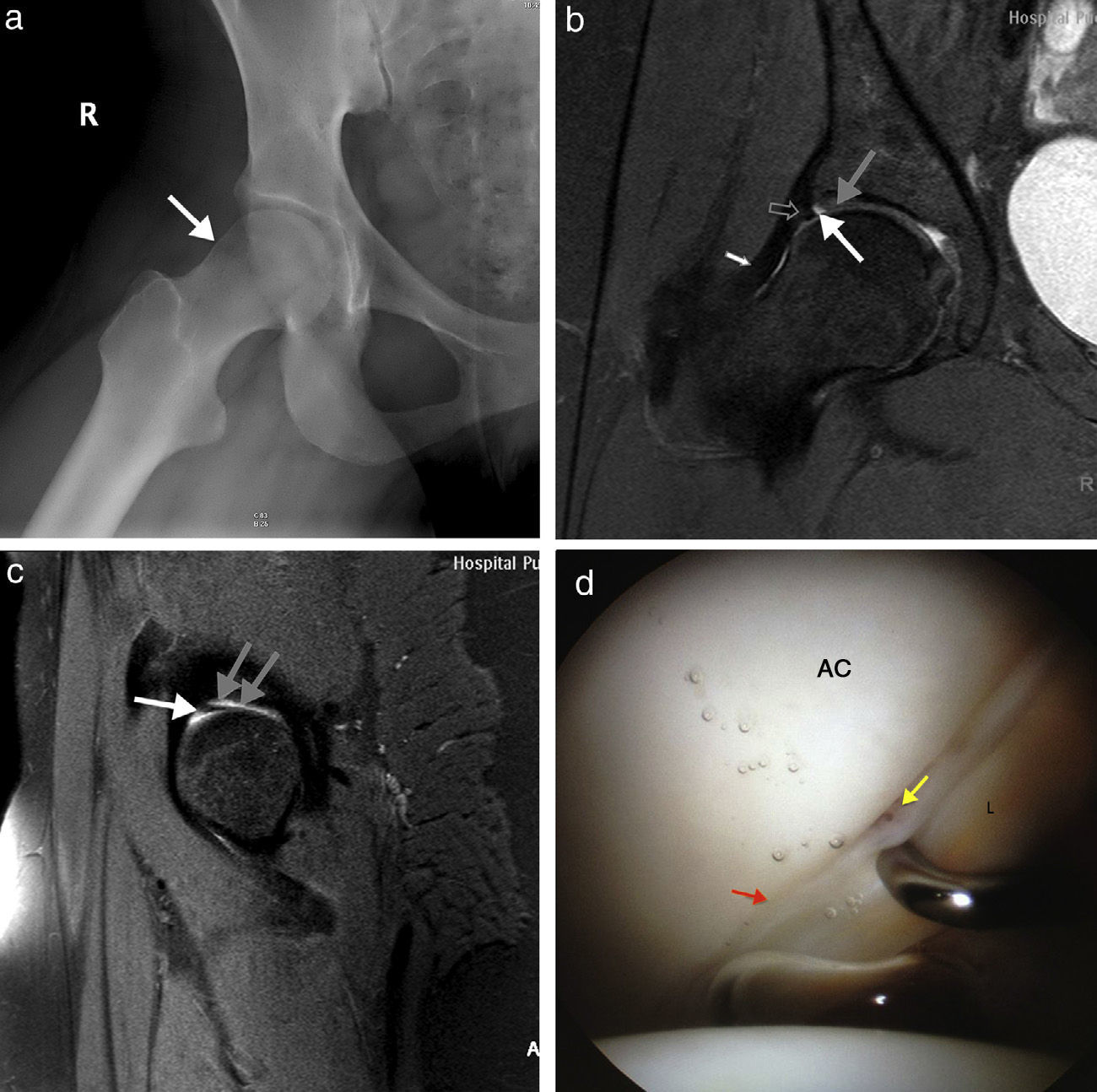
On the other hand, we can also distinguish labrum separation from a sublabral sulcus (Fig. 3)–a variant of normalcy that is usually located in the posterior-inferior region without other morphological or signal alterations in the neighboring structures–labrum and acetabular cartilage.
