To review the prognostic usefulness of chest X-rays in selecting patients with suspected SARS-CoV-2 infection.
Material and methodsThis cross-sectional descriptive observational study analyzed 978 patients with suspected SARS-CoV-2 infections who underwent chest X-ray examinations in the emergency department of a tertiary hospital in March 2020. We separately analyzed demographic, clinical, and prognostic variables in two groups of patients: those in whom reverse-transcriptase polymerase chain reaction (RT-PCR) was done (n = 535) and those in whom RT-PCR was not done because of low clinical suspicion (n = 443).
ResultsIn the group of patients with RT-PCR, the prevalence of SARS-CoV-2 was 70.4%, and the sensitivity of chest X-rays was 62.8%. In the group of patients without RT-PCR, chest X-rays were negative in 97.5%, corroborating the low clinical suspicion; these patients were discharged, and 5.6% of them reconsulted with mild forms of the disease. In the group of patients with RT-PCR, we observed no statistically significant differences in the percentage of pathologic chest X-rays between patients hospitalized in the ICU (72.9%) and in those hospitalized in other wards (68.3%) (p = 0.22).
ConclusionIn the context of the pandemic, patients with low clinical suspicion and negative chest X-rays can be discharged with a low probability of reconsultation or of developing severe COVID19. In patients with RT-PCR positive for SARS-CoV-2, chest X-rays have no prognostic usefulness.
Revisar la utilidad pronóstica de la radiografía de tórax en la selección de pacientes con sospecha de infección por SARS-CoV-2.
Material y métodosEstudio observacional, descriptivo y transversal, realizado en 978 pacientes con sospecha de infección por SARS-CoV-2 a los que se les hizo una radiografía de tórax en el servicio de urgencias de un hospital terciario, en marzo de 2020. Se analizaron variables demográficas, clínicas y pronósticas por separado en pacientes con RT-PCR (reacción en cadena de la polimerasa por transcriptasa inversa) hecha (grupo 1, n = 535) o no hecha por baja sospecha clínica (grupo 2, n = 443).
ResultadosEn el grupo 1 se observó una prevalencia de SARS-CoV-2 del 70,4%. La radiografía mostró una sensibilidad del 62,8%. En el grupo 2, la radiografía fue negativa en el 97,5%, corroborando la baja sospecha clínica, y fueron dados de alta; de ellos, el 5,6% volvió a consultar con formas leves de la enfermedad. En el grupo 1 no se observaron diferencias estadísticamente significativas en el porcentaje de radiografías de tórax patológicas entre los pacientes ingresados en plantas hospitalarias (68,3%) y los ingresados en la unidad de cuidados intensivos (72,9%), (p = 0,22).
ConclusiónEn situación de pandemia, los pacientes con baja sospecha clínica y radiografía negativa pueden ser dados de alta con baja probabilidad de volver a consultar o de desarrollar formas graves de la enfermedad. En los pacientes con SARS-CoV-2 positivo, la radiografía de tórax inicial no tiene utilidad pronóstica.
In December 2019, an outbreak of a new pathogen, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2 virus), was detected in Wuhan (Hubei province, China).1 It quickly spread worldwide, and on 11 March 2020, the WHO declared a pandemic situation.2 The main route of transmission is between people through droplets and/or aerosols. It is also transmitted through contact with mucosal surfaces (eyes, nose and mouth).3
Worldwide, as of October 2021, SARS-CoV-2 infection had caused 246.8 million cases, with five million deaths.4
The reference technique for the diagnosis of SARS-CoV-2 infection is reverse transcriptase-polymerase chain reaction (RT-PCR). It has high sensitivity, but this can vary depending on the symptoms. It takes an average of eight hours to obtain results.5
There are studies which discuss the limited utility of screening with chest X-rays to detect SARS-CoV-2 pneumonia in asymptomatic patients or those with mild symptoms6, and in a consensus document, the Fleischner Society does not recommend it.7
Computed tomography (CT) shows greater sensitivity than chest X-ray, but is not recommended for screening or diagnosis by the American College of Radiology (ACR) or the European Society of Radiology (ESR).8,9
Our aim was to analyse the usefulness of chest X-ray in the accident and emergency department (A&E) to distinguish patients with SARS-CoV-2 pneumonia who needed to be admitted and have the nucleic acid amplification test from those with low clinical and radiological suspicion of infection who could be discharged, at a time of the pandemic when there was a shortage of RT-PCR tests.
