Renal colic is a common reason for presentation to emergency departments, and imaging has become fundamental for the diagnosis and clinical management of this condition. Ultrasonography and particularly noncontrast computed tomography have good diagnostic performance in diagnosing renal colic. Radiologic management will depend on the tools available at the center and on the characteristics of the patient. It is essential to use computed tomography techniques that minimize radiation and to use alternatives like ultrasonography in pregnant patients and children. In this article, we review the epidemiology, clinical and radiologic presentations, and clinical management of ureteral lithiasis.
El cólico renal es un motivo frecuente de consulta en los Servicios de Urgencias y la imagen diagnóstica se ha convertido en una herramienta fundamental del diagnóstico y manejo clínico. La ecografía y, fundamentalmente, la tomografía computarizada sin contraste permiten diagnosticarlo con un rendimiento elevado. El manejo radiológico va a depender de la disponibilidad del centro y de las características de la población. Es imprescindible usar técnicas de baja dosis de radiación en la tomografía computarizada y técnicas alternativas como la ecografía en embarazadas y niños. En este artículo hacemos una revisión epidemiológica, clínica, radiológica y del manejo clínico de la litiasis ureteral.
Renal colics (RC) are the most frequent clinical manifestation of renal lithiasis and a common cause for seeking Hospital Emergency Services (HES). Diagnosing and treating them early reduce complication which is derived from maintained urinary obstruction, such as renal function deterioration and infection accompanied by septic shock risk. Diagnostic imaging plays an important role in clinical management when trying to confirm lithiasis, stage the extent of obstruction in the collector system, assess the probability of spontaneous expulsion and identify complications or alternative diagnoses.1–3 In addition, it makes it easier to select the best therapeutic option, which can be a medical treatment, extracorporeal lithotripsy or nephrolithotomy, endoscopically or percutaneously. The number and size of the calculi as well as their composition influence the selection,2 in such a way that uric acid lithiases respond to medical treatment and extracorporeal lithotripsy is not effective in cases of cysteine, brushite or calcium oxalate monohydrate lithiases. Radiological techniques are also useful to follow the calculus until it is expelled and then to decide whether to maintain medical treatment or complement it with an endourological procedure. The options include simple radiography, intravenous urography (IVU), ultrasound, computed tomography (CT) and magnetic resonance images (MRI). A swift and precise diagnosis has made it possible to use CT without contrast as the first option for patients with acute lumbar pain suggesting RC, a recommendation endorsed by scientific societies such as the American College of Radiologists and the American Urological Association.2,3 Such a recommendation, along with the progressive availability of CT scanners in ER, has promoted a rapid increase in the number of examinations, which in patients with suspicion of RC got multiplied by a factor of 10 in 11 years.4 As a consequence, there has been a parallel rise in the collective radiation dose, which has not entailed a parallel improvement of the “patient-based indicators”, such as the increase in the percentage of lithiasis diagnoses, relevant alternative disease or the percentage of hospitalized patients.4 In order to minimize the doses of radiation it is recommended to use low-dose techniques2 that allow us to reduce such doses up to 70%, according to personal preferences and the technological availability of the scanner. Results with studies using ultra-low doses have been recently published with a range below that of abdominal radiography,5 yet availability of this technique is still limited, as shown by a recent study where only 2% of the CT were performed with doses lower than 3milisieverts (mSv).6 Also patients with ureteral lithiasis undergo image examination before, during and after treatment, a situation that gets itself more complicated due to a certain trend to have lithiasis relapses. Therefore, the examination is highly likely to be repeated once or twice along the process, with the subsequent cumulative effect of the dose in a population that due to its average age of around 40 years is radiosensitive suggestive of caution with the doses.7,8 Consequently, the European Association of Urology recommends ultrasound as the first imaging modality to be used in RC.9
The goal of this article is to review the utility of imaging diagnostic techniques for the clinical diagnosis and management of renal colics.