Figure 3.Thirty-one-year-old female with right hip “cam”-type femoroacetabular impingement. (a) The modified Dunn axial radiograph shows deformity in the anterior–superior region of the head–neck femur junction (white arrow). (b) The coronal 3T sagittal fat-saturated proton density-weighted image shows the acetabular labrum of normal size, shape and signal intensity (hollow arrow); the sublabral sulcus (white arrow) is defined as the plane of separation in the chondrolabral junction with hyperintensity between the acetabular labrum and the chondrolabral junction cartilage (gray arrow) that shows normal thickness and intermediate signal intensity; the articular capsule (white arrow) is not distended so not defined as perilabral recess. (c) The 3T sagittal fat-saturated proton density-weighted MR image shows the sublabral sulcus (gray arrows) and the acetabular labrum (white arrow). (d) The right hip arthroscopic image shows the acetabular cartilage (AC), and the chondrolabral junction (red arrow), the palpator retracts the normal acetabular labrum (AL) showing the sublabral sulcus (yellow arrow).
(0.23MB). - C.
Articular cartilage. Cartilage lesions on the acetabular and femoral surfaces are classified according to the Outerbridge24 system into 5 degrees: Degree 0, intact articular cartilage; Degree I, hypointensity in the articular cartilage; Degree II, ulceration, tear or fibrillation affecting less than 50% of cartilage thickness; Degree III, ulceration, tear or fibrillation affecting more than 50% of cartilage thickness and Degree IV, absence of cartilage with bone exposure.
- D.
Acetabular labrum, chondrolabral joint and cartilage lesions based on the type of FAI. We categorize the pincer, cam and mixed types (when the characteristics of the first two overlap)7 of coxofemoral impingement. The pincer type is characterized by an excessive, focal or diffuse coating of the femoral head12 and the cam type by a gibbus in the femoral head–neck joint, causing the femur head to have a flat or convex shape.13 In order to simplify and be able to compare the degree of an articular cartilage lesion among the FAI types, we categorize two groups of cartilage lesions– arthrosis (corresponding to Degree IV) and non-arthrosis (the remaining).
- E.
Other FAI-based morphological findings. Pit's synovial hernia, os acetabuli, paralabral cyst and alpha angle were described in the arthro-MR readings.
One traumatologist (JCLV), experienced in more than 150 hip arthroscopies, performed this proceeding in all patients showing the intraoperative findings in the surgical section. Due to care reasons the traumatologist knew about the outcome of radiologic tests. The average waiting time between the arthro-MR and the hip arthroscopy was 6 months (range 1 week–13 months). During the waiting no traumas were reported.
Statistical analysisThe statistical analysis of data was performed by the Hospital Department of Biostatistics (IMS) through the SPSS software version 14 (SPSS Inc., Chicago, IL, USA).
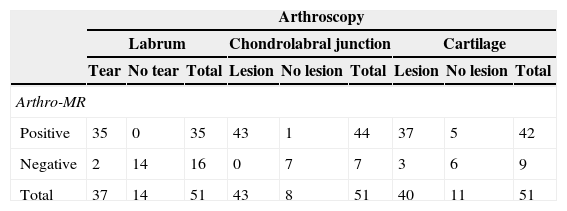
We compared the findings of direct arthro-MR with those of hip arthroscopy by taking the latter as the standard of reference (Table 2). In the alterations of the acetabular labrum, the normal (stage 0) or degenerative (stage I) labrum was considered true negatives (TN), and the labral tear or displacement (stages II and III) both in the arthro-MR and in the hip arthroscopy was considered true positives (TP). The diagnosis of labral tear or displacement in the arthro-MR was considered false negative but it was normal or shown degeneration in the arthroscopy. The diagnosis of normal or degenerative labrum in the arthro-MR that was torn or displaced in the arthroscopy was regarded as a false negative. Both in the affectation of chondrolabral junction and the articular cartilage the absence of lesions (Degree 0) was regarded as a TN and Degrees I–IV–both in the arthro-MR and the arthroscopy–were regarded as a TP. Finding lesions through arthro-MR with normal arthroscopy was considered a false positive and a normal arthro-MR with pathologic findings in the arthroscopy was considered a false negative. From this analysis we were able to estimate the sensitivity (S) and specificity (SP), the positive predictive value (PPV), the negative predictive value (NPV), and the validity index (VI) of the hip direct arthro-MR. The VI or the right proportion of accuracy is defined as the proportion of individuals correctly categorized and responds to the following formula: IV=(TP+TN)/total number of patients.
