Chronic venous insufficiency of the lower limbs is very prevalent.
In recent decades, Doppler ultrasound has become the method of choice to study this condition, and it is considered essential when surgery is indicated.
This article aims to establish a method for the examination, including venous mapping and preoperative marking. To this end, we review the venous anatomy of the lower limbs and the pathophysiology of chronic venous insufficiency and explain the basic hemodynamic concepts and the terminology required to elaborate a radiological report that will enable appropriate treatment planning and communication with other specialists.
We briefly explain the CHIVA (the acronym for the French term “cure conservatrice et hémodynamique de l’insuffisance veineuse en ambulatoire”=conservative hemodynamic treatment for chronic venous insufficiency) strategy, a minimally invasive surgical strategy that aims to restore correct venous hemodynamics without resecting the saphenous vein.
La insuficiencia venosa crónica (IVC) de las extremidades inferiores es una enfermedad muy prevalente.
La ecografía Doppler se ha establecido en las últimas décadas como el método de elección en el estudio de esta patología, por lo que resulta imprescindible ante una eventual indicación quirúrgica.
El objetivo de este trabajo es establecer una metodología en la exploración, incluyendo la realización de cartografía y el marcaje prequirúrgico. Para ello revisaremos la anatomía venosa de los miembros inferiores y la fisiopatología de la IVC explicando los conceptos hemodinámicos básicos y la terminología necesarios para la realización de un informe radiológico que permita una adecuada planificación terapéutica y comunicación con otros especialistas.
Explicaremos brevemente la estrategia CHIVA (cura hemodinámica de la insuficiencia venosa ambulatoria), método quirúrgico mínimamente invasivo que tiene como objetivo restaurar la hemodinámica venosa sin extirpar la vena safena.
Chronic venous insufficiency (CVI) is the set of symptoms and signs derived from venous hypertension in the lower extremities due to poor valvular function of the venous systems.1,2
CVI is the most frequent vascular disease; it affects 20–30% of the adult population and 50% of people over 50 years of age, with a prevalence in Spain of 48.5% of men and 58.5% of women.3
It is suffered in different degrees of seriousness, and it is a problem of public health with significant socio-economic and labor implications. It is the cause for 2.5% of medical leaves in some of our neighboring countries and overall it consumes up 2% of the public health budget.4
Every venous insufficiency is the consequence of avalvulation, which results primarily (essential varicose veins) from the affectation of the superficial venous system and perforator veins, or secondarily (post-phlebitic or post-thrombotic) due to valvular destruction occurring in the deep venous system as a consequence of post-thrombotic recanalization.5
The clinical manifestations of CVI include a wide range of manifestations from initial symptoms such as heaviness, pain or edema; varicose disease, when the varicose veins become visible, above all with orthostasim, to late symptoms, with changes in skin coloration and trophic disorders that can trigger complications (varicophlebitis, varicorrhage, increase in the cicatrization time of leg wounds, dermitis and trophic ulcers).6
Doppler ultrasound is the only non-invasive procedure capable of providing an anatomic and hemodynamic topography for venous circulation of the lower extremities in real time, therefore it is the diagnostic method of choice.
Ever since the appearance of Doppler ultrasound, and progressively, phlebography has come into disuse, since it is an invasive procedure, which uses IV contrast and ionizing radiations, and it has complications associated.
The systematic use of phlebography with CT and phlebography with MRI is not justified today in the study of CVI, and their indications are restricted to a select group of patients, especially: cases of venous insufficiency of unusual cause that manifest themselves in a complex manner, one that is not cleared up by Doppler examination: varicose veins of pelvic or abdominal origin, unusual anatomic variants or vascular malformations, and recurrent varicose veins of unclear etiology.1,7–9 An adequate ultrasound study, including mapping and pre-surgical marking, is essential for the surgeon to plan treatment and it has allowed us to lay the foundations of conservative treatment of CVI.10
The CHIVA method is a minimally invasive surgical technique for the treatment of varicose veins. The goal of this surgery is to eliminate veno-venous derivations through disconnection of the escape points, preserving the saphenous vein and normal venous drainage of the superficial tissues of the limb. To obtain optimal results, it is necessary for the valvulo-muscular pump to work properly and to guarantee the integrity of the deep venous system.
Other therapeutic possibilities in the treatment of varicose veins are stripping (classical surgical treatment with ligation of the arch and saphenectomy), sclerotherapy and endovascular therapy (radiofrequency or endolaser).
Regardless of the surgical technique used, the initial Doppler study is necessary to establish therapeutic indication, know the origin of the varicose collaterals and what the hemodynamic pattern causing them is. When we use the CHIVA technique, immediate pre-operative marking is essential.
The goal of this article is to establish a methodology in Doppler ultrasound study in CVI and venous mapping and pre-surgical marking.
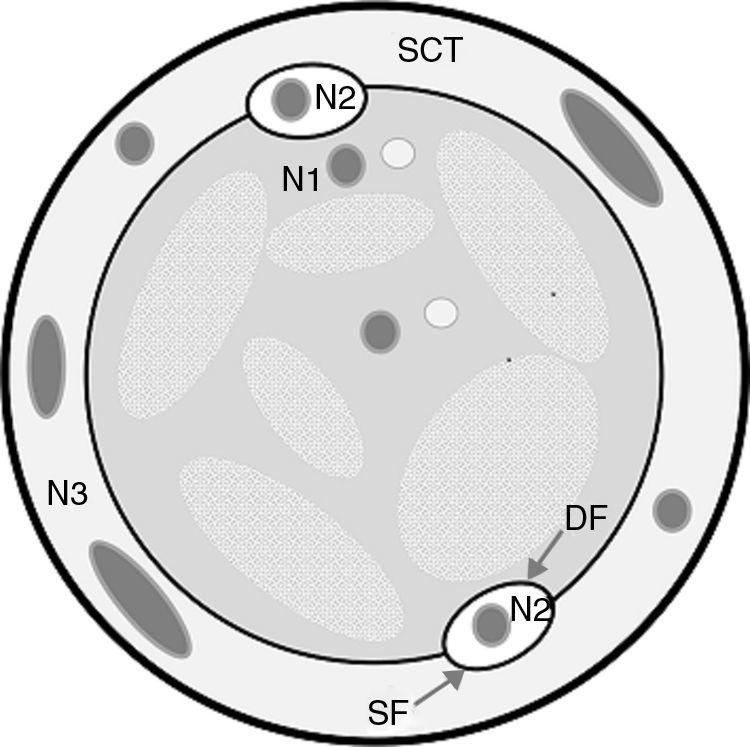
AnatomyThere are two venous fasciae, both hyperecogenic and easily identifiable: the muscular or deep fascia, covering the muscular planes, and the superficial or venous fascia outlining the subcutaneous cellular tissue.11,12 This allows us to delimit venous networks (Fig. 1):
- •
N1 or primary network: deep with respect to the muscular fascia. This is where the deep venous system (DVS) lies which runs parallel to the arteries from the foot to the thigh. It is made up of plantar veins, the tibial veins, the popliteal vein and the femoral vein. The sinusoids located within the muscle at calf level are the soleus and the gastrocnemius veins are important too.
