Door-to-balloon time (DBT) has become a measure of performance and is the focus in quality of care improvement initiatives. This study aimed to evaluate the association between DBT and its impact on hospital costs.
MethodsPatients treated with primary percutaneous coronary intervention between 2008 and 2013 were divided according to the DBT < or ≥ 90minutes. All costs recorded at hospital discharge were adjusted by the Medical-Hospital Cost Variation Index.
ResultsA total of 141 patients were included, grouped as DBT < 90minutes (n = 77) and DBT ≥ 90minutes (n = 64). DBT was 64.0 ± 14.1minutes and 133.8 ± 35.2minutes, respectively. There were no differences in clinical outcomes between the groups. The costs were R$ 34,883.24 ± 27,749.46, with the mean cost for DBT < 90minutes being R$ 33,194.24 ± 27,387.61 and the cost for DBT ≥ 90minutes R$ 36,947.58 ± 28,267.80 (p = 0.43). The costs, according to the culprit artery, were R$ 29,588.53 ± 16,358.85 for the right coronary artery; R$ 48,494.62 ± 44,015.04 for the left circumflex artery; and R$ 34,016.96 ± 26,503.94 for the left anterior descending artery. There was a difference between the costs of procedures related to the left circumflex artery when compared to the right coronary or left anterior descending arteries (p = 0.01), but there was no difference between the costs related to the right coronary, when compared to the left anterior descending artery (p = 0.68).
ConclusionsThere was no difference in hospital costs regarding the private health insurance, when the groups were divided according to the DBT. Clinical outcomes were similar and a difference in costs was found for patients with the circumflex artery as the culprit vessel.
O tempo porta-balão (TPB) tornou-se uma medida de desempenho e é foco de iniciativas de melhoria da qualidade assistencial. Este estudo teve como objetivo avaliar a relação entre o TPB e seu impacto nos custos de internação hospitalar.
MétodosPacientes tratados com intervenção coronária percutânea primária, entre 2008 e 2013, foram divididos de acordo com o TPB < ou ≥ 90 minutos. Todos os custos registrados na alta hospitalar foram ajustados por meio do Índice de Variação de Custos Médico-Hospitalares.
ResultadosForam incluídos 141 pacientes, agrupados em TPB < 90 minutos (n = 77) e TPB ≥ 90 minutos (n = 64). Os TPB foram 64,0 ± 14,1 minutos e 133,8 ± 35,2 minutos, respectivamente. Não foram observadas diferenças nos desfechos clínicos entre os grupos. Os custos foram de R$ 34.883,24 ± 27.749,46, sendo o custo médio para TPB < 90 minutos de R$ 33.194,24 ± 27.387,61, e para TPB ≥ 90 minutos, de R$ 36.947,58 ± 28.267,80 (p = 0,43). Os custos, segundo a artéria culpada, foram de R$ 29.588,53 ± 16.358,85 para a coronária direita; R$ 48.494,62 ± 44.015,04 para a circunflexa; e de R$ 34.016,96 ± 26.503,94 para a descendente anterior. Houve diferença entre os custos dos procedimentos relativos à artéria circunflexa comparados aos da coronária direita ou da descendente anterior (p = 0,01), mas não houve diferença entre os custos relativos à coronária direita, comparados à descendente anterior (p = 0,68).
ConclusõesNão houve diferença nos custos hospitalares, no âmbito da saúde suplementar, quando os grupos foram divididos de acordo com o TPB. Os desfechos clínicos foram semelhantes, e foi encontrada uma diferença de custos em pacientes com a artéria circunflexa culpada.
Door-to-balloon time (DBT) is one of the markers of quality of care and, according to the current guidelines, it should be less than 90minutes.1–3 Several clinical and logistic factors may be related to a high DBT.4–6 A decrease in DBT results in a reduction of short- and medium-term mortality, as well as lenght of hospital stay.7,8
In recent years, health care costs have increased faster than the general inflation rate, thus becoming a liability to be paid by both the institution that provides the service and the agents that finance the procedures. Cost control without loss of quality is, thus, an urgent topic.9
Despite the positive effect of reducing DBT on patient outcomes, the impact on care-related costs in Brazil is still scarcely studied. As it represents a disease with high prevalence and of great influence in economic terms, as well as having significant morbidity and mortality,10 it becomes essential to understand the costs associated with the management of patients with ST-elevation acute myocardial infarction (STEMI).
This study aimed to evaluate the association between DBT and its impact on hospital costs.
MethodsStudy place, design, and institutional measuresIn 2007, Hospital Vera Cruz, a tertiary hospital that integrates the supplementary health network in Belo Horizonte (MG), initiated a project on the quality of care provided to patients with acute myocardial infarction through the measurement of several indicators, among them the DBT.