Comparison between hip direct arthro-MR and hip arthroscopy taking the latter as the standard of reference.
| Arthroscopy | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Labrum | Chondrolabral junction | Cartilage | |||||||
| Tear | No tear | Total | Lesion | No lesion | Total | Lesion | No lesion | Total | |
| Arthro-MR | |||||||||
| Positive | 35 | 0 | 35 | 43 | 1 | 44 | 37 | 5 | 42 |
| Negative | 2 | 14 | 16 | 0 | 7 | 7 | 3 | 6 | 9 |
| Total | 37 | 14 | 51 | 43 | 8 | 51 | 40 | 11 | 51 |
Arthro-MR: magnetic resonance arthrography.
Also we used the Pearson's chi-square test to evaluate the differences between the groups of patients based on FAI and the Cohen's kappa index with 95% confidence intervals in order to assess the diagnostic concordance between the direct arthro-MR and the arthroscopy. For all tests one significance level <5% in the bilateral contrast was considered acceptable.
ResultsOut of the 51 patients with FAI treated with arthroscopy due to morphologic alterations of the femur head or acetabulum only three (3) did not show articular lesions, 37 patients showed acetabular labrum tear, 44 chondrolabral junction lesions and in 40 patients lesions of the articular cartilage were diagnosed. The values of S, SP, positive predictive value, NPV, and VI of both the hip direct arthro-MR and kappa's index can be seen in Table 3.
- A.
Acetabular labrum. The arthro-MR correctly identified the normal labrum in 5 patients and degenerative changes in 9 patients (7 stage IA and 2 stage IB). In the 37 patient-group (72.5%) with labral tears the arthro-MR correctly spotted the 4 stage II patients (3 stage IIA and 1 stage IIB); however out of the 23 stage IIIA patients (according to the arthroscopy) (labral displacement) in the arthro-MR 2 stage II patients (degeneration) were misdiagnosed.
- B.
Chondrolabral junction. The arthro-MR VI was 98%; 7 patients were Degree 0, 13 Degree I, 9 Degree II, 17 Degree III and 4 Degree IV. Only in one case there was disagreement–when the arthro-MR confirmed stage IV and the arthroscopy stage III.
- C.
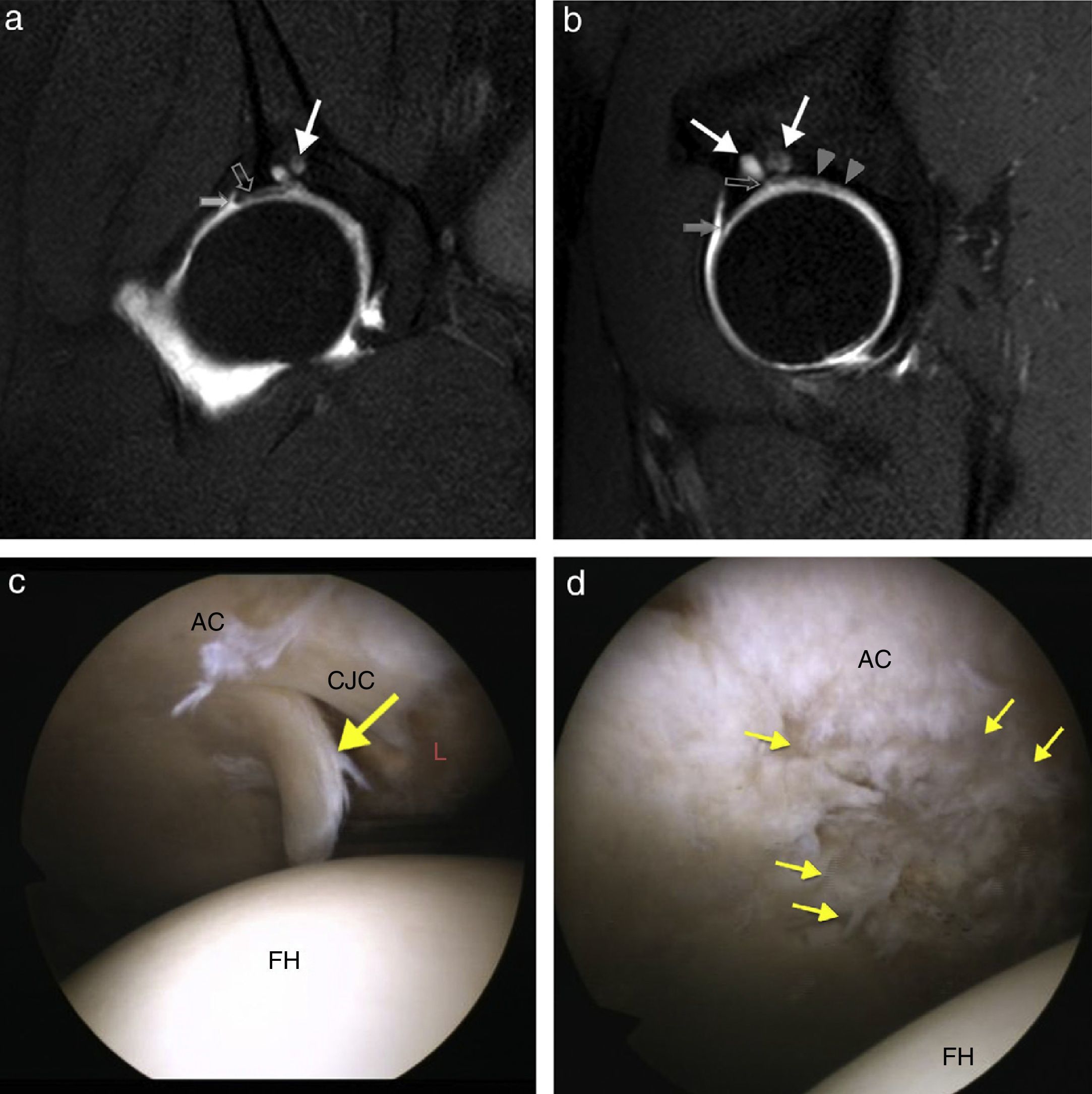