Material and methodsObservational, descriptive, cross-sectional study, which included 978 consecutive patients with symptoms suggestive of SARS-CoV-2 infection who had a chest X-ray from 10 to 23 March 2020, during the first weeks of the pandemic.
The established hospital protocol for patients with suspected SARS-CoV-2 infection consisted of performing an initial chest X-ray to classify patients with radiological findings compatible with COVID-19 pneumonia (positive) or not compatible (negative). The chest X-rays were reported by thoracic and non-thoracic radiologists from A&E.
The group with positive radiological findings was given the RT-PCR test, and in the group with negative X-rays, RT-PCR was considered according to the degree of clinical suspicion, at the discretion of the attending doctor.
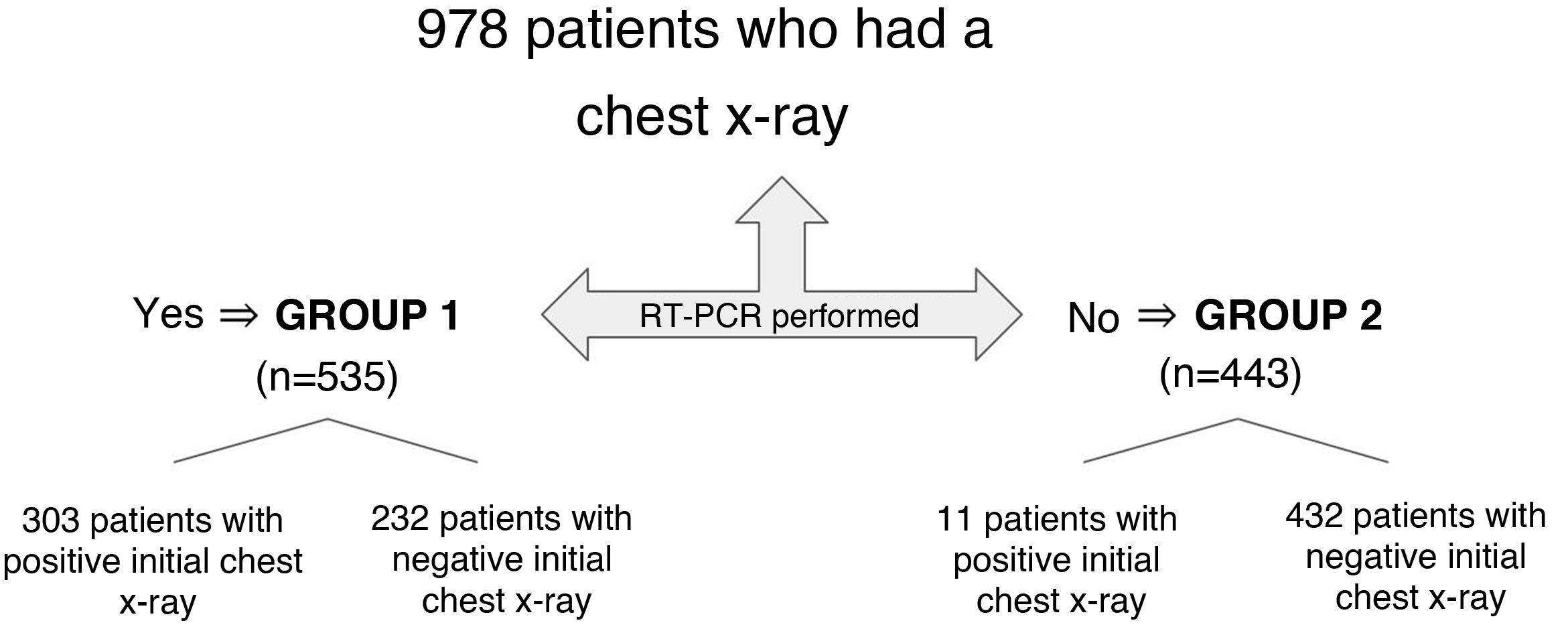
The dependent variable was established as the performance of the RT-PCR test, and it was compared with the rest of the independent variables, classifying the patients into two groups: group 1, of patients with RT-PCR performed (n = 535) and group 2, of patients with low clinical suspicion who were not given the test (n = 443) (Fig. 1).