With the implementation of these indicators, measures were taken to improve the DBT, such as expedite the admission of patients in the emergency room; perform the 12-lead electrocardiogram (ECG) within 10minutes after admission; and engaging the whole team, consisting of nurses and physicians (clinical and interventional cardiologists) through a standardized code. With the implementation of these measures, there was a progressive reduction in DBT.
As determined by the quality program, epidemiological data and time related to treatment were collected and stored in an institution database.
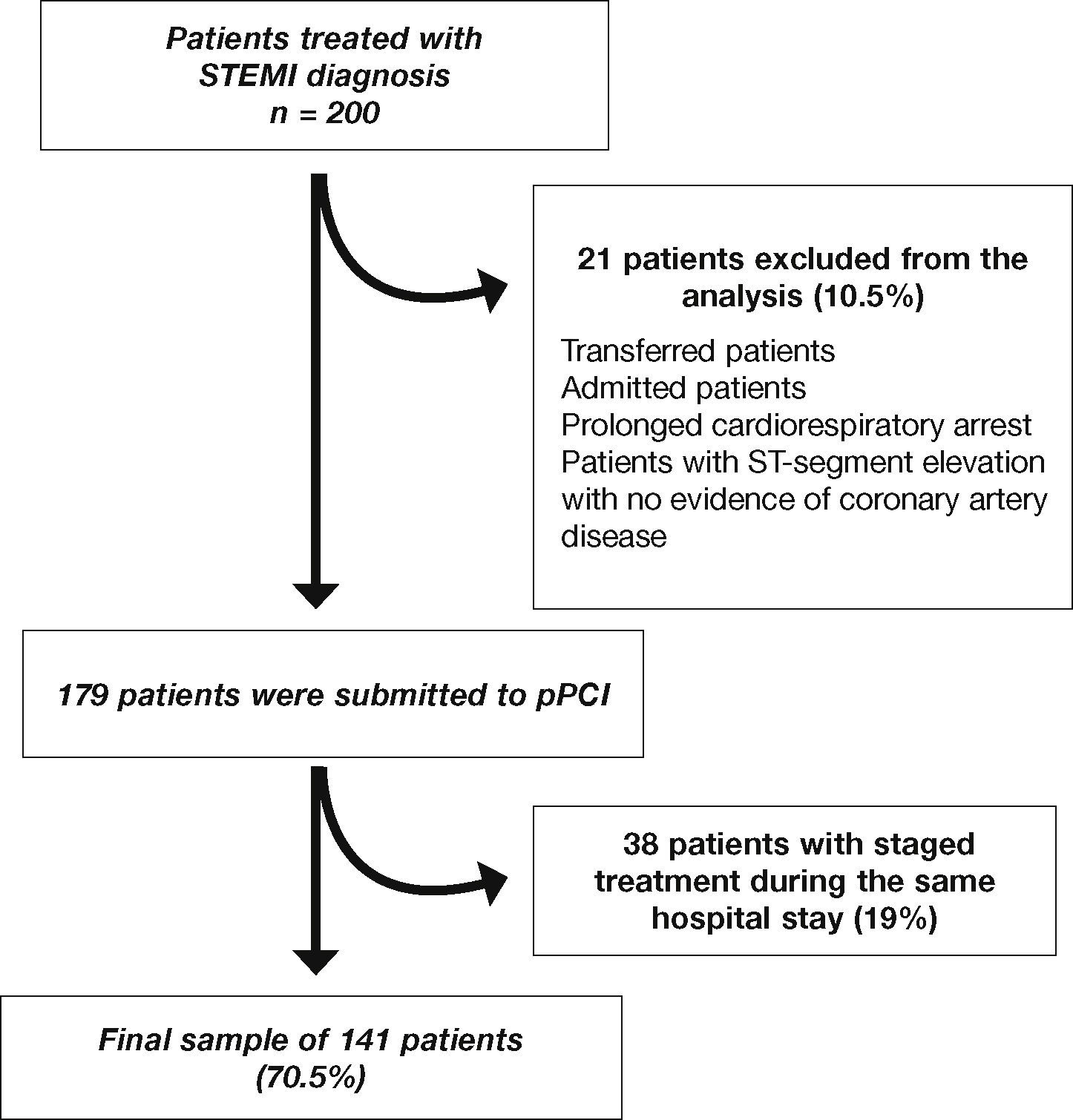
Study populationBetween March 2008 and June 2013, 200 patients underwent primary percutaneous coronary intervention (pPCI). Patients transferred from other institutions; those who developed STEMI after admission; those on prolonged cardiorespiratory arrest in the emergency room; those with segment ST-elevation without evidence of coronary artery disease (e.g., acute myocarditis, ventricular repolarization disorder, or Takotsubo syndrome); and those submitted to staged treatment during the same hospital admission were excluded from the analysis.
