Extramedullary plasmacytoma (EMP) is a plasma cell neoplasm of soft tissue without bone marrow involvement or other systemic characteristics of multiple myeloma. Approximately 80%–90% of EMPs involve the head and neck region, especially in the nasal cavity, paranasal sinuses, tonsillar fossa, and oral cavity. An EMP of the larynx is extremely rare and is a locally destructive lesion without systemic spread. Clinical features vary depending on the tumor location. A diagnosis is established by histopathology, immunohistochemistry, and a systemic survey to exclude systemic plasma cell proliferative diseases. Extramedullary plasmacytomas are highly radiosensitive and radiotherapy is therefore used as a treatment. In this study, we report on a rare case of EMP of the larynx evaluated with computed tomography and present histopathologic findings for a 74-year-old female patient.
El plasmocitoma extramedular (PEM) es una neoplasia de células plasmáticas del tejido blando sin afectación de la médula ósea ni otras características sistémicas de mieloma múltiple. Aproximadamente el 80%–90% de los PEM afectan a la región de la cabeza y el cuello, especialmente a la cavidad nasal, los senos paranasales, la fosa amigdalina y la cavidad oral. Los casos de PEM de laringe son extremadamente raros y se trata de una lesión destructiva a nivel local sin propagación sistémica. Las características clínicas varían en función de la localización del tumor. El diagnóstico se establece mediante histopatología, inmunohistoquímica y un estudio sistémico para excluir las enfermedades sistémicas de proliferación de células plasmáticas. Los plasmocitomas extramedulares son altamente sensibles a la radiación, por lo que se utiliza la radioterapia como tratamiento. En este estudio, notificamos un caso raro de PEM de laringe evaluado con tomografía computarizada y presentamos los resultados histopatológicos de una paciente de 74 años.
Extramedullary plasmacytoma (EMP) is a rare plasma cell neoplasm that occurs mainly in the soft tissues of the head and neck and accounts for 4% of all plasma cell tumors.1 Extramedullary plasmacytoma involvement can be seen in the nasal or nasopharyngeal area, larynx, oropharynx, tongue, tonsils, small salivary glands, posterior pharyngeal wall, thyroid gland, parathyroid gland, middle ear, colon and liver.2 Laryngeal involvement of the EMP is very rare and constitutes 0.2% of all malignancies in the larynx.3 The diagnosis of EMP is based on immunohistochemistry and the exclusion of systemic plasma cell proliferative diseases. Radiological imaging methods such as computed tomography (CT) and magnetic resonance imaging (MRI) are useful to evaluate the dissemination of the EMP to the spine, pelvis, femur and humerus.4,5 Since the EMP is radiosensitive, the standard treatment protocol is radiotherapy. Therefore, it is necessary to differentiate the EMP from the solitary plasmacytoma of bone and multiple myeloma in terms of treatment approach. In this study, we evaluated an EMP of the larynx in a 74-year-old female patient using histopathological and radiologic imaging findings.