Articular cartilage. VI was 84.3%: there were 6 patients without lesions in the articular cartilage and 37 with lesions (17 patients were Degree I, 3 Degree II, 2 Degree III and 15 Degree IV). Disagreement between the two tests happened in 8 patients (15.7%): the arthro-MR could not confirm cartilage alterations in 3 patients– 2 with stage I lesions and 1 with stage III lesions in the arthroscopy. In one case the arthro-MR stratified one stage I patient while the arthroscopy confirmed no alterations were present. In 3 patients the arthroscopy underestimated the alterations: 2 cases categorized as grade II and 1 as grade III when the arthro-MR would show Degree IV geodes (Fig. 4).
Figure 4.Forty-four-year-old male with right hip “cam”-type femoroacetabular impingement. (a) The coronal 3T sagittal THRIVE fat-saturated T1-weighted image shows the acetabular labrum of the superior–external region with a slight signal increase due to degenerative changes (white arrow); separation plane of the chondrolabral junction (hollow arrow) in which contrast is introduced due to labral displacement; signal hypointensity of both the acetabular cartilage and geodas in the acetabulum ceiling (white arrow). (b) The sagittal THRIVE T1-weighted arthro-MR image shows the small anterior acetabular labrum (gray arrow) with normal signal intensity; the acetabular cartilage (arrow heads) shows signal hypointensity foci while geodas can be seen in the acetabulum (arrows) in communication with the articular space (hollow arrow). (c) The image of the right hip arthroscopy shows the femur head (FH), the acetabular cartilage (AC), and the chondrolabral junction cartilage (CJC), and one “trap door”-like lesion (arrow); the acetabular labrum (A.L.) is frayed due to degenerative changes. (d) The arthroscopic image shows normal femur head (FH) cartilage and AC alterations in a big area (outlined by arrow heads) with surface irregularities and fraying.
(0.26MB). - D.
FAI-type-acetabular labrum, chondrolabral junction and cartilage lesions. There were no significant differences for the different types of alterations of the acetabular labrum, the chondrolabral junction and the various types of FAI. It was not like that in the cartilage lesions based on the type of FAI. We could confirm a greater extension and degree of the acetabular cartilage lesion in the anterior–superior region of the “cam”-type FAI (Fig. 2). Of the 28 patients with “cam”-type FAI half of them had arthrosis but the other half did not while only 4.3% of the mixed and “pincer”-type FAI patients had arthrosis and 95.6% did not (p=0.002).
