A little over 30 years have passed since the first report on the use of coronary balloon angioplasty or, as it is currently called, primary percutaneous coronary intervention (PCI), for the treatment of patients with acute myocardial infarction, which is now called acute coronary syndrome with ST-segment elevation.1
This therapy started in parallel and had the same objectives of pharmacological coronary reperfusion (performed through intracoronary and, subsequently, intravenous administration of fibrinolytics): rapid and complete recovery of the anterograde coronary flow in the occluded epicardial coronary artery; reduction of the underlying coronary stenosis promoting the acute event; and coronary microcirculation preservation.2 These principles are the weapons used to overcome muscular necrosis and its malevolent and severe consequences, which quickly appear after acute coronary vessel occlusion.3
The first controlled and randomized trials comparing both methods, primary PCI vs. fibrinolytics, were published in 1993. Since then, a wave of positive, effective, restorative reperfusion of the coronary flow lost in acute occlusion has been definitively established, being largely favorable to the use of primary PCI.4
The advent of the so-called “modern antiplatelet therapy”, which started with intravenous administration of glycoprotein IIb/IIIa inhibitors and progressed to the synthesis and use of the oral inhibitors of P2Y12 platelet receptors, has provided the much-needed systemic safety to the interventional procedure, a catalyst of strong coagulation vectors, and, as a final pillar of primary PCI consolidation, the mechanical anchoring of the ruptured atherothrombotic plaque, through coronary stent implantation.3
Within a 20-year period, the interventionist method, feared and discredited at an initial moment, has become a unanimity in contemporary cardiology practice, reigning over the world's medical guidelines as the method of choice to treat ST-elevation myocardial infarction, with Class I and Level of Evidence A recommendation – the highest possible.5–7
Thus, a strong pressure has been placed on hospital medical services on a worldwide scale. Hemodynamic and cardiovascular intervention services, previously accustomed to closing their activities after business hours, were turned upside down in their logistics, being forced to operate in the so-called eternal cycle, open 24hours during the 7 days of the week, without ever closing.5–7
Primary PCI has brought results that can be considered unique in the history of modern cardiology. The impact of reduced mortality, together with these patients’ rapid rehabilitation to work and social life, demonstrated the best feature of this procedure: the unequivocal ability to save lives, removing even the most resistant critics from their conservative trenches (for every 100 patients undergoing primary PCI vs. fibrinolysis, 5 deaths, 5 reinfarctions, and 1 stroke are prevented).8
However, how can this benefit be offered to the entire population, in broadest sense? From the rural dweller, away from the tertiary centers, to the urban patient, trapped in chaotic traffic jams, and in all the different healthcare management systems?
As demonstrated by Araújo et al.,9 primary PCI requires hospitals with a tertiary structure, equipped with dedicated radiology equipment, structured coronary units, an ample and always available array of percutaneous devices (the coronary anatomy will only be known in an emergency and will be always different from one patient to another), promptly available cardiac surgery and – most importantly – the dedicated “HR factor” (Human Resources), with qualified interventionists, trained in the approach of this acute and risky scenario, and a trained and experienced multidisciplinary team, in addition to treatment and access protocols that have been validated, implemented, and proven to be effective, available 24/7!3,5–7 Phew! A bridge too far?
Araujo et al.,9 located in the extreme south of Brazil, have shown that it is indeed possible and have demonstrated their results in their consecutive cohort. It is interesting to observe the incidence of cases in one of the largest federal hospitals in the Southern region of Brazil - approximately 80 per year; six, on average, per month; a little more than one per week.