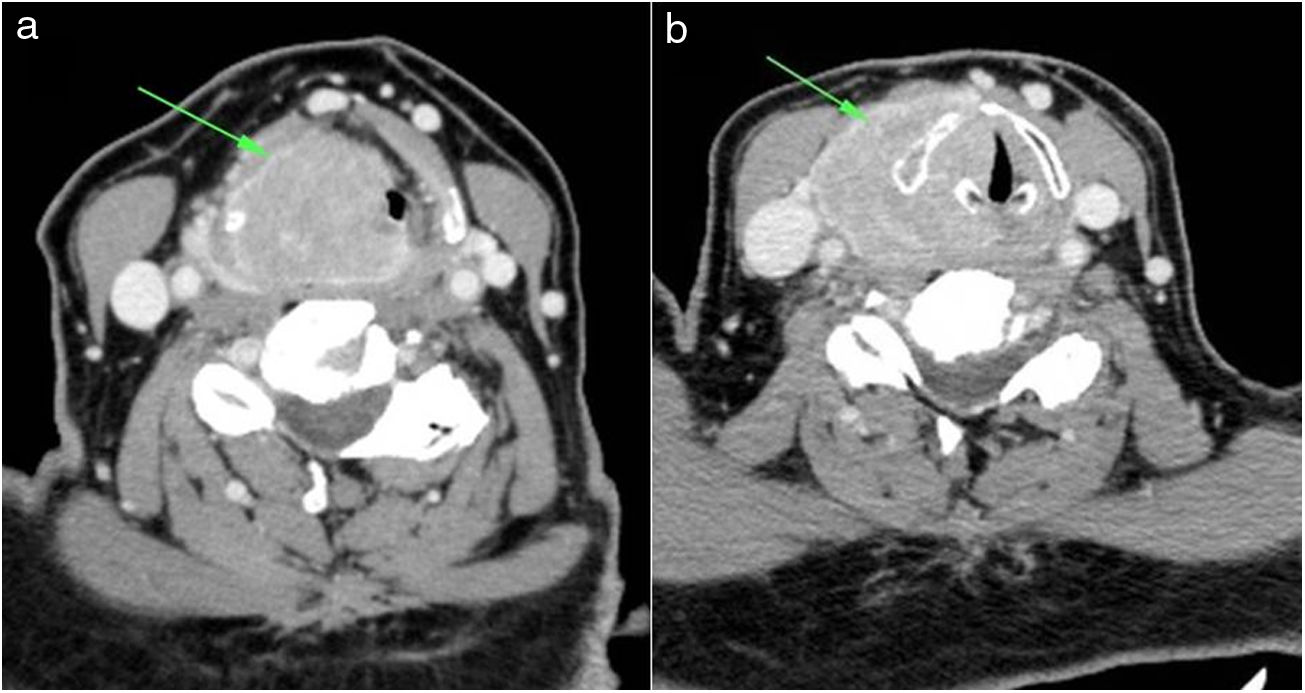
Case reportThe 74-year-old female patient was admitted to the Ear-Nose-Throat (ENT) specialist with complaints of hoarseness and difficulty swallowing that had persisted for approximately 1 year. Her past medical history and physical examination was unremarkable. The direct laryngoscopy revealed a mucosa-covered purple mass lesion arising from the pyriform sinus and lateral pharyngeal wall which nearly obstructed the lumen. Contrast-enhanced CT imaging of the neck revealed a 35×45mm lesion surrounding the right vocal cord and aryepiglottic fold, extending to the supraglottis and the extralaryngeal space with supraglottic airway narrowing (Fig. 1A,B). Size and appearance of the cervical lymph nodes were normal.
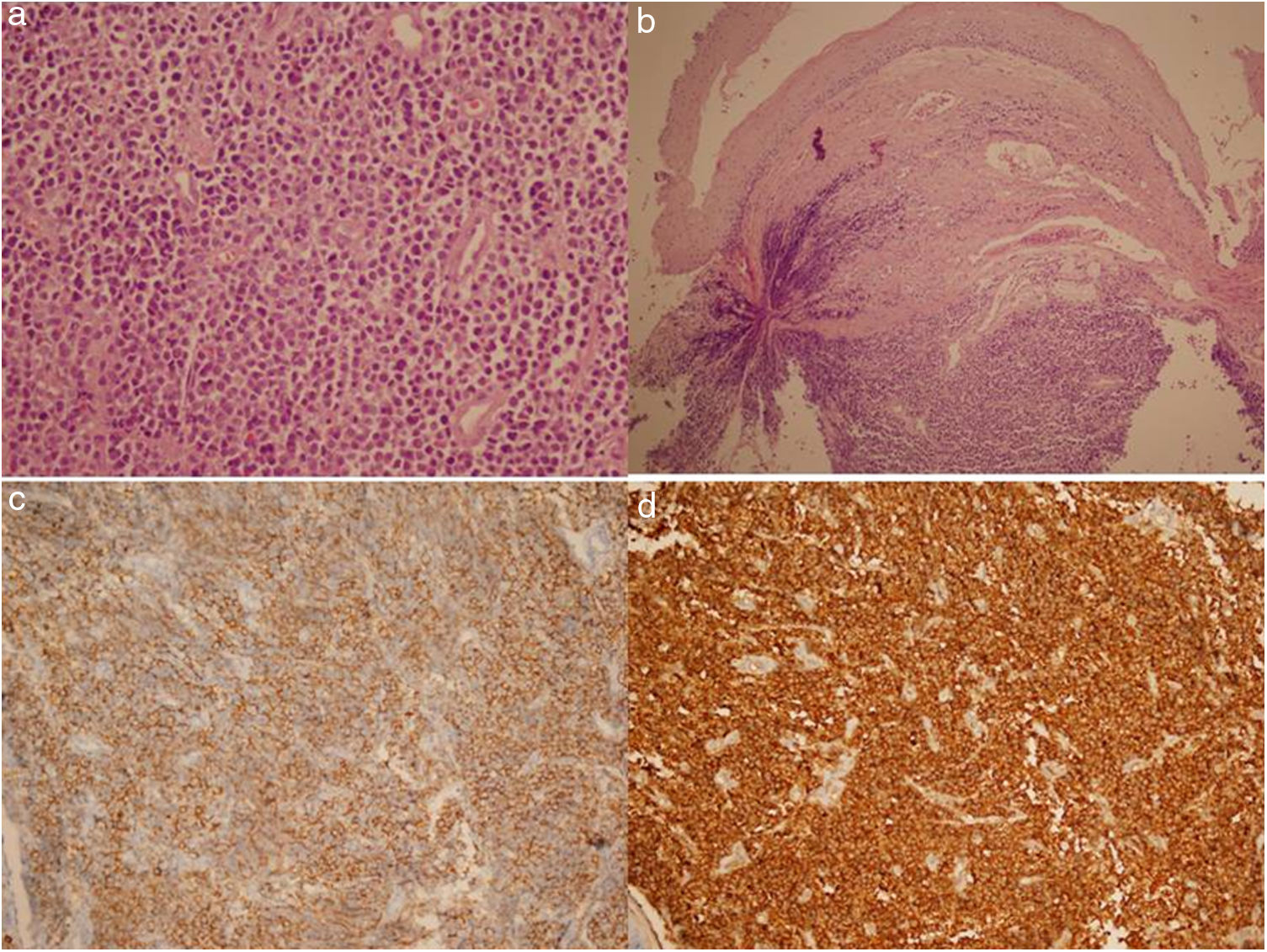
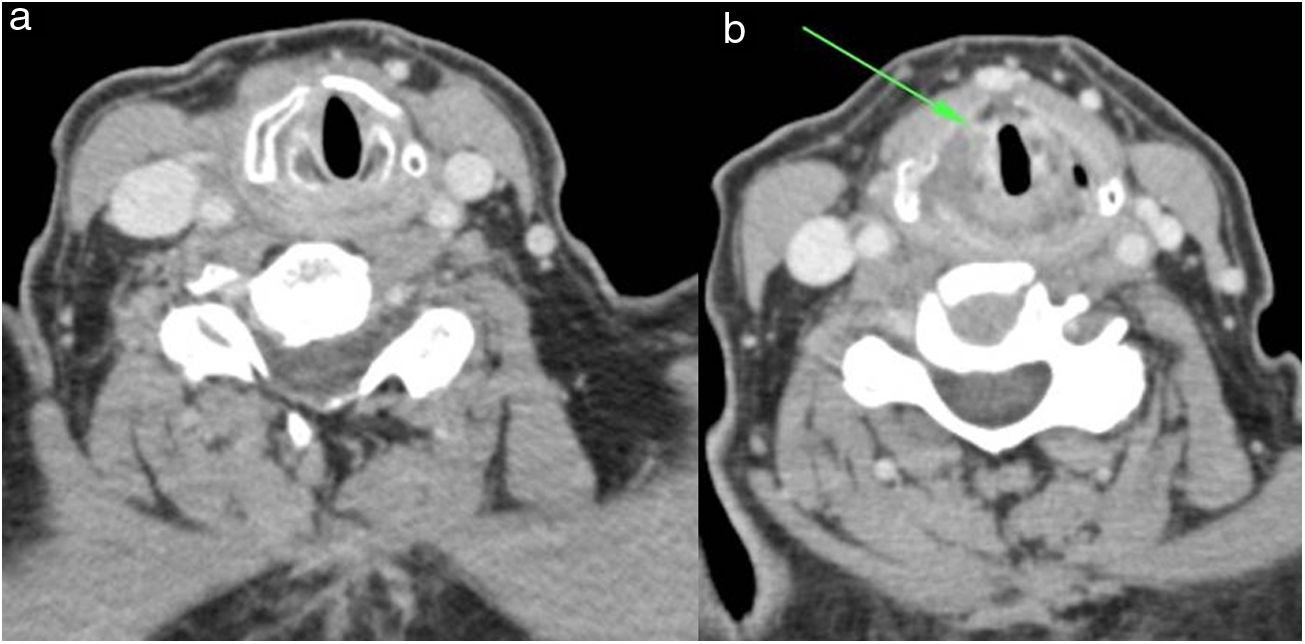
A direct laryngoscopy was performed under general anesthesia for the biopsy of the supraglottic mass. Histopathological examination revealed a uniform plasma cell