The care was carried out following the on-duty schedule of the interventional cardiology laboratory, which has in-attendance and on-call medical and nursing staff 24hours a day, 7 days a week.
The patients included in the study were divided into two groups according to DBT < or ≥ 90-minutes.
ProcedurePatients received a loading dose of 300mg of acetylsalicylic acid and 300 to 600mg of clopidogrel. The use of morphine, sublingual/intravenous nitrate, or beta-blocker was made at the discretion of the physician. All patients received unfractionated heparin immediately before the intervention (60 to 100 U/kg). Patients were taken to undergo the intervention as soon as the cath lab was available. The pPCI procedures were performed as described in literature.11 Specific technical aspects, such as access route, drug administration, type of stent, and thromboaspiration, were carried out at the discretion of the interventionists. After pPCI, patients were referred to the coronary care unit and received treatment according to the institutional protocol established for STEMI.
Data collectionData collection was performed in two ways. First, delays and epidemiological data were collected dating to the patient's admission at the institution; second, the data related to costs were collected through the review of medical records and of the invoices sent by the institution to the health insurance companies. This registry was approved by the Research Ethics Committee of the hospital (CAE 46658215.5.0000.5135).
Angiographic analysis and definitionsLesion morphology was classified according to the definitions established by the American College of Cardiology/American Heart Association (ACC/AHA).12 Angiographic analysis was performed by two of the authors (RW and MABE), identifying the culprit artery and considering as a significant lesion that which would cause vessel lumen obstruction > 70% by the visual method interpretation. Thrombus on the angiography was defined as abrupt cessation of vessel flow, with contrast retention or a filling defect in a patent vessel (negative image) over a stenotic or adjacent region.13
Procedure success was defined as obtaining angiographic success (residual stenosis < 30% with Thrombolysis In Myocardial Infarction - TIMI grade 3 flow), as well as absence of major adverse cardiovascular and cerebrovascular events, including death, reinfarction and emergency coronary artery bypass graft surgery.
The DBT was defined as the delay between the first medical contact and the first balloon inflation; total ischemic time was defined as the delay between symptom onset and the first balloon inflation.
Lenght of hospital stay was recorded in days since the admission day (day zero). The analysis of the length of stay considered only the patients who were discharged home, excluding those who died during the hospitalization period.
Cost analysisHospital costs were described in Brazilian currency (Real). As they were recorded at the time of hospital discharge, all costs included in the analysis were adjusted by the Índice de Variação de Custos Médico-Hospitalares (VCMH/IESS).14 The costs referred to values charged by the institution from the supplementary health insurance companies, which included costs related to health care, procedures, medications, orthotics, and prosthetics, as well as to the daily cost of the intensive care unit.
All patients remain hospitalized at the discretion of the attending cardiologist, according to daily clinical practice.
Statistical analysisThe collected data were stored in an Excel spreadsheet (Microsoft Corporation, Redmond, USA) and data analysis was carried out with the Statistical Package for the Social Sciences (SPSS) software, version 9.0 (Chicago, USA). The qualitative variables are shown as absolute number and frequency, and were analyzed by Chi-square or Fisher's exact test. Quantitative variables are shown as mean and standard deviation and were analyzed using Student's t-test. All results were considered significant at p ≤ 0.05.
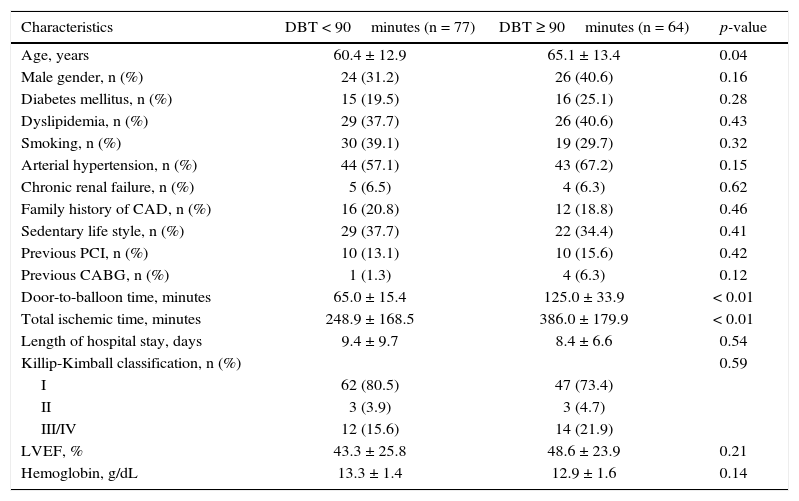
ResultsPatients selected for final analysis (Fig. 1) were grouped into DBT < 90minutes (n = 77) and DBT ≥ 90minutes (n = 64). The mean DBT was 64.0 ± 14.1minutes and 133.8 ± 35.2minutes, respectively. No significant differences were observed regarding the clinical variables (Table 1).