On the other hand the paralabral cyst of posterior location that we saw in four patients was associated with the “pincer”-type FAI only.
- E.
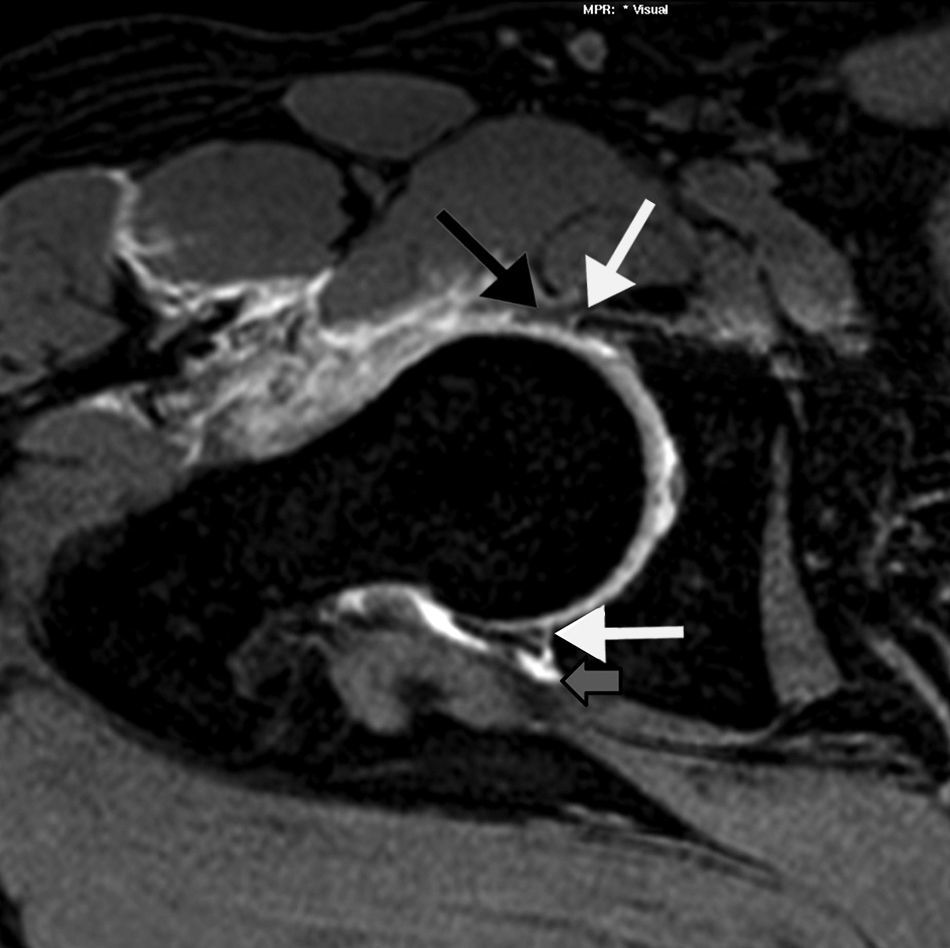
Other morphologic findings associated with FAI. Perilabral recess was clearly defined in 72.5% of hip arthro-MR studies. In 9 patients one os acetabuli could be confirmed. Four (4) patients showed paralabral cysts only (Fig. 5).
Figure 5.Forty-two-year-old male with “pincer”-type FAI. The axial THRIVE T1-weighted arthro-MR images shows the acetabular labrum of the anterior region (black arrow) degenerated with intermediate signal; separation plane or anterior chondrolabral junction tear (white arrow) where contrast is introduced between the anterior acetabular labrum and the bone rim; in the posterior region of the acetabular ring; the posterior region of the acetabular ring shows the separation plane or posterior chondrolabral junction tear (white arrow) plus one posterior paralabral cyst (gray arrow) in communication with the articular space.
(0.09MB).