EpidemiologyThe incidence of urolithiasis in Spain is 0.73%, which amounts to some 325,000 new cases every year.10 RC is the most frequent complication of renal lithiasis, with an incidence between 0.9 and 3 cases/1000 inhabitants/year11,12 and it usually affects patients between 20 and 60 years old, with a maximum incidence between 40 and 60 years old men predominantly.12–14 It is estimated that up to 12% of men and 6% of women will experience one or more RC episodes in their lives,12 with a recurrence rate of 50%.15 One in four patients with RC has a family history of RC a situation that multiplies the risk of lithiasis by three.16
Depending on the size and location of the calculus, expulsion can take a few hours or even several weeks, a period of time in which successive episodes of colic pain may occur. Some calculi will not be expelled spontaneously and will require intervention; also relapse is common after the index event.17
Clinical contextRC is triggered by partial or complete ureteral obstruction, usually due to an impacted lithiasis that raises pressure significantly. The classic clinical presentation of ureteral lithiasis is intense, unilateral, sudden colic pain. It is initially located in the lumbar fossa usually irradiating toward the inguinal and genital areas to later evolve when the calculus descends in such a way that in the middle ureter it can simulate appendicitis or diverticulitis, depending on its location–right or left. As the calculus comes closer to the bladder, the symptoms of vesical irritation predominate, such as polakisuria and tenesmus. It is usually accompanied by digestive symptoms such as nausea, vomiting or constipation due to ileus reflux.12,16,18 In approximately 90% of the patients hematuria occurs yet the lack of it does not exclude RC12,15; even half of the patients with aneurisma of the abdominal aorta can have it.19 With the typical pain accompanied by hematuria, clinical diagnosis is possible and the imaging tests do not strictly be necessary since they will not change the therapeutic decisions.20–22 Nevertheless, most of today's guidelines and recommendations indicate an immediate imaging test–ideally CT without contrast in all patients who come into the ER with RC, even with typical presentation.2,3 This recommendation that can have defensive nuances, seems to be justified by the fact that it is necessary to rule out other processes, in addition to the fact that it confirms ureteral lithiasis and the need for immediate treatment if the calculus is large. However interventions on the urinary tract are not free from complications and medical treatment is considered to be an option, at least during the first 2 weeks. The probability of spontaneous expulsion with medical treatment of a calculus smaller than 5mm is 65%, and 47% if it is between 5 and 10mm, irrespective of its location. Based on its location, distal lithiases are expelled more often and before the proximal ones.23 When a calculus has not been expelled in 4–6 weeks, it is not likely to be expelled and hence indicative of intervention.12
Performing systematically irradiating radiological tests is more under discussion in higher-risk populations. In children 3% of the studies are performed with CT without contrast when suspicion of RC8 yet today the need for using it systematically because of its greater radiosensitivity is questionable. Another risk group is that of patients with known nephrolithiasis and previous colic episodes, in whom an alternative diagnosis is improbable and CT without contrast will change the therapy in 6.5%24 only yet it increases the accumulated effective dose.8 Finally, there is a lower prevalence of nephrolithiasis among women and their gynecologic symptoms are frequent, on occasions clinically overlapping, that is why they are more often studied with CT than men8 with less diagnostic yield. In some works, up to 58.2% of the CT performed on women did not produce any findings, and the rate of lithiasis rate found (26.8%) was significantly lower than that of men (61.6%).13 It seems reasonable to avoid any systematic use of CT without contrast in these three groups and use alternative strategies.
The calculi that cannot be seen in the ultrasound are usually the smallest ones that are usually expelled spontaneously and this is why their results, in practice, do not vary significantly from those of CT without contrast.25 That is why it has been decided to use ultrasound and simple radiography as an initial option in the general population too reserving CT without contrast for patients with a fever and clinical suspicion of a complicated colic, or in cases when the ultrasound is negative.26 But even the ultrasound and the X-ray might not be necessary at the beginning with patients without a fever who respond well to painkillers which occurred in 76% of the patients of a recent series.11 In this group, complications were minimal and there were no morbidity differences when the imaging examination was delayed for 2–3 weeks. In another study in which the CT outcomes did not change the clinical decisions in patients with clinically overt RC, the authors considered that benefit is marginal and should be avoided.20 For that purpose it has been suggested that it is helpful to develop a rule of clinical decision to minimize the use of CT in patients with RC without jeopardizing their own safety.7,20 A clinical predictive rule was recently developed and validated including five factors associated with ureteral lithiasis: male gender, recent pain, non-black race, nausea and vomiting, and microscopic hematuria.27 Three groups were classified as follows: patients with low, medium and high probability of RC. In the latter group, the probability was close to 90%, and the probability of an alternative diagnosis was very low. In young people and women included in this group it would be justified to avoid using CT without contrast in the ER or to perform such CT with low-dose techniques.