- •
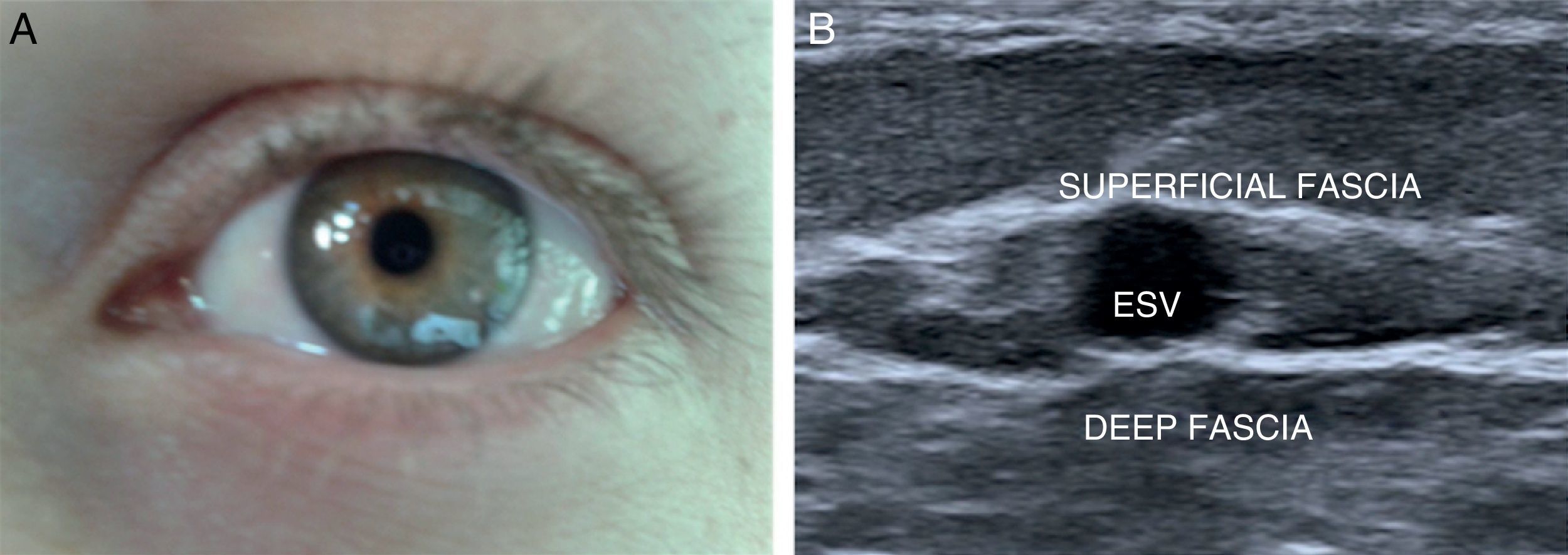
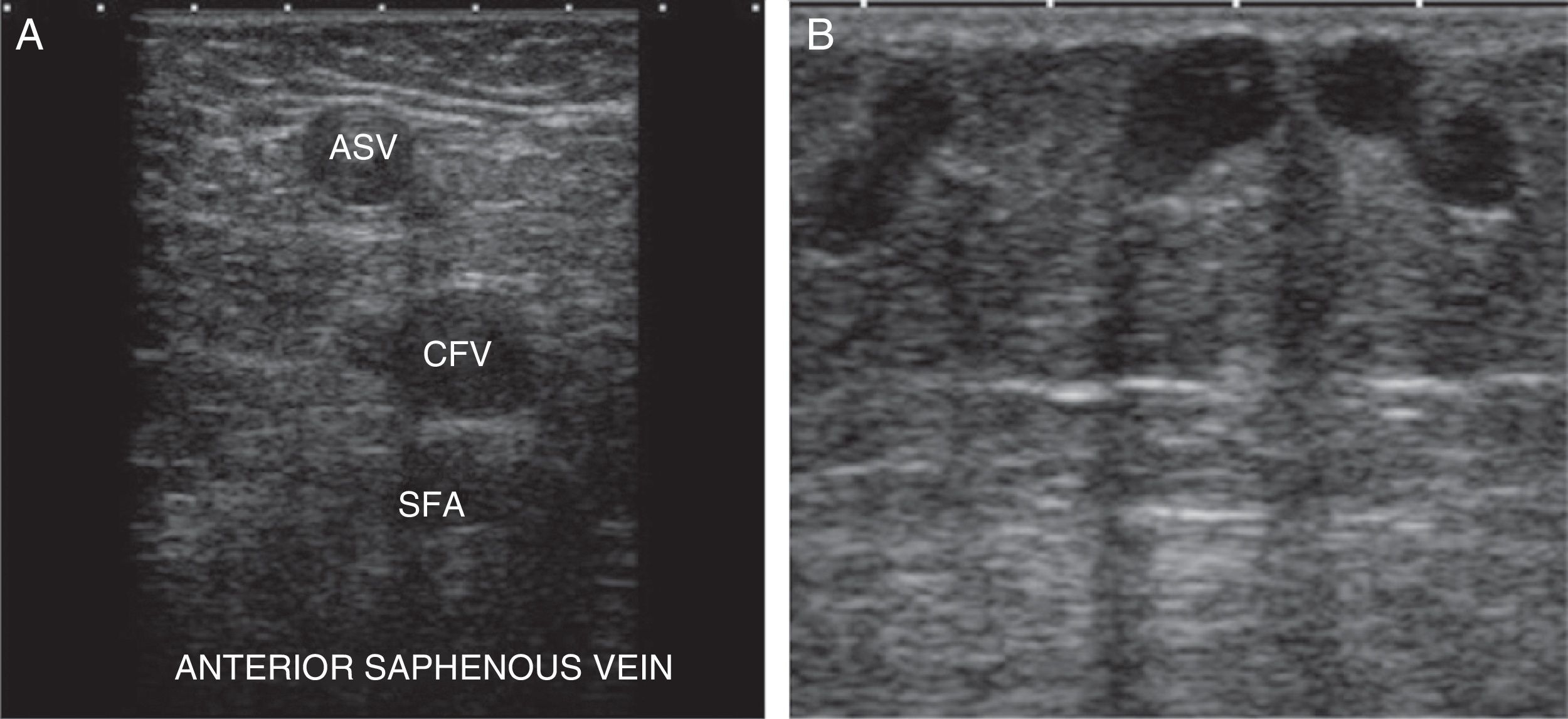
N2 or secondary network: between both fasciae (sign of the eye) (Fig. 2). The superficial venous system is located here and it is made up of the internal saphenous vein (ISV), the external saphenous vein (ESV), and their anatomical variants (anterior saphenous and Giacomini veins) (Fig. 3A).