proliferation with eccentrically situated nuclei under the epithelium (Fig. 2A,B) with CD138 (Bio SB, clone B-A38, USA) positive (Fig. 2C) immunohistochemistry characteristic of EPM. In addition, kappa (Thermo scientific, clone L1C1, USA) and lambda (Thermo scientific, cloneHP6054, USA) light chains (Fig. 2D) and IgG were found to be positive; CD56 (Genemed, clone 123C3, USA) and siklinD-1 (Ventana, SP4-R rabbit monoclonal, USA) were negative. The patient was further investigated for the presence of systemic disease. Hemoglobin concentration was 14g/dL, serum creatinine was 0.61mg/dL, and blood urea was 14.8mg/dL. Electrophoresis of serum and urine protein was normal. The skeletal survey did not reveal any lytic lesion. As a result of bone marrow biopsy, approximately 5%–10% plasma cells who were positive stained with CD138 and CD56 were detected. Cyclin D1 is negative. Thorax, abdominal and pelvic CTs were normal. In the absence of systemic involvement, the patient was diagnosed as having an EMP. The patient was treated with radiotherapy and chemotherapy. Three months after treatment was completed, tumor regression was confirmed by CT (Fig. 3A,B). There was no supraglottic mass and a 100% free supraglottic airway.
EMP of the larynx is an extremely rare plasma cell neoplasm.6 It accounts for 1% of all head and neck malignancies and 0.2% of all malignancies in the larynx.3 It is three times more common in males than in females.7 Common sites of involvement in the larynx (in order of frequency) are the epiglottis, ventricles, vocal cords, false cords, the aryepiglottic folds, arytenoids, and the subglottic region.5 Presenting symptoms are usually limited and nonspecific. Therefore, the diagnosis of an EMP of the larynx is often delayed. The most common symptom of EMP is slowly developing hoarseness. Late symptoms are dysphagia, dysphonia, dyspnea, chronic cough, stridor, and pain associated with locally aggressive tumors.1,6,8 Acute airway obstruction requiring intubation is very rare.