Posterior-anterior view chest X-rays which were well-centred and showed well inflated lungs were included in the study. Chest X-rays reported as low quality and performed on portable equipment were excluded.
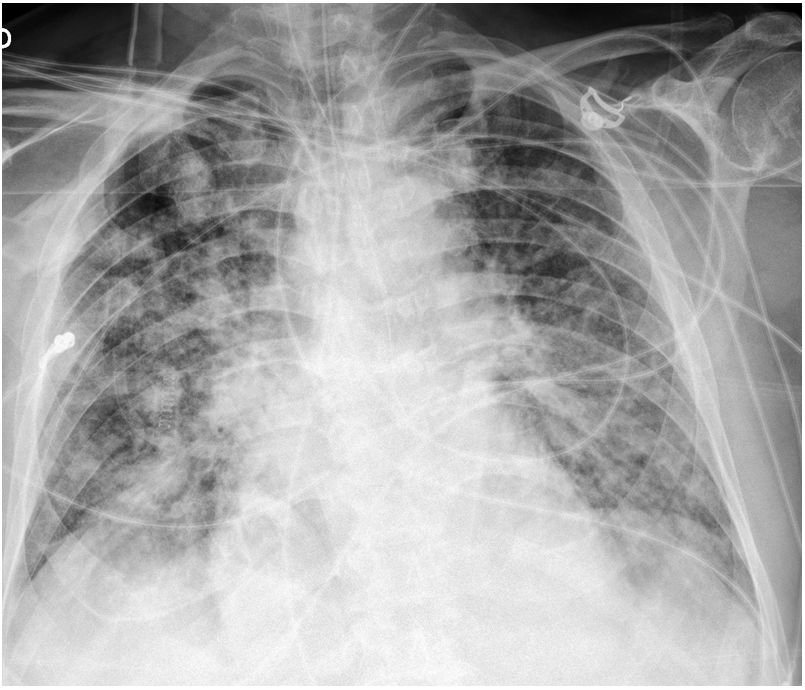
Positive chest X-rays were those with findings consistent with COVID-19 pneumonia, i.e. bilateral pulmonary consolidations or opacities of mainly peripheral and basal location (Fig. 2). X-rays were considered negative if they showed lobar consolidations or pleural effusion or were normal.6 We carried out a prospective follow-up of the patients with a negative initial X-ray, and noted chest X-rays that showed abnormalities (following the same inclusion criteria as the initial ones), either during their hospital stay or because they returned to A&E.
Demographic (age, gender) and prognostic variables [need for admission, admission to the intensive care unit (ICU), intubation and mortality] were included in the study.
The χ2 statistical test was used for the analysis of qualitative variables, considering p < 0.05 as statistically significant. It was carried out with SPSS for Windows, v24.0 software (IBM Corporation, Armonk, NY, USA).