The ISV is the most important trunk of the superficial venous system. It originates in the anterior side of the internal malleolus and it runs from the leg to the groin through the inner side of the thigh, to drain through its arch into the DVS (common femoral vein, CFV).
The ESV originates behind the external malleolus and runs all the way up the mid line of the calf, draining into the DVS at the level of the popliteal vein. In approximately one third of the cases, it continues up toward the ISV through the Giacomini vein, or else it drains into the DVS through a perforator vein.
- •
N3 or tertiary network: it is made up of veins located outside the superficial fascia. They usually correspond to branches of the saphenous veins or those originating from the perforator veins (Fig. 3B).
- •
N4 or quaternary network: it is a special type of N3 connecting two N2. They can be longitudinal (N4L) if they communicate with the same N2 or transversal (N4T) if they communicate two different N2.
Varicose bundles are mainly made up of dilations or tortuosities of N3 and N4.
N2 and N3 communicate with N1 through the arches or perforator veins.
Physiology, physiopathology and hemodynamic conceptsPhysiologyThe venous system acts as a blood reservoir and it carries blood from the capillaries to the heart, against gravity and without a pump of its own; therefore, it is necessary for the venous system to be patent, there must also be integrity of the valvular system and a preserved heart function.
Physiopathology11,12Venous insufficiency is defined as the incapacity of a vein to pump blood flow and return it to the heart, adapted to the needs of drainage regardless of its location and activity. It is due to the obstruction of drainage or the existence of reflux, or a combination of both.
Hemodynamic concepts11 (Fig. 4)- •
Antegrade flow: in the physiologic direction of the vein.
- •
Retrograde flow: contrary to physiological direction.
- •
Leakage point: passage from an inner to an outer compartment.
- •
Entry point: passage from an outer to an inner compartment.
- •
Reflux: flow that returns in a direction contrary to the physiological direction; it assumes a previous flow in the normal direction (reflux is bidirectional).
- –
Reflux criteria: retrograde flow during muscular relaxation for more than 0.5s or less if the speed is greater than the antegrade speed obtained during muscular relaxation.13
- –
- •
Valvular competence/incompetence: it refers to the function of the valves; it does not necessarily presuppose the direction of the flow.
- •
The phenomenon of venous insufficiency can be defined as a veno-venous shunt or retrograde circuit formed by a leakage point (e.g., the sapheno-femoral junction), a usually retrograde trajectory (varicose veins) and a re-entry point into the DVS (through perforator veins). They can be either open or closed based on whether blood recirculates inside or not. Closed shunts will cause system overload.
Veno-venous shunts can be activated during muscular relaxation or contraction and they must be differentiated from other conditions that can occur in similar ways. A clear example is the vicariate shunt or collateral circulation shunt10 occurring in patients with acute venous thrombosis or un-recanalized poorly collateralized post-phlebitic syndrome that can lead to venous hypertension manifestations without reflux. They are created to compensate a DVS obstacle, and the SVS acts as a bridge or collateral for blood return; it shows continuous activity in systole (contraction) and diastole (muscular relaxation).