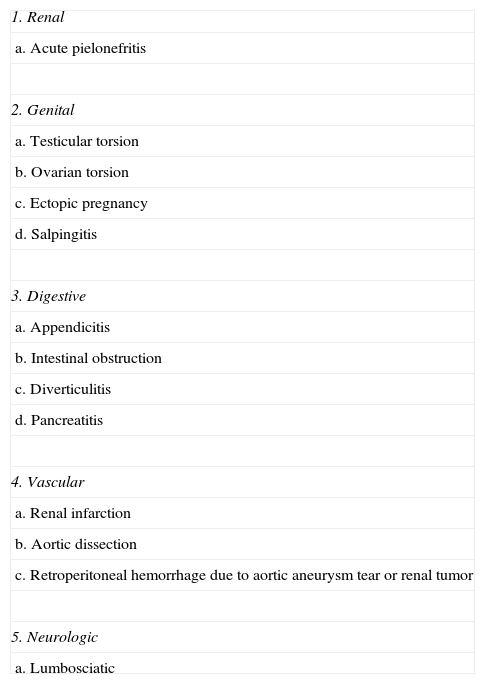
Another argument to use CT in acute lumbar pain is to exclude alternative diagnoses, especially the feared acute aortic syndrome.19 The probability of a non-urinary alternative diagnosis as a cause for colic lumbar pain is usually 10–13%,18,27 though when patients are evaluated with a tool to help in the making of the clinical decision the percentage of patients highly likely to have ureteral lithiasis is ≤3%28 only or <0.3–1.6%.27
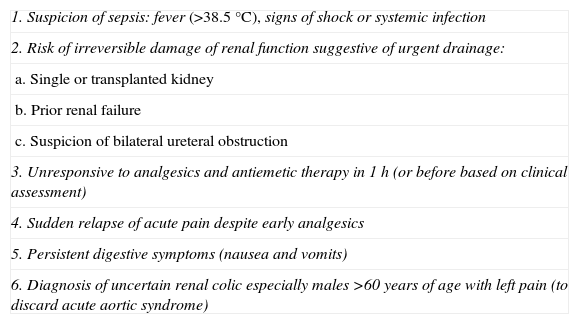
In most patients, colic diagnosis is clinical. With typical pain and hematuria, and a good response to treatment, clinical and radiological correlation is a close one and the emergency imaging tests do not change the initial management,20 the probability of spontaneous expulsion is 70–90% and functional recovery complete when the obstruction resolves in 2 weeks.11 On the contrary emergency tests, CT without contrast or ultrasound based on the clinical context, are clearly indicated in cases of acute lumbar pain suspicious of colic, with a fever, single kidney or pain refractory to treatment, situations where the NICE guidelines recommend hospitalization12 (Table 1). It is also indicated in cases where clinical presentation is atypical and can simulate other processes making it necessary to include ureteral lithiasis among the possible causes of abdominal pain16,18 (Table 2).
Urgent indications for image modalities in patients with acute renal coil.
| 1. Suspicion of sepsis: fever (>38.5°C), signs of shock or systemic infection |
| 2. Risk of irreversible damage of renal function suggestive of urgent drainage: |
| a. Single or transplanted kidney |
| b. Prior renal failure |
| c. Suspicion of bilateral ureteral obstruction |
| 3. Unresponsive to analgesics and antiemetic therapy in 1h (or before based on clinical assessment) |
| 4. Sudden relapse of acute pain despite early analgesics |
| 5. Persistent digestive symptoms (nausea and vomits) |
| 6. Diagnosis of uncertain renal colic especially males >60 years of age with left pain (to discard acute aortic syndrome) |
Differential diagnosis of reno-ureteral colic.
| 1. Renal |
| a. Acute pielonefritis |
| 2. Genital |
| a. Testicular torsion |
| b. Ovarian torsion |
| c. Ectopic pregnancy |
| d. Salpingitis |
| 3. Digestive |
| a. Appendicitis |
| b. Intestinal obstruction |
| c. Diverticulitis |
| d. Pancreatitis |
| 4. Vascular |
| a. Renal infarction |
| b. Aortic dissection |
| c. Retroperitoneal hemorrhage due to aortic aneurysm tear or renal tumor |
| 5. Neurologic |
| a. Lumbosciatic |
It is the fastest modality to help identify calcic lithiasis. Although 90% of urinary calculi have been classically considered as radiopaque, the figures of sensitivity and specificity of the abdomen X-ray to detect them are 45–59% and 71–77% respectively. Vision in radiography is made difficult due to intestinal and bone structure overlapping.29 Its sensitivity is especially low in calculi <4mm, and those located in the middle or distal ureter.29 The second difficulty is distinguishing between lithiasis and other intraabdominal calcifications such as phleboliths, vascular calcifications or apendicoliths yet phleboliths usually has a typical radiolucent center in simple radiographies which helps to diagnose them. At present use is recommended for the follow up of ureteral calculi diagnosed through CT or ultrasound, for control purposes of the position of Double J urethral catheters or in combination with ultrasound, especially in cases of RC where there is no hydronephrosis.1
Intravenous urographyFor years the IVU was the diagnostic modality of choice in RC allowing us to identify lithiasis in the excretory duct and repercussions on such duct –location, presence or not of dilatation, extent of obstruction, contrast and nephrogram delay in the excretory duct. However, it has been progressively replaced by CT without contrast, since the work by Smith et al.30 in 1995. Prospective studies have shown similar31–35 or greater36,37 CT without contrast sensitivity figures to that of urography for the detection of urinary lithiasis with greater safety, more rapidly and cost-effectively.