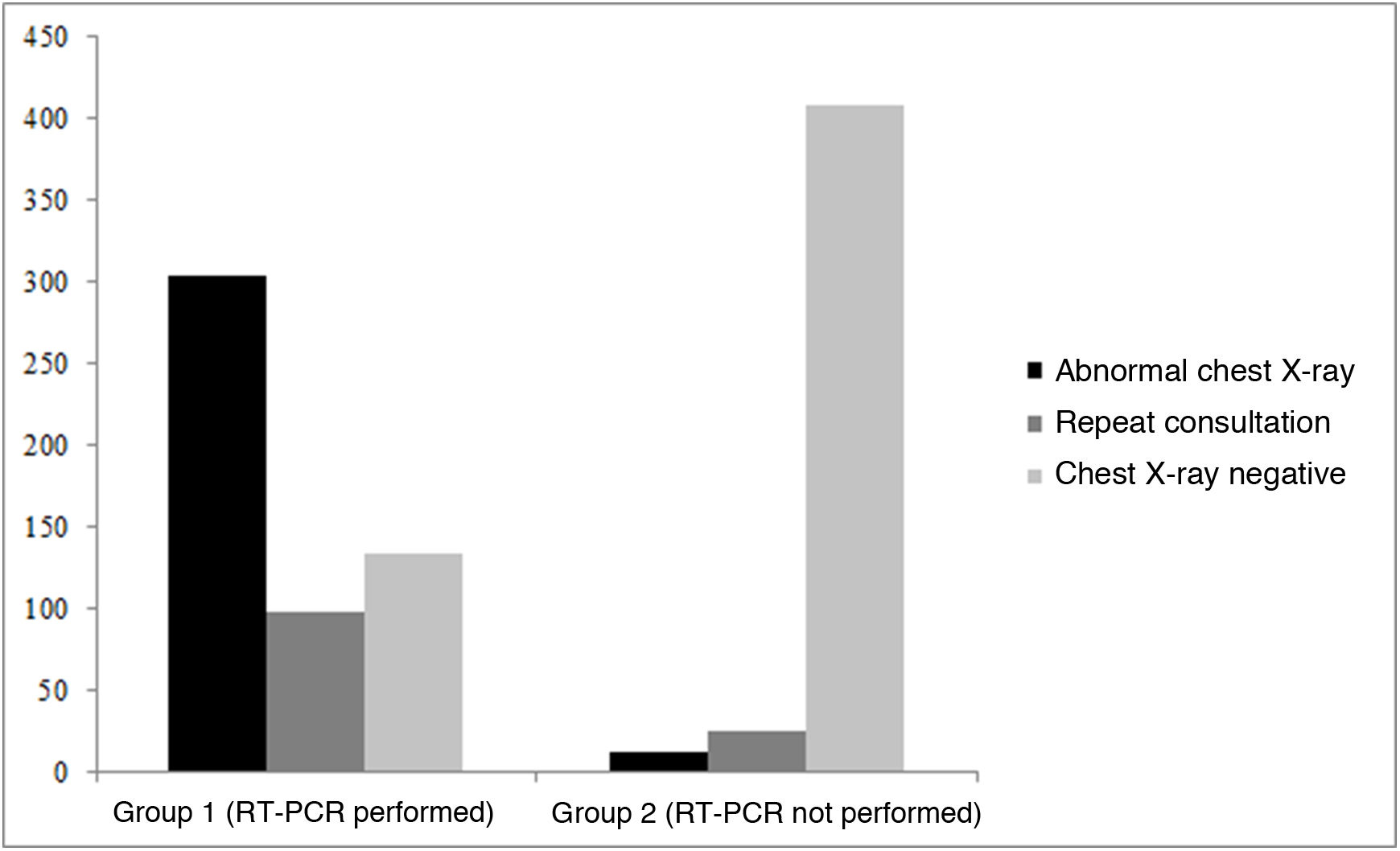
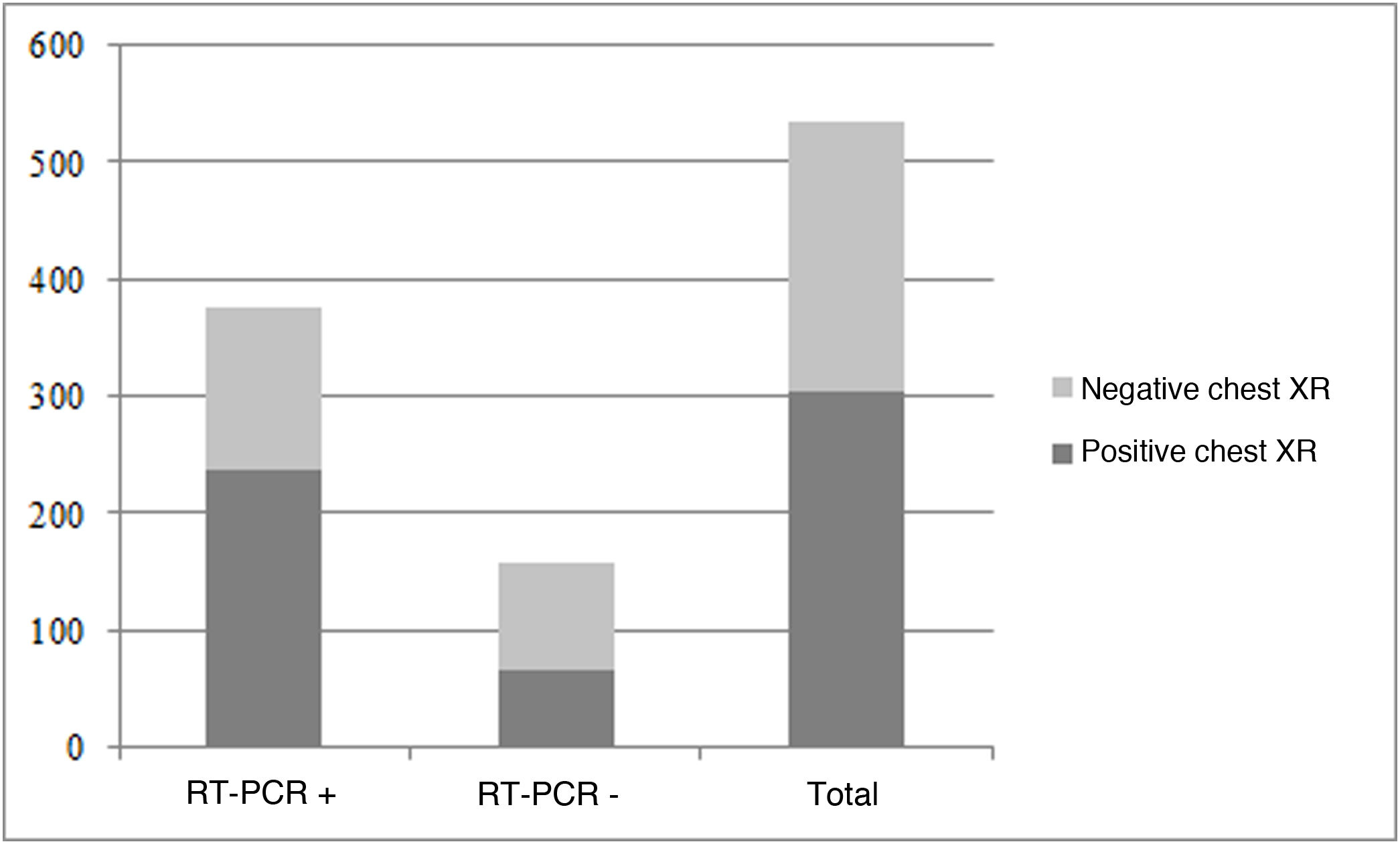
ResultsAfter excluding patients whose X-rays did not meet the above requirements, 978 patients who attended A&E with suspected SARS-CoV-2 infection were included in the study (52.1 ± 19.1 years, 50.2% male). They were divided into a first group of 535 patients who had the RT-PCR technique due to strong clinical suspicion and a second group of 443 patients who did not have RT-PCR due to a low degree of clinical suspicion (Table 1, Fig. 3).
Description of the variables for groups 1 and 2.
| Group 1 (RT-PCR performed) | Group 2 (RT-PCR not performed) | p | |
|---|---|---|---|
| Patients | 535 | 443 | |
| Age | 58.44 ± 18.24 years | 44.54 ± 17.2 years | <0.05 |
| Gender | 253 female, 282 male | 234 female, 209 male | >0.05 |
| Initial X-ray positive | 303 | 11 | <0.05 |
| Later X-ray positive | 98 | 24 | <0.05 |
| Admission, ICU and intubation | 310 admitted to ward, 50 ICU, 36 intubation | 4 admitted to ward | <0.05 |
| Death | 41 | 1 | <0.05 |
RT-PCR: reverse transcription-polymerase chain reaction; ICU: intensive care unit.
In group 1, the prevalence of SARS-CoV-2 infection was 70.4% (377/535). The prevalence was higher among those who had a positive chest X-ray (78.2%, 237/303) than among those with a negative chest X-ray (60.3%, 140/232), obtaining a χ2 of p < 0.05.