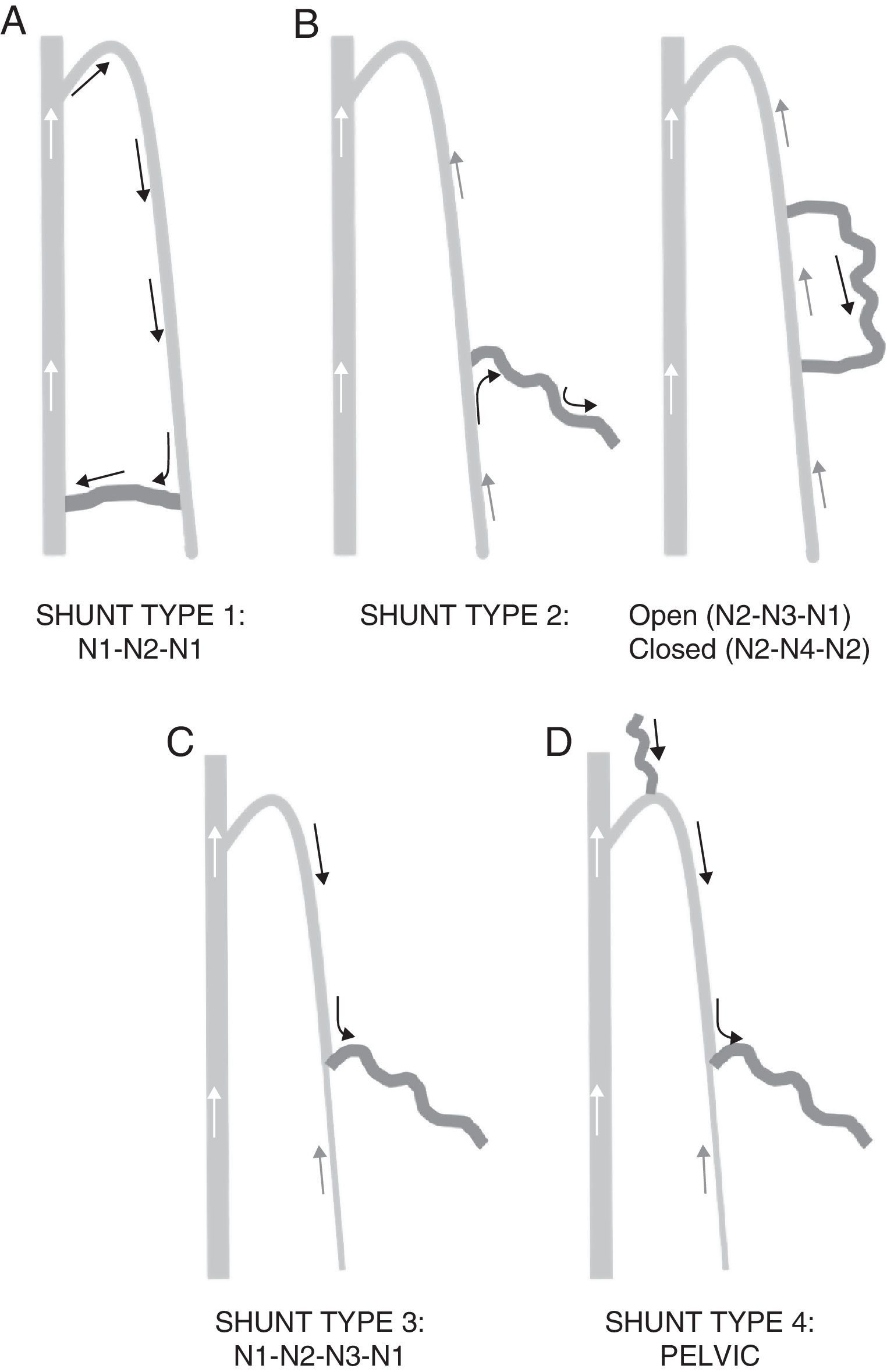
Types of shunts:
They are classified based on their points of leakage and re-entry, and the trajectory described between one and the other (Fig. 5).
- •
Type 1 Shunt: N1-N2-N1. The leakage point is established between the deep venous system and the saphenous vein (in the arch or through perforator veins). It originates a retrograde saphenous vein with re-entry through a perforating vein located in the same saphenous vein. It is a closed shunt. There is no overlapped collateral.
- •
Type 2 Shunt: the leakage point originates in the saphenous vein itself. They can be open (if the collateral flows into a perforator veins into the deep system, N2-N3-N1) or closed (collateral flows into the saphenous vein, N2-N4-N2).
- •
Type 3 Shunt: N1-N2-N3-N1. Like type 1, with a collateral overlapped between the maximum energy column and re-entry. Closed.
- •
Type 4 Shunt. All the shunts not included in the above categories. Basically of pelvic origin (N3-N2-N3-N1).
In the 1980s Francesci14 described a procedure for treating CVI based on acting on the hemodynamic elements that determine the appearance of varicose veins, with preservation of the superficial venous network.
This procedure has had a significant growth in the last decade in our country due to its good post-operative recovery and few complications.15
It is not a technique, but a strategy based on12:
- •
fragmentation of the pressure column;
- •
Interruption of the veno-venous shunts by disconnecting the leakage points.
- •
Preservation of the saphenous and the re-entry perforating veins, preserving normal venous drainage of the leg superficial tissues.
- •
Suppression of the undrained N3-N4.
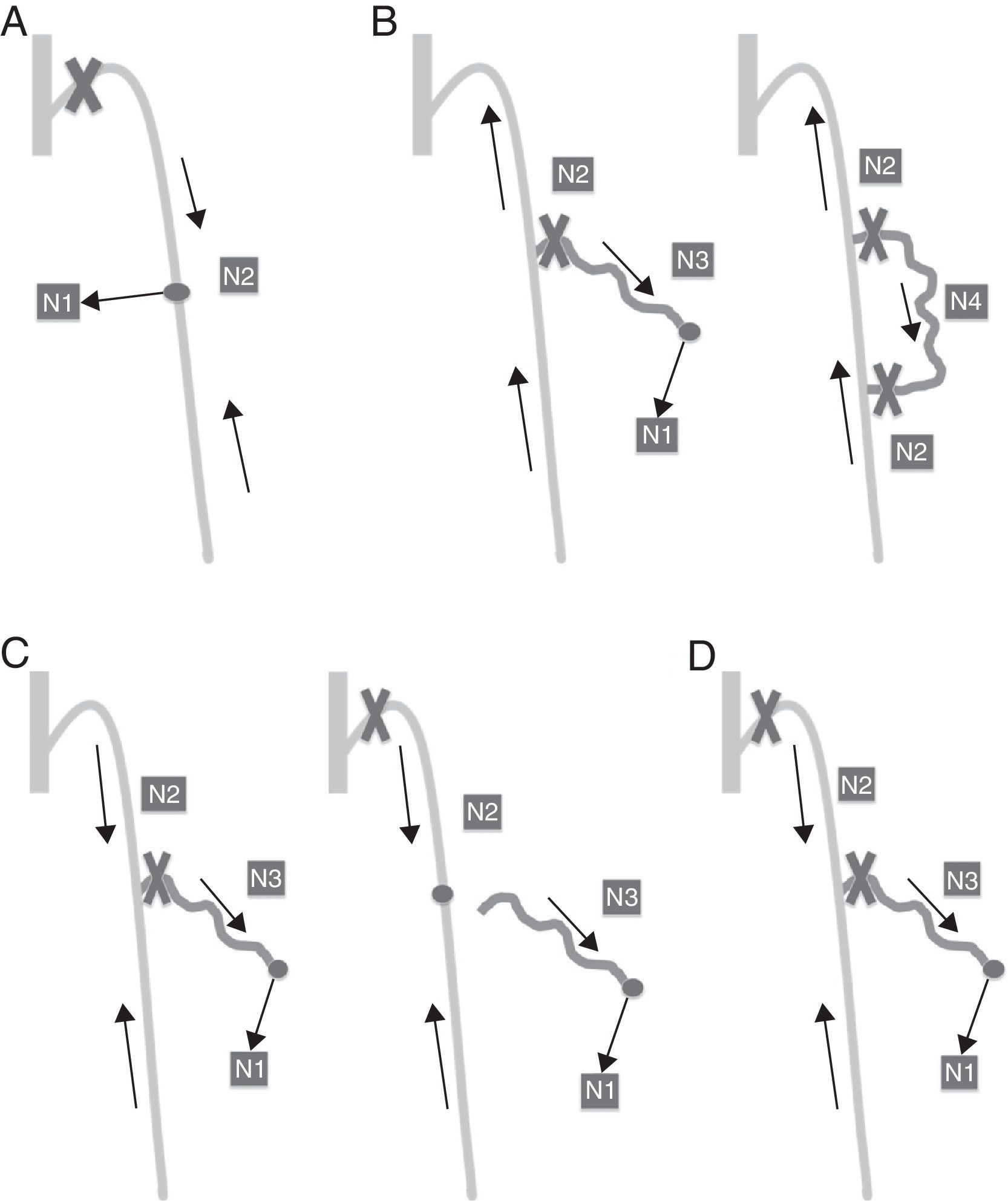
Forms of application (Fig. 6):
- •
CHIVA 1: in only one time without creating hemodynamic affectation and obtaining a drained system. Shunt Types 1, 2 and 4. The suppression of the main leakage point can be done at the same time it acts upon the eventual N3.