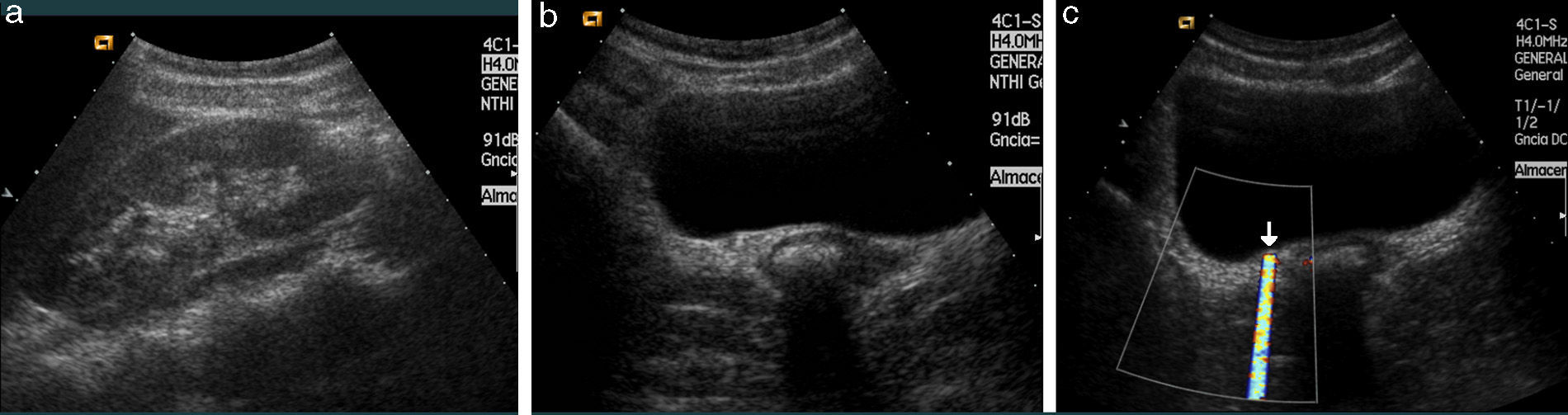
UltrasoundIt is a quick, portable, relatively cheap method that does not use ionizing radiations or require iodized contrast. It allows us to detect lithiasis and, especially, the dilation and degree of dilation of the excretory duct above the obstruction point. It allows us to identify radiotransparent lithiases not visible through simple radiology and even indinavir calculi also not visible through CT (Fig. 1). It also helps find other diseases of the excretory duct, kidney and extrarenal structure that can all simulate a RC.
Patient with left renal colic. (a)–(c) Ultrasound. Calyx lithiasis (a) and (c) and proximal obstructive ureteral lithiasis (b). (d) Computed tomography (CT) without contrast to assess treatment not showing renal or ureteral lithiases but showing indirect signs of renal colic. (e) and (f) After the resolution of the symptoms through ureterorenoscopy with ureteral calculus removal and placement of a pig-tail catheter a CT with contrast examination is performed in the excretory phase showing the lower calyx defect (arrows) corresponding to the image lithiasis (c).
Calculi are identified as hyperechoic focuses with a posterior acoustic shadow. Small lithiases (<5mm) or those located in the middle ureter are especially difficult to see. That explains the wide variation (47.5–98%) in the sensitivity of the ultrasound.38–40 Another limitation of ultrasounds is that several hours must pass until the dilation of the excretory duct; so it can be negative in the initial stage of RC if lithiasis is not identified. The correct hydration of the patient before the proceeding provokes the distension of excretory duct and the adequate filling of the urinary bladder improving the view of the distal ureter.40,41 Combining the “B-mode” with the color and pulsated Doppler methods increases diagnostic yield thanks to other suspicious signs such as twinkling or comet-tail artifact (Fig. 2) of the Doppler color ultrasound allowing us to detect small lithiases that do not get to generate a posterior shadow.42–44 A reduced or asymmetrical ureteral jet and especially the lack of it are also suspicious signs of ureteral obstruction.45 The high intrarenal resistance index (RI) is used as a differential criterion between obstructive and non-obstructive dilation in such a way that >0.7 RI or a difference >10% between the two kidneys is considered diagnostic of obstructive uropathy.46 However, the variability of RI normal values with a trend to increase with age, systolic pressure and decrease of renal function, should be considered.47
Ultrasound of a patient with right RC. (a) Right kidney with minimal ectasia of some calyces–almost indiscernible without other findings. (b) Around the right meatus there is a dubious ureteral lithiasis without evident dilation. (c) Color Doppler. “Twinkling” artifact that helps identify ureteral lithiasis. This artifact occurs in coarse and irregular interfaces reflecting ultrasound waves intensely. It is a rapid alternation of several colors that appear right behind a hyperechogenic image giving the false appearance of movement.