Statistical indicators of the comparison between the direct arthro-MR and hip arthroscopy.
| Labral tear% (95% CI) | Chondrolabral junction lesion% (95% CI) | Articular cartilage lesion% (95% CI) | |
|---|---|---|---|
| Sensitivity | 94.6 (86–100) | 100 (99–100) | 92.5 (83–100) |
| Specificity | 100 (96–100) | 87.5 (58–100) | 54.5 (21–85) |
| PPV | 100 (98–100) | 97.7 (92–100) | 88.1 (77–99) |
| NPV | 87.5 (68–100) | 100 (93–100) | 66.7 (30–100) |
| Validity index | 96 (87–100) | 98 (93–100) | 84.3 (73–95) |
| Kappa coefficient | 0.95 (0.87–1.0) | 0.97 (0.92–1.0) | 0.78 (0.64–0.92) |
95% CI: 95% confidence intervals; arthro-MR: magnetic resonance arthrography; NPV: negative predictive value; PPV: positive predictive value.
In our series of patients thanks to hip direct arthro-MR we found 94.5% tears and displacements of the acetabular labrum, 100% of chondrolabral junction lesions and 92.5% of cartilage lesions diagnosed through hip arthroscopy. The NPV of hip arthro-MR was 100% for chondrolabral junction lesions. The correlation between the arthro-MR and hip arthroscopy for alterations of the acetabular labrum has been really good in our series considering we tried to characterize the lesions of the acetabular labrum by distinguishing between tear and displacement of degenerative changes. These outcomes are in line with other publications of reference. In 1999, Czerny et al.25 published a series of 40 patients who underwent hip arthro-MR and arthroscopy out of which 35 had lesions of the acetabular labrum; the arthro-MR sensitivity was 91% and specificity 71%. A few subsequent studies have shown similar results.26
Most tears (55–92%) occur in the anterosuperior acetabular labrum.5,27,28 This location combined with the labrum anatomical orientation–anchored to the acetabular ring– poses a challenge to detect labral lesions. In an effort to improve diagnostic performance, some authors have shown a certain preference for oblique or radial planes.18,29,30 In our everyday practice, gradient echo volumetric sequences make it possible, through multiplane reconstructions, for images to be optimized in each case.
The chondrolabral joint has gained importance recently in the FAI pathogenesis because it is believed that the alterations occur in the anchorage of the labrum to the acetabulum and they initially respect the body of the labrum.18 Chondrolabral joint lesions include labral separation and adjacent cartilage anomalies. The assumption that they are both related is based on the works by Beck et al.31 and Schmid et al.32 They both proved that in the FAI there are alterations in the chondrolabral joint cartilage in all patients with labral anomalies. This has also been the case in our experience. In the series by James et al.,18 of 38 patients with chondrolabral joint alterations in arthroscopy, 97% were identified through MRIs.
Chondrolabral lesion is by far the factor that shades the most the mid-short term prognosis of surgical therapy.31 Hence the importance of precise diagnosis to discard patients with advance degenerative changes and give precise information on what results we can expect after surgery.31,33 Unlike labral lesions where arthro-MR is superior to conventional MR,15,16,25,26 the cartilage morphological alterations are still a diagnostic challenge for both image modalities.34,35 The acetabular cartilage lesions and those of the femur head pose the following paradox: conventional MR is excellent and superior to arthroscopy to define bone changes secondary to chondral lesions and lesions affecting the whole cartilage thickness. But the sensitivity for low-grade cartilage lesions is lower in the arthro-MR or high-field MR as opposed to the arthroscopy. The difficulty probably lies in the fact that the hip joint cartilage thickness is really thin compared to other joints like the knee,33,35 that the surface is curved35 and that the acetabular and femoral cartilage surfaces just do not fit in.18,35 This is why applying the modified Outerbridge classification24 can be really difficult especially in grades 0–II.