- •
CHIVA 2: strategy in two times. Type 3 Shunts.
- –
In the first time it acts upon N2-N3 leakage point (the saphenous vein develops a new re-entry perforating vein on N2 transforming the Type 3 shunt into a Type 1 shunt).
- –
In the second time the N1-N2 leakage point is closed.
- –
It requires periodic Doppler controls and it is counterindicated in cases where the caliber of the saphenous vein is greater than 1cm, due to the risk of thrombosis and potential complications when the arch is left open.
- •
CHIVA 1+2: Type 3 shunts. In only one surgical act it generates hemodynamic conflict by compromising the system drainage; it suppresses the leakage points without organizing drainage.
On some occasion it develops neo-N3.
The intervention is usually performed on one limb only.
It has a certain number of advantages compared to other more aggressive surgical techniques like stripping (removal of veins), such as a local anesthesia as opposed to rachideal anesthesia, fewer complications, immediate walking after the intervention and a faster come-back to work meaning lower socio-economic costs.15,16
There is no statistically significant difference between the healing percentages after 5 years of follow-up with both techniques.17
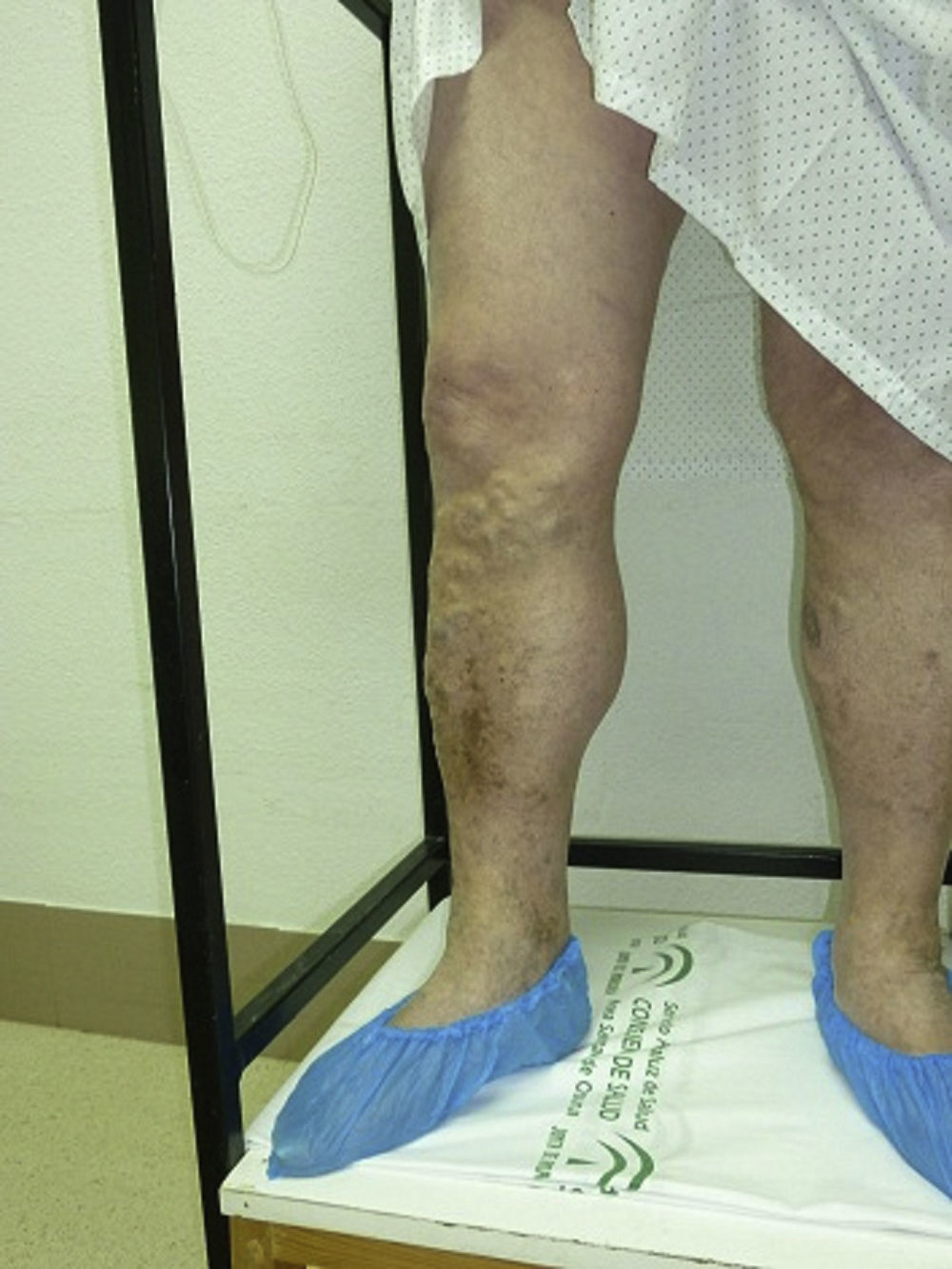
Exploratory techniqueIndications2,18The main indication is for all those patients with symptomatic varicose veins or trophic disorders (ulcers, dermatitis, atrophy, etc.) eligible for surgery (Fig. 7), to guide therapeutic decision, and for patients with edema or leg pains of uncertain origin.