Within the group of patients with positive RT-PCR for SARS-CoV-2 (377 patients), 237 developed COVID-19 pneumonia detected on the initial chest X-ray. Of the 140 patients with a negative initial chest X-ray, 53 (38%) patients showed abnormalities on subsequent chest X-rays performed during their stay in hospital or when the patient returned to A&E (Fig. 4).
A sensitivity of 62.8%, a specificity of 58.2%, a positive predictive value (PPV) of 78.2% and a negative predictive value (NPV) of 39.7% were obtained for the initial chest X-ray in the diagnosis of SARS-CoV-2 infection (Table 2). If we include the patients with chest X-ray abnormalities during the course of the infection (including hospital stay and when they returned to A&E), the sensitivity rises to 76.9%, with a PPV of 81.5% and a NPV of 51.4%; the specificity does not vary (Table 3).
Contingency table in group 1 patients (n = 535) taking into account the initial radiological findings.
| RT-PCR + | RT-PCR − | Total | |
|---|---|---|---|
| Abnormal chest X-ray | 237 | 66 | 303 |
| Chest X-ray negative | 140 | 92 | 232 |
| Total | 377 | 158 | 535 |
+: positive result for SARS-CoV-2 in the RT-PCR test; −: negative result for SARS-CoV-2 in the RT-PCR test; RT-PCR: reverse-transcription-polymerase chain reaction.
Contingency table in group 1 (n = 535) taking into account the radiological findings during the patient's disease course (including admission and when they returned to the accident and emergency department).
| RT-PCR + | RT-PCR − | Total | |
|---|---|---|---|
| Abnormal chest X-ray | 290 | 66 | 356 |
| Chest X-ray negative | 87 | 92 | 179 |
| Total | 377 | 158 | 535 |
+: positive result for SARS-CoV-2 in the RT-PCR test; −: negative result for SARS-CoV-2 in the RT-PCR test; RT-PCR: reverse-transcription-polymerase chain reaction.
In group 2, the chest X-ray was negative in 97.5% (432/443) of patients, corroborating the low degree of clinical suspicion, for which they were discharged; 5.6% (24/432) returned to A&E due to persistence or worsening of symptoms, but without needing hospital admission.