CT is available nowadays in most HES and it is a rapid check-out confirming the calculus, its size and location, as well as hydronephrosis or possible complications. It facilitates the management of patients and shortens the hospital stay time at the HES. Since no IV contrast is needed, it improves its profile of safety since it avoids the risks of renal toxicity and any other possible allergic reactions. The CT without contrast is considered to be the modality that provides the greatest diagnostic yield for the detection of ureteral calculi, with sensitivity and specificity >95% in most recent papers.3 Yield is even better especially in small ureteral lithiases.48,49 In the absence of lithiasis it shows us the recent passage of the calculus or allows us to determine alternative diagnoses, such as acute vascular disease, renal tumors or appendicitis, for which it is usually necessary to administer IV contrast. On the other hand, in cases in which one endourological procedure is indicated, clinical guidelines recommend using multidetector CT with IV contrast to be able to have access to the excretory duct map. Lastly when it comes to the follow-up, it is important that the analysis not only shows the size and location of lithiases but also if they are visible in the topogram, which will allow us to do more follow-up through radiographies.50 To be able to use lithotripsy it is necessary to report on the distance between the lithiasis and the skin.
Dose of radiationBoth the IVU and the abdomen radiography, as well as the CT without contrast lead to exposure to ionizing radiation. The cumulative effect of the doses of radiation together with epidemiological data that half the patients with lithiasis will relapse within the next 10 years suggests a foreseeable significant cumulative radiation dose if this technique is used to diagnose and control these patients.6 The effective dose of a simple abdomen radiography ranges between 0.5 and 1mSv, while that of the IVU ranges between 1.3 and 3.5 or more mSv based on the number of radiographies obtained. The dose of CT without contrast is even higher, around 4.5–5mSv, but in older scanners, especially if a low noise index is required, 10mSv can be surpassed. Low-dose CT without contrast protocols not beyond 3mSv have been proposed for the analysis of patients with RC. With these protocols the diagnostic precision is close to that of conventional CT without contrast, with a sensitivity of 97% and a specificity of 95%.51 Routine use of these types of protocols is recommended except for patients whose body mass index >30kg/m2, in whom it is recommended to use a conventional technique to guarantee the good quality of images.2,52 When contrast is necessary in CT, the radiation dose increases proportionally to the number of phases performed.
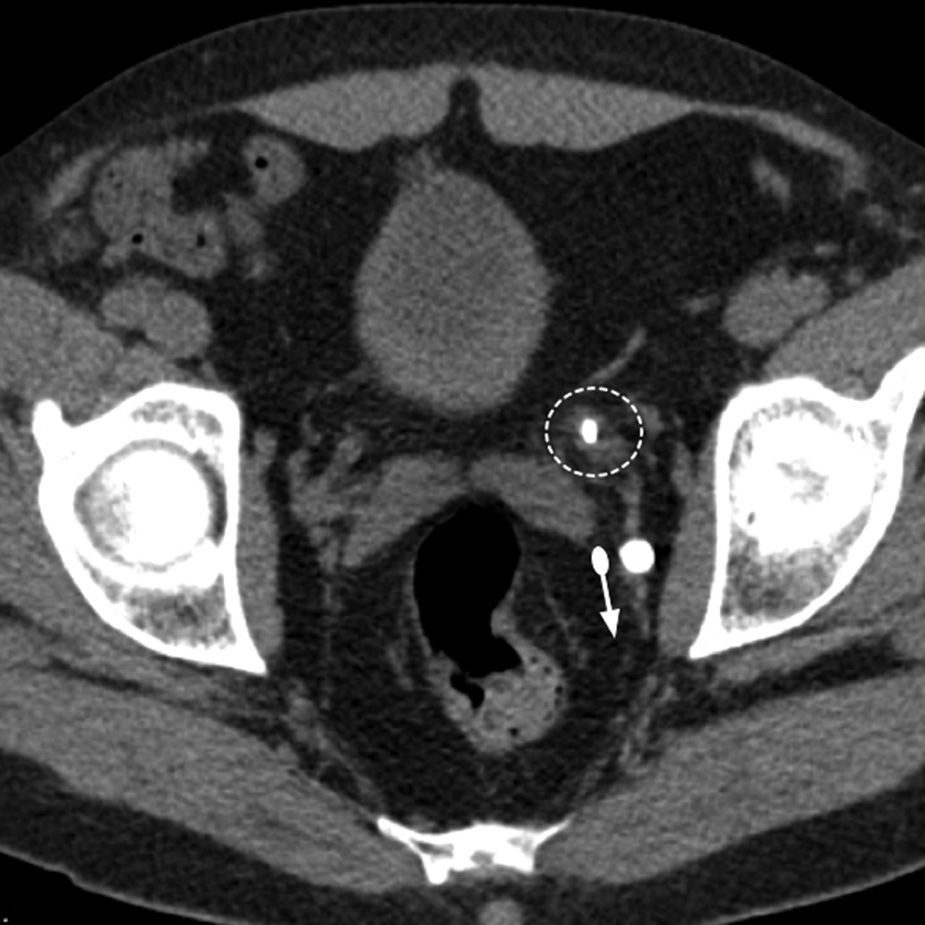
DiagnosisDirect visualization of the calculus is the main CT sign in RC and can usually be identified in most cases. On occasion, it can be difficult to see because of respiratory or metal devices adjacent to the lithiasis, because it is very small or because its composition is “CT-lucid”. The latter occurs with certain infective lithiases made up of proteinaceous material or in lithiases secondary to some antiretroviral drugs in HIV patients.53 When the calculus is located in the distal ureter, it can be difficult to differentiate from a phlebolith, especially if fine sections are not available. In this case the “halo” and “comet tail” signs are useful (Fig. 3). The former refers to the padding of soft parts around the lithiasis, caused by the edematous ureteral wall,54 and the latter, described as typical of phleboliths, consists of the observation of a tail of soft tissue density corresponding to the venous vessel.55 When it is not possible to differentiate them IV contrast in the excretory phase is necessary to be able to see the ureteral pathway.