Patients with vascular spiders or telangiectasis do not need to be assessed through Doppler ultrasounds.
Technical requirements- •
B-mode ultrasound and color and pulsed wave Doppler.
- •
High-frequency linear transducer (7.5–13MHz) to obtain good-quality images of the superficial veins and sector transducer (3.5–5MHz) useful for the assessment of the deep venous system in thick or edematous legs.6
- •
A stool and platform for the study of bidepalism.
The main goal of the venous Doppler is to confirm vascular patency, identify the type of venous insufficiency, determine the types of veno-venous shunts, identify the leakage and re-entry points, and perform venous mapping.
This study will allow us to decide which is the ideal treatment for each patient.12
SystematicFirst of all, it is important to perform an anamnesis to know the patient's symptoms, and a physical examination of the limb to be examined in a well-lit room in order to establish the location and distribution of the varicose veins. We will be looking for previous surgeries. This is how we will be able to optimize the study and predict the origin of the reflux.19
Secondly, with the patient lying in the supine position we will assess the DVS from the CFV up to the popliteal vein and the bifurcation of the tibial-peroneal trunks to ensure its patency and competence.19
It is important to analyze the morphology of the spectral wave with pulsed Doppler at the level of the CFV, which should be phasic and should be modified with breathing to rule out a possible proximal obstruction in the iliac axis. This is how we will rule out that reflux in the internal saphenous vein is due to a vicariant flow.2,10
The existence of reflux in the common femoral and the popliteal veins should be assessed a few centimeters above the sapheno-femoral or sapheno-popliteal junction.
Next we will assess the superficial venous system with the patient standing on a platform, with his leg in abduction and external rotation, with his weight being supported by the opposite leg. It is an essential that the study is performed with a stand-up patient.2,10–12,18,19
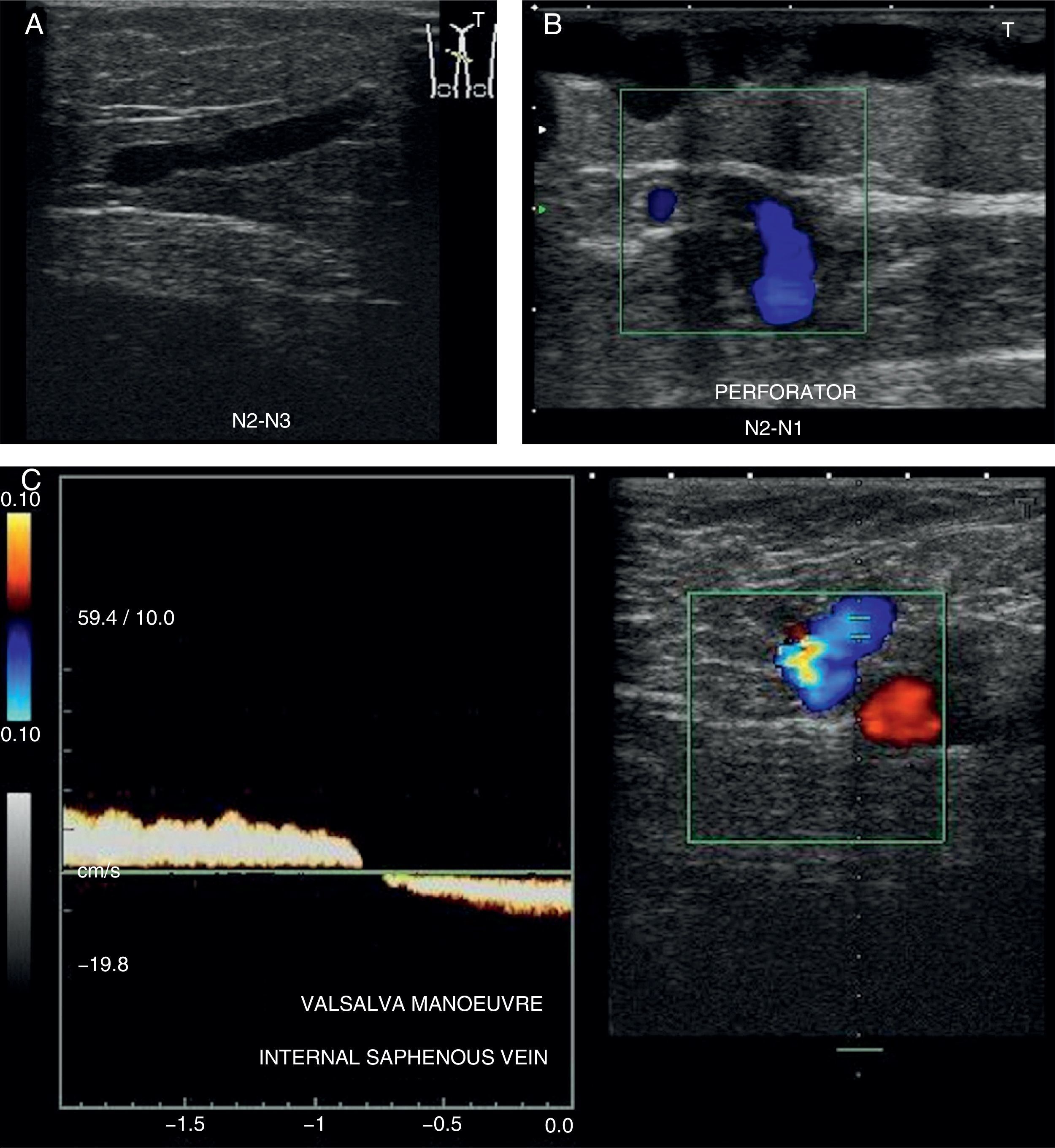