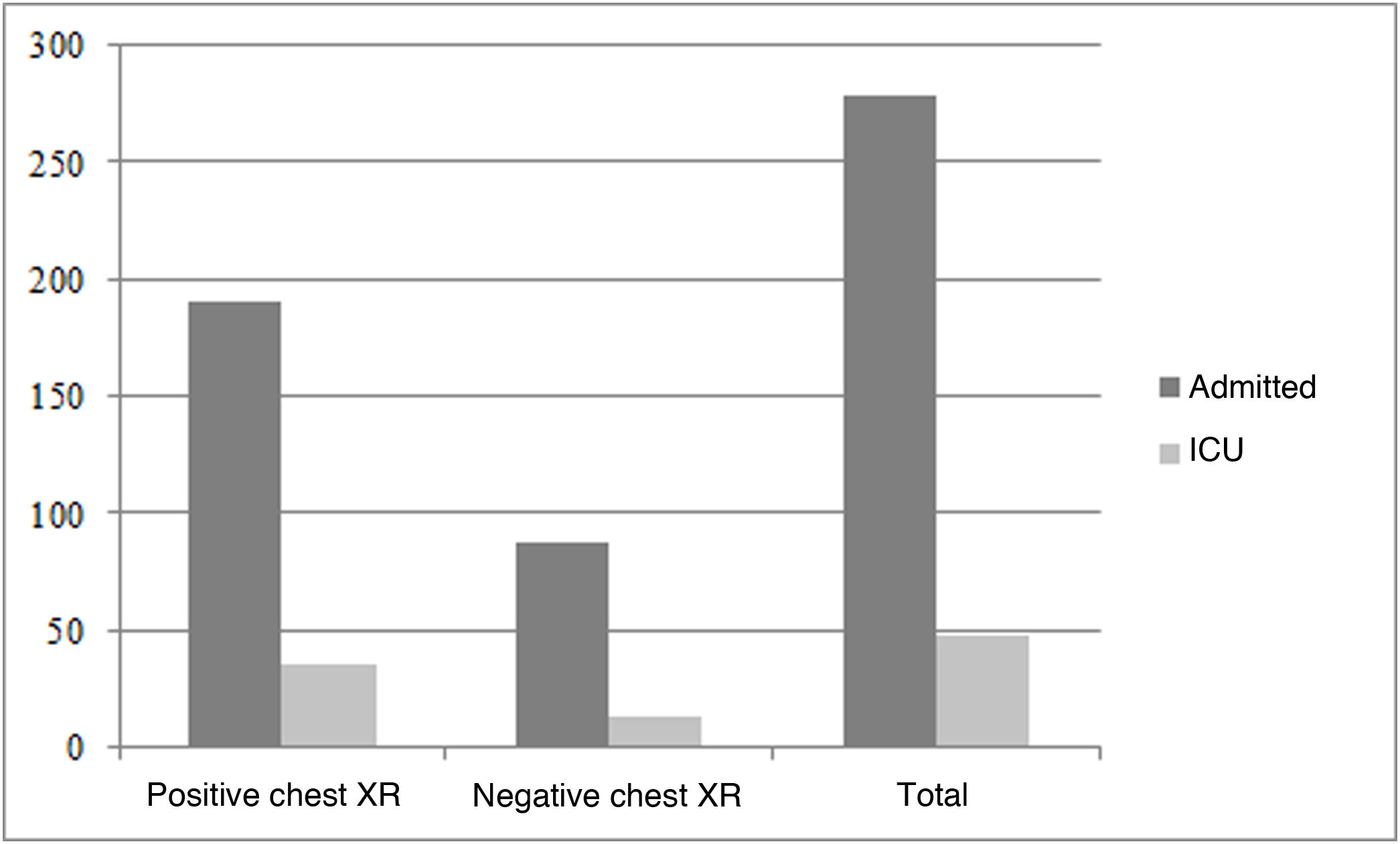
The 326 patients admitted to hospital with positive RT-PCR for SARS-CoV-2 were divided into two groups according to whether they needed admission to a hospital ward (278 patients) or to ICU (48 patients). No statistically significant differences were detected between the two groups according to abnormalities in the initial chest X-ray (68.3% and 72.9% respectively) (Table 4, Fig. 5).
Comparison between patients not admitted, admitted to ward and admitted to ICU.
| Not admitted | Admitted to ward | ICU | p | |||
|---|---|---|---|---|---|---|
| RT-PCR | Not performed | Negative | Positive | Positive | Positive | – |
| Patients | 439 | 158 | 51 | 278 | 48 | – |
| Abnormal chest X-ray | 11 (2.5%) | 53 (33.5%) | 12 (23.5%) | 190 (68.3%) | 35 (72.9%) | 0.22 |
RT-PCR: reverse-transcription-polymerase chain reaction ICU: intensive care unit.
Thirty-five of the 377 patients with positive RT-PCR (9.3%) died. The percentage of patients with positive chest X-ray was similar in the group of patients who died (65.7%, 23/35) to those who did not (62.4%, 214/343), with no statistically significant differences detected (χ2p > 0.6).
With regard to demographic variables, no statistically significant differences were found between the gender of the patients and performing the RT-PCR test (p = 0.095). Differences were found, however, between the age of the patients and performing the test (p < 0.05), as it was more likely in older people.
Men had higher admission and mortality rates (p < 0.05), but no gender differences were found when analysing admission to ICU.
Older patients had higher admission, admission to ICU and mortality rates (p < 0.05), with all the patients who died being over the age of 60.
DiscussionIn the early days of the pandemic, due to a lack of RT-PCR tests and the arrival of many patients at A&E, it was necessary to develop triage circuits to separate patients who required hospital admission from those who could be discharged.