Radiological imaging methods are very useful in diagnosis. Also, lesion size, location, invasion of the adjacent tissue, and adjacent bone and cartilage destruction can be evaluated with imaging methods. Calcification and areas with low densities in the thyroid cartilage and infiltrative growth pattern are the typical findings of the EMP, which can seen with CT.10 Also, contrast-enhanced CT usually shows a well-circumscribed homogenous laryngeal mass, which appears with a mild-to-moderate contrast enhancement.1 MRI shows a laryngeal mass with hypointense on T1-weighted images (WIs) and hyperintense on T2 WIs. After injection of intravenous gadolinium, moderate-significant enhancement can be seen in the lesion.4 It is not possible to differentiate definitely EMP of the larynx from other benign and malignant laryngeal tumors by imaging methods. The diagnosis of solitary EMP is based on the exclusion of bone involvement and the demonstration of neoplastic plasma cells by immunohistochemical methods. In addition, in order to make a diagnosis of a solitary EMP there should be no disseminated disease. For this purpose, radiological imaging methods such as X-ray, CT and MRI can be used to evaluate the spine, pelvis, femur and humerus.4,5 Bone marrow biopsy should also be within the normal range. In addition, there should be no signs of serum urine monoclonal protein, anemia, hypercalcemia, or renal impairment.5
Surgery, radiotherapy, chemotherapy, and combinations of these can be used in treatment. Radiotherapy is the standard treatment for EMP as it is highly radiosensitive.3 Extramedullary plasmacytomas can be controlled locally at a rate of 80%–100% with radical radiotherapy.8 One of the advantages of radiotherapy for an EMP is excellent protection of the sound. However, acute radiation toxicity as a result of prolonged radiotherapy over several weeks is a disadvantage of the radiotherapy treatment.9 Surgery can be performed in lesions with failed radiotherapy. In addition, surgery is preferred to prevent long-term sequelae of radiotherapy. With regard to multiple myeloma progression, a chemotherapy approach is still controversial for prevention and treatment of recurrent disease. Chemotherapy can also be used for inoperable patients and disseminated disease.9
The prognosis of EMP observed in the head and neck is better than that for solitary plasmacytoma of the bone and multiple myeloma. In those cases of bone and multiple myeloma, 70% of the patients typically undergo10 years of surveillance.4 However, 10%–30% of cases progress to multiple myeloma within two years. The prognosis of these cases is poor. Multiple factors play a role in progression of multiple myeloma. The size of the tumor at diagnosis, total serum protein level, and a monoclonal spike observed on serum protein electrophoresis are predictive factors of progression to multiple myeloma.5 Therefore, patients should be followed for an extended period of time following treatment. Follow-ups should be performed systemically as well as local control.3 Clinicians should be alert to multiple myeloma findings such as anemia, bone pain, and renal failure.8
ConclusionAlthough EMP of the larynx is rarely seen in cases of head and neck tumors, it should be kept in mind in the differential diagnosis of laryngeal tumors. There are no characteristic radiological imaging findings. Radiotherapy is a common and effective treatment modality for EMP because of its radiosensitivity. Although the prognosis for patients with EMP is good, multiple myeloma may progress in the long term. Therefore, long-term systemic follow-up is required following treatment.
Authorship1. Responsible for study integrity: ATS and ME.
2. Study conception: ATS.
3. Study design: ATS and ME.
4. Data acquisition: ATS and SG.
5. Data analysis and interpretation: ATS and SG.
6. Statistical processing: ATS.
7. Literature search: ATS and SG.
8. Drafting of the manuscript: ATS, ME and SG.
9. Critical review of the manuscript with intellectually significant contributions: ATS, ME and SG.
10. Approval of the final version: ATS, ME and SG.
Conflicts of interestThe authors declare that they have no conflict of interest.
Please cite this article as: Tanrivermis Sayit A, Elmali M, Gün S. Evaluación del plasmocitoma extramedular de laringe con hallazgos radiológicos e histopatológicos. Radiología. 2022;64:69–73.