Computed axial tomography without contrast of a patient with left RC. Two pelvic calcifications are identified. One of them corresponds to an obstructive distal ureteral lithiasis showing a discontinued circle (halo sign) formed by the edematous ureteral wall around the lithiasis. Another larger and posterior calcification is a phlebolith with the comet tail sign, corresponding to a posterior trail made up of the vessel where the phlebolith is (parallel to the arrow).
Like in ultrasound there are indirect signs that increase the CT diagnostic yield, whose relevance is greater when lithiasis is not identified for the reasons aforementioned or because it has already been expelled. These signs do not usually appear until 6h before the beginning of the obstruction, and they include excretory duct dilation, change in ureteral caliber, perirenal and periureteral fat stringiness, renal edema, the presence of other non-obstructive renal lithiases and delays in uptake and excretion if IV contrast has been administered.
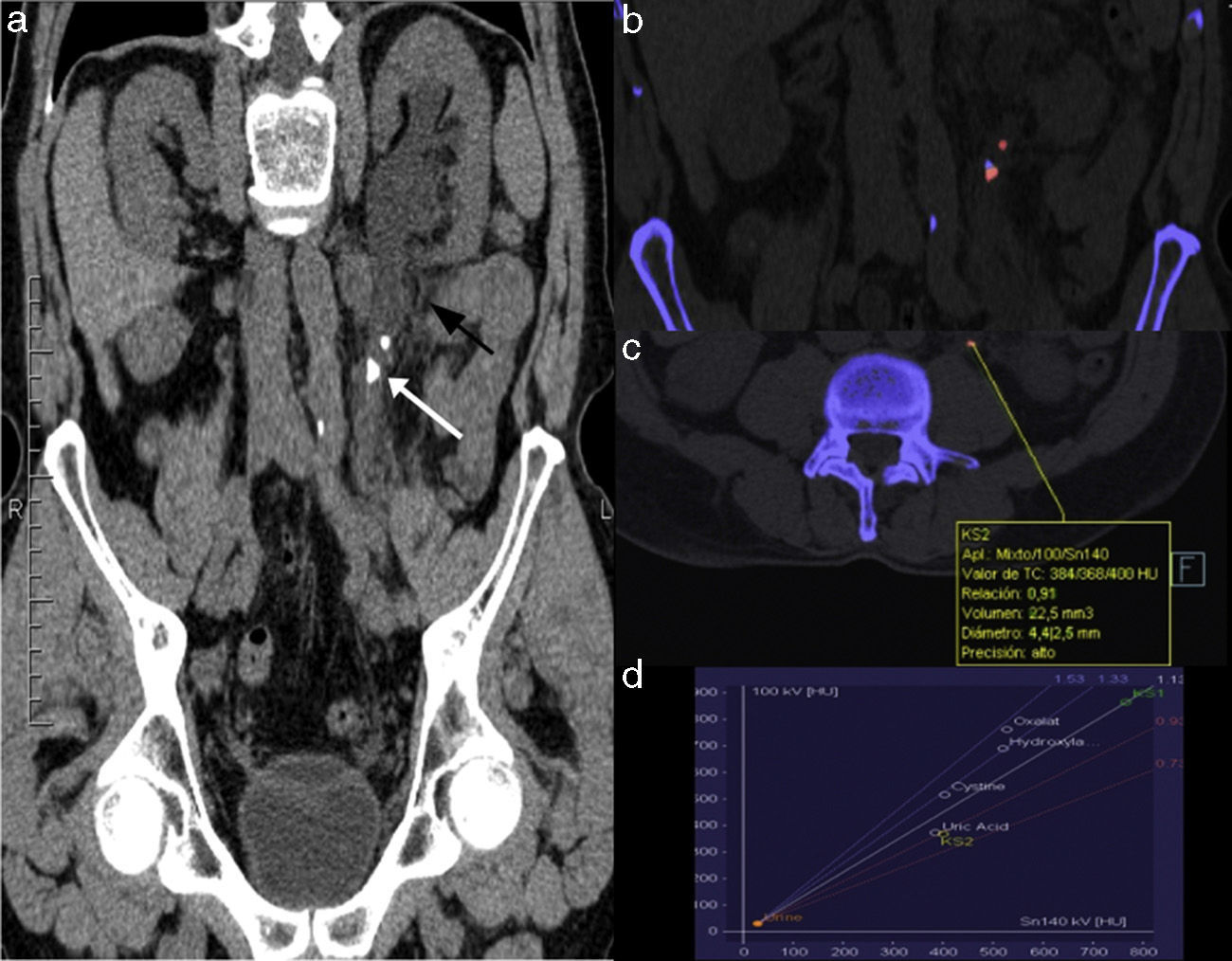
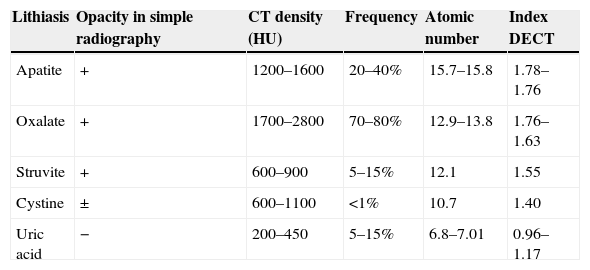
Analysis of the lithiastic compositionIn addition to identifying lithiasis, CT also provides information about its composition, which is useful to determine treatment. Uric acid and xanthine lithiases are radiotransparent and cannot be identified through a simple abdomen radiography and can only be detected indirectly through the IVU as filling defects. Although they can be seen well with CT without contrast, its density is lower than that of the rest (Table 3). Nevertheless, there is great density overlapping especially in uric acid lithiases compared to the rest that do not allow us to identify them in vivo.56
Lithiasic composition through DECT.
| Lithiasis | Opacity in simple radiography | CT density (HU) | Frequency | Atomic number | Index DECT |