Among patients for whom there was strong clinical suspicion and RT-PCR was performed (group 1 in our study), in 56.6% of cases the X-ray showed abnormalities. According to Fleischner Society recommendations, a chest X-ray is a good technique for detecting lung involvement or suggesting alternative diagnoses.7 A meta-analysis showed that chest X-ray correctly diagnosed COVID-19 pneumonia in 80.6% of patients and erroneously in 28.5%. No statistically significant differences were found between chest X-ray and CT (computed tomography).10
Other authors also followed the same protocol as ours during the pandemic, when the availability of the RT-PCR test for SARS-CoV-2 was limited. They performed a chest X-ray as the first imaging test,11 and if this was indeterminate or intermediate risk, continuing with a CT to further characterise the distribution of involvement12. The sensitivity and specificity of chest X-ray interpreted by expert radiologists is 89% and 66% respectively. Sensitivity drops to 66% when the radiologists are less experienced.13
A chest X-ray also enables us to select the most serious patients while waiting for the RT-PCR result, as this can take hours.7,10
An initial negative chest X-ray or CT does not exclude the diagnosis of SARS-CoV-2 infection, as an infected patient can have a normal imaging test in the early stages of the disease and become positive later.11,14,15
Among patients for whom there was low clinical suspicion and RT-PCR was not performed, in 97.5% of cases the X-ray showed no abnormalities. In a study conducted in young Singaporean patients with a positive RT-PCR test for SARS-CoV-2, but with mild symptoms, the vast majority had no chest X-ray abnormalities or clinical worsening.16 The Fleischner Society does not recommend chest radiography in patients with mild symptoms of SARS-CoV-2 infection or asymptomatic patients without risk of worsening7, although in our case it was a criterion for discharging patients with low risk of complications.
Some studies have shown a sensitivity, specificity, PPV and NPV similar to ours when analysing the chest X-rays of patients who have attended A&E with symptoms compatible with SARS-CoV-2 infection.17,18
Chest X-rays reported by thoracic and non-thoracic radiologists were considered in our evaluation, and differences in sensitivity and specificity were not assessed. Tsakok et al. 19 showed no statistically significant differences in sensitivity and specificity between reports made by thoracic and non-thoracic radiologists.
In our study, we found differences in the disease prognosis between males and females and between age groups. These findings were similar to those in other studies, which also showed that severe infection and death were more common among adult males.20,21
Our study had limitations because the RT-PCR test was not performed on all patients, only those for whom there was strong clinical suspicion, so we did not study patients who were asymptomatic or had few symptoms and no chest X-ray abnormalities. There is now better access to and availability of the RT-PCR test for the diagnosis of SARS-CoV-2 infection, so the diagnosis is made with this technique using chest X-ray for detection of pneumonia. We did not consider either the extension or the pattern of the chest X-ray abnormalities, analysing only whether they had abnormalities or not. In addition, we did not apply a quantification scale to the radiological findings when assessing the chest X-rays, as other authors have done.22,23
ConclusionsDuring the initial phase of the SARS-CoV-2 pandemic when RT-PCR diagnostic testing was limited, chest x-ray proved to be a useful tool in screening patients requiring hospital admission, regardless of performing RT-PCR. We found in our study that patients with no abnormalities on the initial chest x-ray had a good prognosis and rarely returned to the accident and emergency department.
In the patients admitted, however, the initial chest x-ray had no prognostic value.
Authorship- 1.
Responsible for study integrity: ESG, AP, JMEF and JAS.
- 2.
Study concept: ESG, AP, JMEF and JAS.
- 3.
Study design: ESG, AP, JMEF and JAS.
- 4.
Data collection: ESG and AP.
- 5.
Data analysis and interpretation: ESG, AP and JMEF.
- 6.
Statistical processing: ESG, AP and JME.
- 7.
Literature search: ESG, AP and JAS.
- 8.
Writing of the manuscript: ESG, AP, JMEF and JAS.
- 9.
Critical review of the manuscript with intellectually significant contributions: ESG, AP, JMEF and JAS.
- 10.
Approval of the final version: ESG, AP, JMEF and JAS.
The authors declare that they have no conflicts of interest.
Please cite this article as: Saez de Gordoa E, Portella A, Escudero-Fernández JM, Andreu Soriano J. Utilidad de la radiografía de tórax para la detección de neumonía COVID 19 durante la pandemia por SARS-CoV-2. Radiología. 2022;64:310–316.