1.5T MR high-resolution sequences improve the diagnostic yield.18,30 They can get to identify almost 90% of the acetabular cartilage lesions and 100% of the femur head cartilage lesion,18 and even with a good outcome (86–92%) more subtle cartilage lesions (grade I).30 It is expected that the 3T MRI has a bright future for the bloodless diagnosis of the acetabular labrum or joint cartilage lesions.36 Due to the etiopathogenic differences of FAI, the intra-articular lesions vary in extension and location based on the predominant morphological alteration. In the “pincer”-type impingement the acetabular labrum can be hurt in the anterior region and characteristically the chondral lesion can be hurt in the acetabulum posterior rim12,14 due to a fulcrum or counter-blow mechanism of the femur head.7,37 In our experience when the posterior cartilage lesion is produced in the chondrolabral transition a small paralabral cyst can be associated. In most of our patients with the “cam”-type FAI – other than the characteristic triad38 of the alpha angle increase – anterior–superior acetabular cartilage lesion and anterior–superior labral lesions we have been able to find a greater extension and degree of the acetabular cartilage lesion at the anterior–superior region level. This observation matches other studies that suggest that patients with “cam”-type FAI and alpha angle >65° run a greater risk of articular cartilage lesions while the increase of the acetabular coverage seems to have protective effects.39
Among the limitations of this study we can mention in the first place that the waiting time between the hip arthro-MR and the arthroscopy (median 6 months) was too long due to institutional and care reasons. In this period the articular cartilage affectation progressed which can in turn affect the correlation accuracy between both modalities. Secondly the classifications that we used are useful to compare our results with other studies on radiology but it is not proven yet if they are important when it comes down to therapy since the correlation with Lage arthroscopic classification is poor.28,40 On the other hand the size of our sample is small and patients were selected among the studied ones through hip arthroscopy and they already had FAI radiological alterations. Lastly 14 patients had one high resolution additional in the 3T MR. These images were assessed in the clinical setting and even though there were not reviewed for this work they could have influenced the clinical decisions.
Based on our results there are two possible lines of research. In the first place the utility of hip direct arthro-MR is still to be determined for the detection of intra-articular lesions in patients with not only clinical manifestations of FAI but also with mild or absent radiological alterations. And in the second place we still need to establish what the role of 3T MRI with high-resolution sequences is in the diagnostic protocol of FAI.
In sum the direct arthro-MR adequately finds and characterizes chondrolabral junction and acetabular labrum lesions in patients with FAI. The extensive lesions of the articular cartilage and secondary bone changes (geodes, edema-like lesions and subchondral sclerosis) – main prognostic unfavorable factors in patients with FAI – are better defined in MR explorations (included arthro-MR) than in arthroscopies. Nevertheless the cost-effectiveness of arthro-MR in low-grade chondral lesions is lower.
Ethical responsibilitiesProtection of people and animalsAuthors confirm that no experiments have been performed on human beings or animals.
Data confidentialityAuthors confirm that the protocols of their centers have been followed on matters concerning the publishing of data from patients. They also confirm that all patients included in this study have been given enough information and handed over their written informed consent for their participation in this study.
Right to privacy and informed consentAuthors confirm that in this report there are no personal data from patients. This document is kept by the corresponding author.
Author contribution- 1.
Manager of the integrity of the study: AMCR.
- 2.
Original idea of the study: AMCR, JCDLV, MAPL.
- 3.
Study design: AMCR, JCDLV, IMS.
- 4.
Data collection: AMCR, JCDLV, MAPL, IMS.
- 5.
Data analysis and interpretation: AMCR, JCDLV, MAPL, IMS, MP.
- 6.
Statistical analysis: AMCR, IMS.
- 7.
Reference search: AMCR, JCDLV, MAPL.
- 8.
Writing: AMCR, IMS.
- 9.
Manuscript critical review with intellectually relevant contributions: JCDLV, MAPL, MP.
- 10.
Final version approval: All authors have read and approved the final version of this article.
The authors reported that there are no conflict of interests.
Our gratitude to Dr. Luis Ramos González, MD Chief of the Unit of Radiodiagnosis at the Hospital Universitario Puerta de Hierro (2002–2012) for promoting the magnetic resonance arthrography (arthro-MR) and always cheering us up in our search for excellence in our caring, teaching and scientific activities. Also our gratitude to Ana Hualde Juvera– excellent radiologist and friend–for helping us review all the arthro-MR images.
Please cite this article as: Crespo Rodríguez AM, de Lucas Villarrubia JC, Pastrana Ledesma MA, Millán Santos I, Padrón M. Diagnóstico de lesiones del labrum acetabular, de la unión condrolabral y del cartílago en el pinzamiento femoroacetabular: correlación entre artrografía mediante resonancia magnética directa y artroscopia de cadera. Radiología. 2015;57:131–141.