To confirm the presence of reflux we will use these manoeuvers:
- •
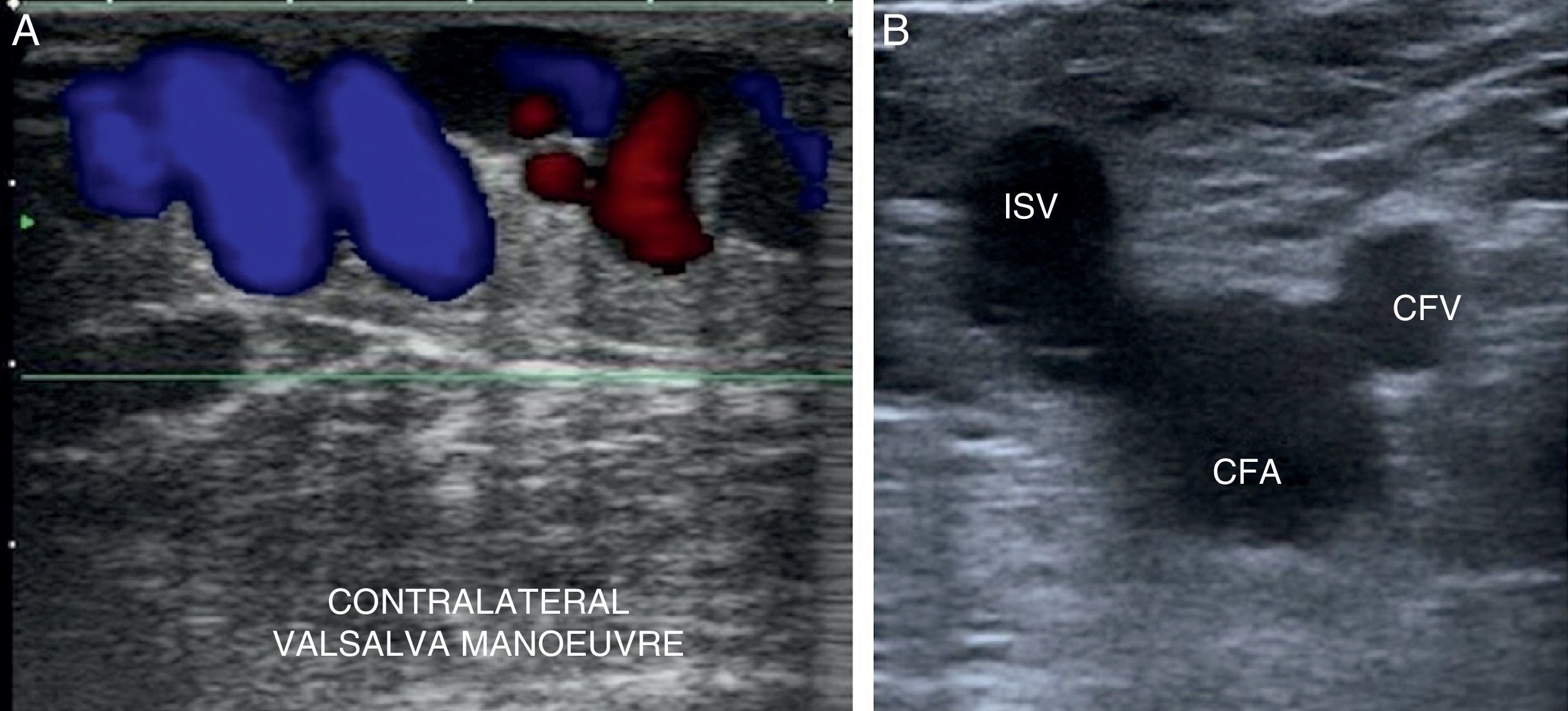
Valsalva manoeuver: increasing thoraco-abdominal pressure2,10,11,18 (Fig. 8A).
- •
Paraná manoeuver: the patients is pushed and he contract his muscles to keep balance and then relaxes the muscles.
- •
Distal compression/relaxation manoeuver2,6,10,12: performing distal compression until the flow disappears; the reflux is considered positive when upon stopping the compression the inverted flow is detected by showing a change of color and inversion of the spectral curve19,20 in transversal slices and with color Doppler.
Transient retrograde reflux is normal and it occurs with valvular closure.
We will begin the study at the level of the sapheno-femoral junction in B-mode (Mickey Mouse sign) (Fig. 8B).
At this point we should look for the possible cause of reflux, which in most cases is caused by incompetence at the level of the sapheno-femoral junction.21
The most common cause of reflux immediately distal to this point is incompetence of the tributary vein of the lower abdomen or pelvis (superficial epigastric vein and external pudendal vein),19,21 especially in multiparous women10,19,21 (type 4 shunt). Vulvo-perineal varicosities are significantly associated with pelvic congestion syndrome.21
Approximately 3cm from the junction, the calibers of both saphenous veins should be measured, which in normal conditions should be less than 3–4 mm.18,19 This measurement will influence the therapeutic decision and can be used as a reference for further examinations. Although it is not an absolute counterindication one saphenous diameter>10mm means the CHIVA procedure should not be used because of a possible postoperative symptomatic thrombosis.15
The presence of reflux is usually associated with an increase in the diameter of the venous structure.
Next we will assess possible caliber changes looking for leakage points and the location and distribution of varicose veins, as well as possible re-entry points (through perforator veins into the DVS or the secondary network (N4)).
We will use the same systematics to study the great saphenous vein and the small saphenous vein.