|---|---|---|---|---|---|
| Apatite | + | 1200–1600 | 20–40% | 15.7–15.8 | 1.78–1.76 |
| Oxalate | + | 1700–2800 | 70–80% | 12.9–13.8 | 1.76–1.63 |
| Struvite | + | 600–900 | 5–15% | 12.1 | 1.55 |
| Cystine | ± | 600–1100 | <1% | 10.7 | 1.40 |
| Uric acid | − | 200–450 | 5–15% | 6.8–7.01 | 0.96–1.17 |
HU, Hounsfield units; DECT, double energy CT.
The CT modality with double energy, whether with a single source (alternating the energy or performing a double study at different energies) or with a double source (double tube) allows us to differentiate materials of similar density through the absorption variation at different energies.57,58 Most lithiases have a greater density when kilo voltage kV) is lower (80–100kV). On the contrary, uric acid calculi are attenuated in a similar way both spectra, or even more in those of greater kV (Fig. 4). This difference, quantifiable through the double energy index allows us to distinguish uric acid lithiases from the rest,59 even using low-dose protocols.60–62
Computed tomography without contrast with double energy of a patient with symptoms of left RC. (a) Curve coronal reconstruction following the ureteral tract. The white arrow shows a proximal obstructive ureteral lithiasis. The perirenal and periureteral fat shows stringiness (black arrow). (b) Coronal image of application for renal lithiasis once the double energy information is processed showing a mixed composition of the obstructive lithiasis (red=uric acid, blue=not uric acid) and a pure uric acid composition of the proximal non-obstructive ureteral lithiasis. (c) and (d) Quantification of the pure uric acid lithiasis composition showing double energy relation <1 (0.91) and a location in the graph corresponding to uric acid lithiasis (KS2). The color in this figure is visible only in the electronic version of this article.