Given the number of infarctions reported to the Brazilian Unified Health System (SUS, acronym in Portuguese), approximately 50,000 cases/year, these numbers can be considered low, showing that the bridge remains too far; that is, it is not possible to treat as many patients as we should, since, for the most part, the distance and the multiple difficulties in the diagnosis of myocardial infarction result in a delay that removes the patients from the window of the best therapeutic opportunity: treatment at most within the initial 12hours, and in an ideal world, in the first 6hours of symptom onset. From the number of primary PCIs reported to SUS, it can be estimated that 12% of infarctions treated under the public healthcare system undergo primary PCI.10,11
The therapeutic strategy of primary PCI requires understanding of the severity and intensity of myocardial infarction symptoms, as well as the search for professional help as soon as possible. In this sense, SUS users are far from having this awareness, partly because of those who should educate them.12,13
Additionally, it should be mentioned that the availability of hospitals with established PCI programs is far from ideal because of the number of inhabitants, and that effective and organized transfer programs for this type of reperfusion are still a dream in our country.10–13
In turn, data from primary PCIs are available in the SUS electronic database, starting in 2004; in the last 10 years, the increment in the number of procedures was remarkable, exceeding 300%.11
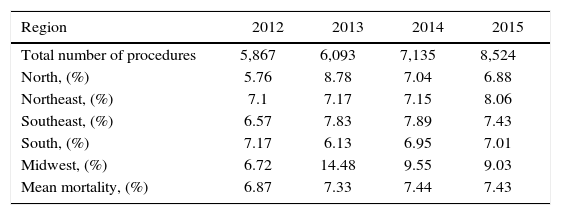
Comparing the findings of Araujo et al. with SUS numbers is an interesting task that illustrates the effort of colleagues to build a reperfusion bridge for these acutely infarcted individuals (Table 1).9–11
Primary percutaneous coronary intervention. In-hospital mortality rate and number of procedures performed under the Brazilian Unified Health System.
| Region | 2012 | 2013 | 2014 | 2015 |
|---|---|---|---|---|
| Total number of procedures | 5,867 | 6,093 | 7,135 | 8,524 |
| North, (%) | 5.76 | 8.78 | 7.04 | 6.88 |
| Northeast, (%) | 7.1 | 7.17 | 7.15 | 8.06 |
| Southeast, (%) | 6.57 | 7.83 | 7.89 | 7.43 |
| South, (%) | 7.17 | 6.13 | 6.95 | 7.01 |
| Midwest, (%) | 6.72 | 14.48 | 9.55 | 9.03 |
| Mean mortality, (%) | 6.87 | 7.33 | 7.44 | 7.43 |
The mean mortality observed in the study by Araújo et al. was 9.9%, or approximately one-quarter higher than the Southern regional average in the year 2015. The authors discuss this finding, focusing on the delay in transferring these infarcted patients, considered higher than the ideal (transfer time of 4.4 ± 2.5hours and door-to-balloon time of 68 ± 34minutes) – the latter being very good, below the desired 90minutes.
In addition to the delay in transfer, the patient's delay in seeking care is a contributing factor to the increase in the time of ischemia, which determines worsening of results and prognosis.3
In the study by Araujo et al., Killip IV was observed in 11.6% of cases on admission, and cardiovascular events at 30 days were observed in 18.3%. These results, among other factors, may be justified by the delay in opening the artery.14
The patients were referred from other health units 74% of the and in 29.3% they were transferred by the Emergency Medical Services (SAMU, acronym in Portuguese), that is, a bridge needs to be built for patients to arrive quickly, considering that a specialized structure to receive them will be waiting.
The increase in the delay will result in a reduction of the benefits and may lead to increased procedural difficulty in reestablishing normal anterograde coronary flow, but the advent of adjuvant techniques and potent anticoagulant and antiplatelet pharmacology may help to increase PCI performance in scenarios of greater thrombotic adversity.3
Other justifications and suggestions can be listed: delayed start of antiplatelet therapy (in the primary center, not only upon arriving at the tertiary center) and analysis of the interventionist profile, since it is a university hospital (physicians in training vs. physicians with established experience).
Is the bridge still too far? Yes, it will always be; while we do not reach a higher percentage of infarcted individuals being submitted to primary PCI, we will need strong, unwavering and committed healthcare management performance.
In a country of bold inequalities, with abysmal socioeconomic gradients of continental extension, with heterogeneous public management, thrice divided in its powers, often claudicating, oscillating, and subject to political-partisan rather than technical influences, only the persistence of a united, interested, and apt group of physicians can achieve significant advances, thus building not an unstable platform, but a perennial bridge, lined with solid concrete, to pave the reperfusion for the many more that will need it.
Or else, all we shall have left to say, as one high official told British field marshal Montgomery, which inspired a great film, filled with Hollywood stars: “I think we may be going a bridge too far...”
Conflicts of interestThe authors declare no conflicts of interest.