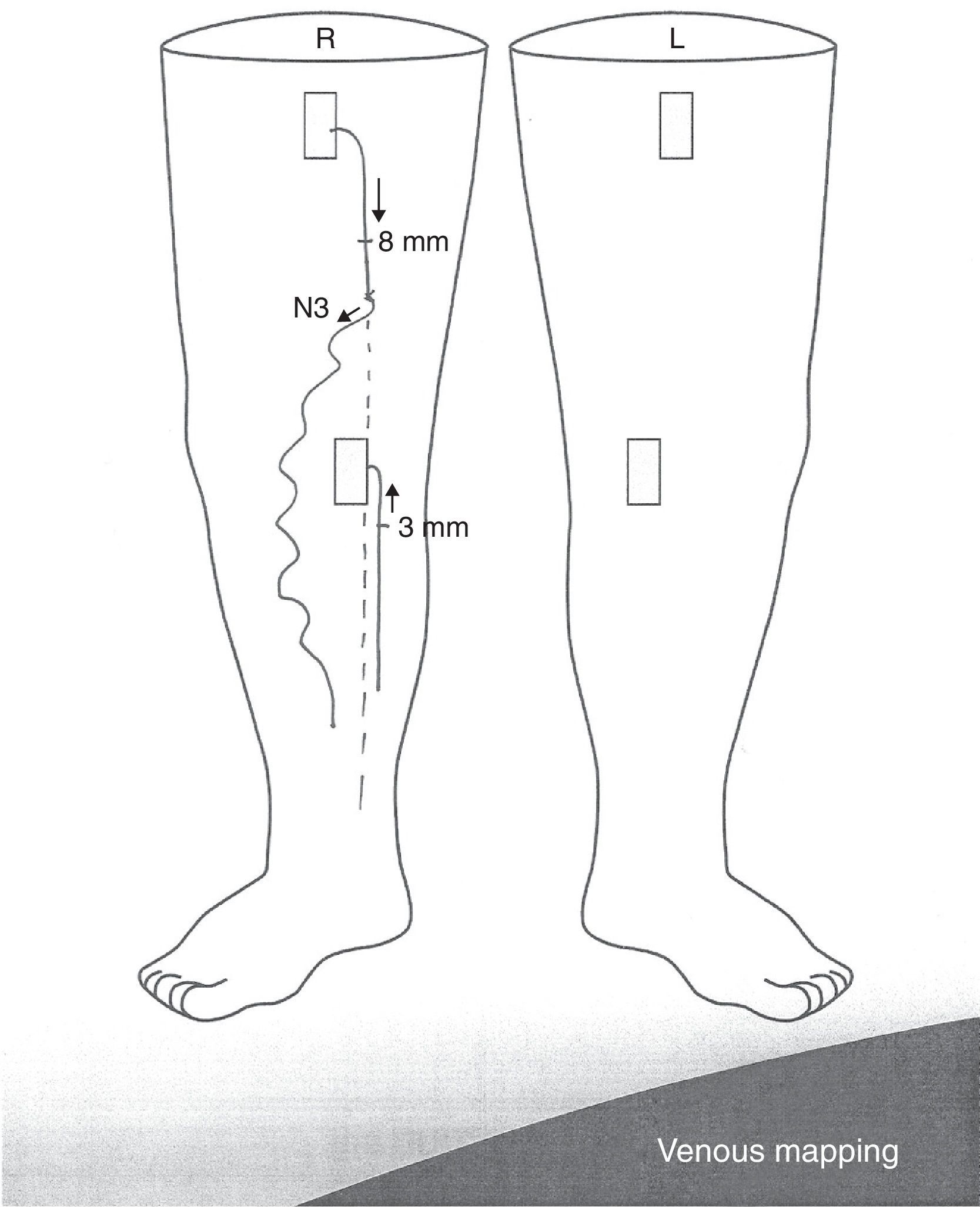
MappingLastly all these data must be recorded in a detailed manner and in an adequate nomenclature in the radiologic report and in one diagram,10 or mapping, which is the schematic description of the venous hemodynamics of the limb, which in turn allows us to rationalize treatment11 (Fig. 9).
The mapping needs to show the diameters of the saphenous veins, the leakage and re-entry points and the distribution of the varicose bundles marked with arrows in the direction of flow10 and identify the type of shunt.
Presurgical marking (Fig. 10)Right before the surgical intervention, the leakage and re-entry points and the palpable varicose segments (N3-N4) that need to be phlebotomized are marked on the skin in accordance with the guidelines established in the previous section.
Marking will be performed with the stand-up patient except in the case of varicose veins on the great saphenous vein; in this case the marking of the arch will be performed with the patient lying in the prone position given the anatomic variation in the origin thereof. We will not need to mark the arch of the small saphenous vein.
Marking is performed in indelible ink and on a shaved limb. It needs to be extremely accurate so that the surgeon can perform all the necessary incisions of the smallest possible size.
The patient shall not wash his body in the hours elapsing between the marking and the procedure.12
The mapping needs to be available for the surgeon during the initial study.
ConclusionDoppler ultrasound allows an adequate topographic and hemodynamic assessment of the SVS and the DVS in turn necessary for the diagnostic and therapeutic guidance of CVI and also allows us to establish differential diagnoses with other possible pathologic entities capable of causing similar symptoms.22
To perform the examination correctly, it is necessary to have an adequate knowledge of CVI anatomy and hemodynamic patterns.
Venous mapping is essential for surgical planning which must be individualized for every patient.12,20
The CHIVA strategy is a safe method allowing a quick and active recovery of the patients’ normal activity, including coming back to work with a low incidence of complications that are usually local and benign15,23 and an acceptable relapse rate.
Ethical responsibilitiesProtection of people and animalsThe authors declare that no experiments with human beings or animals have been performed while conducting this investigation.
Data confidentialityThe authors confirm that they have followed the protocols from their institutions on publishing data from patients.
Right to privacy and informed consentThe authors declare that in this article there are no data from patients.
Authors- 1.
Manager of the integrity of the study: MGC and PMV.
- 2.
Study Idea: CGH and MFRS.
- 3.
Study Design: CGH and MFRS.
- 4.
Data Mining: MGC and PMV.
- 5.
Data Analysis and Interpretation: MGC and PMV.
- 6.
Statistical Analysis: N/A.
- 7.
Reference Search: CGH, MFRS, MGC and PMV.
- 8.
Writing: CGH, MFRS, MGC and PMV.
- 9.
Critical review of the manuscript with intellectually relevant remarks: CGH, MFRS, MGC and PMV.
- 10.
Approval of final version: CGH, MFRS, MGC and PMV.
The authors declare no conflict of interests associated with this article whatsoever.
Please cite this article as: García Carriazo M, Gómez de las Heras C, Mármol Vázquez P, Ramos Solís MF. Estudio de la insuficiencia venosa crónica mediante ecografía Doppler y realización de cartografía venosa. Radiología. 2016;58:7–15.