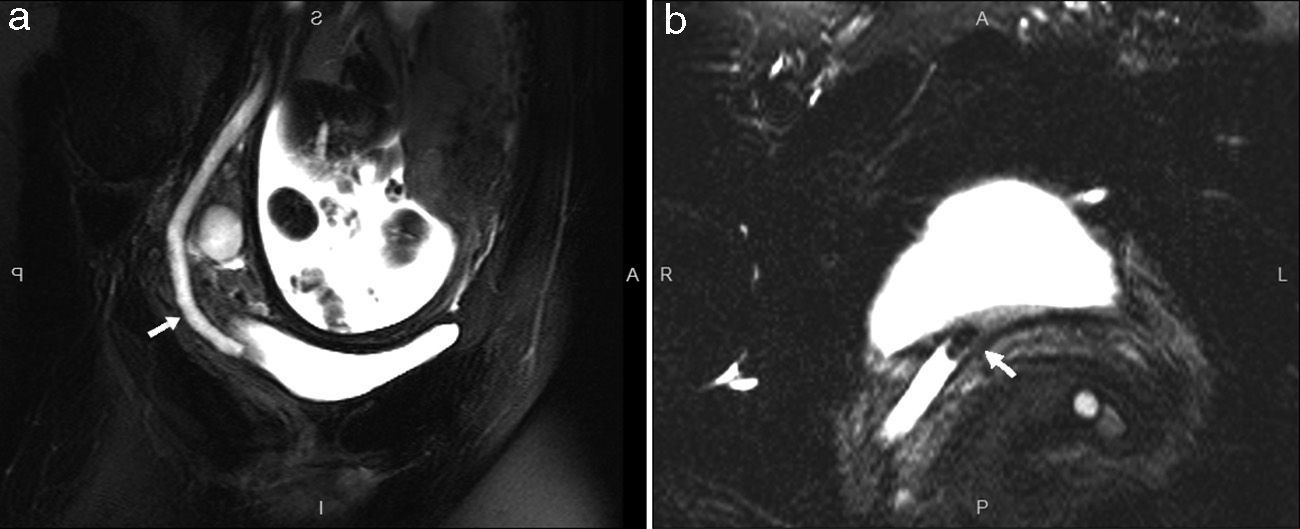
The uro-MR, especially the sequences that are highly T2-weighted allows us to detect excretory duct dilation63,64 and distinguish pregnancy physiological hydronephrosis from that secondary to lithiasis. Although lithiases can go unnoticed, when the urinary tract is dilated they are usually identified as filling defects with signal void (Fig. 5). MRIs are a good alternative to CT for pregnant women with negative or non-conclusive ultrasound result yet its safety is not proved in the first quarter, its use is arguable and it must only be indicated after the assessment of the risk-benefits ratio. On the other hand, the availability of MR machines for emergency studies is very limited.
Magnetic resonance in a 20-week pregnant patient with right renal colic. (a) Coronal reconstruction showing ureter dilation (arrow) up to the pelvis. (b) T2-weighted axial sequence showing dilated distal ureter with juxtavesical intraureteral signal void image corresponding to lithiasis (arrow).
The tendency in all HES is to indicate imaging examination for all RC patients. CT is the modality with the best diagnostic yield and in many centers it has become the initial test to assess the index RC. Using imaging modalities systematically in patients suspicious of RC and typical clinical presentation does not change management significantly.20–22 Its use should be limited to patients who do not show any clinical improvement after treatment, in cases of fever or leukocytosis, in patients with a single kidney or with renal failure, or in high-risk populations.1,9,12 If CT without contrast is performed low-dose techniques should be used. Although the ultrasound is inferior to the CT for the detection of lithiasis, it would be reasonable to use it as an initial method especially in younger patients where the probability of an alternative serious diagnosis is lower.26,65,66 Lower cost, greater availability, absence of ionizing radiations and the fact that in most cases therapeutic management will not change, even in those cases where the ultrasound has not identified lithiasis, are other arguments in favor of the ultrasound.1,24 In older patients with persistence of clinical signs, especially if the initial ultrasound examination is negative, the CT would be indicated. Although in all the cases the first step can be to resort to ultrasound, its use is compulsory in children and young people as well as in pregnant and fertile women. When it is not conclusive, CT without contrast allows us to identify ureteral lithiasis with great precision and to investigate possible alternative diagnoses. If CT without contrast is negative for lithiasis and there are no signs of a recent passage of a calculus it is recommended to administer an IV contrast, once any other medical contraindication have been excluded (history of anaphylaxis, renal failure or dehydration due to vomiting). In women in their 2nd and 3rd quarters of pregnancy if available MRI should be the 2nd-choice image modality.
Ethical responsibilitiesProtection of people and animalsAuthors confirm that no experiments have been performed on human beings or animals.
Data confidentialityAuthors confirm that the protocols of their institution have been followed on the publication of data from patients.
Right to privacy and informed consentAuthors confirm that in this report there are no personal data from patients.
Author contributionManager of the integrity of the study: CN.
Original idea of the study: CN.
Study design: CN, JMA.
Data mining: not applicable.
Data analysis and interpretation: not applicable.
Statistical analysis: not applicable.
Reference search: CN, RS, JMA.
Writing: CN, RS, JMA.
Manuscript critical review with intellectually relevant contributions: CN, RS, JMA.
Final version approval: CN, RS, JMA.
Conflict of interestAuthors reported no conflict of interest.
Please cite this article as: Nicolau C, Salvador R, Artigas JM. Manejo diagnóstico del cólico renal. Radiología. 2015;57:113–122.