Clinical characteristics.
| Characteristics | DBT < 90minutes (n = 77) | DBT ≥ 90minutes (n = 64) | p-value |
|---|---|---|---|
| Age, years | 60.4 ± 12.9 | 65.1 ± 13.4 | 0.04 |
| Male gender, n (%) | 24 (31.2) | 26 (40.6) | 0.16 |
| Diabetes mellitus, n (%) | 15 (19.5) | 16 (25.1) | 0.28 |
| Dyslipidemia, n (%) | 29 (37.7) | 26 (40.6) | 0.43 |
| Smoking, n (%) | 30 (39.1) | 19 (29.7) | 0.32 |
| Arterial hypertension, n (%) | 44 (57.1) | 43 (67.2) | 0.15 |
| Chronic renal failure, n (%) | 5 (6.5) | 4 (6.3) | 0.62 |
| Family history of CAD, n (%) | 16 (20.8) | 12 (18.8) | 0.46 |
| Sedentary life style, n (%) | 29 (37.7) | 22 (34.4) | 0.41 |
| Previous PCI, n (%) | 10 (13.1) | 10 (15.6) | 0.42 |
| Previous CABG, n (%) | 1 (1.3) | 4 (6.3) | 0.12 |
| Door-to-balloon time, minutes | 65.0 ± 15.4 | 125.0 ± 33.9 | < 0.01 |
| Total ischemic time, minutes | 248.9 ± 168.5 | 386.0 ± 179.9 | < 0.01 |
| Length of hospital stay, days | 9.4 ± 9.7 | 8.4 ± 6.6 | 0.54 |
| Killip-Kimball classification, n (%) | 0.59 | ||
| I | 62 (80.5) | 47 (73.4) | |
| II | 3 (3.9) | 3 (4.7) | |
| III/IV | 12 (15.6) | 14 (21.9) | |
| LVEF, % | 43.3 ± 25.8 | 48.6 ± 23.9 | 0.21 |
| Hemoglobin, g/dL | 13.3 ± 1.4 | 12.9 ± 1.6 | 0.14 |
DBT: door-to-balloon time; CAD: coronary artery disease; PCI: percutaneous coronary intervention; CABG: coronary artery bypass grafting; LVEF: left ventricular ejection fraction.
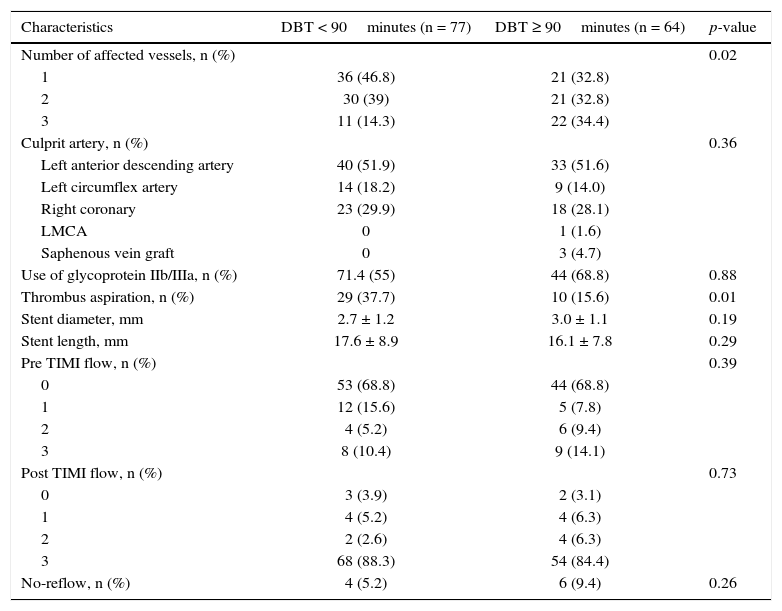
pPCI was carried out through the femoral access in 139 cases (98.5%), while the radial access was used in the remaining patients. The culprit artery in 50% of the cases was the left anterior descending (LAD) artery. A glycoprotein IIb/IIIa inhibitor was administered to 54.5% of patients in the group DBT < 90minutes and to 56.4% of the patients in the group DBT ≥ 90minutes (p = 0.88). A total of 151 coronary stents were implanted, all bare-metal stents, with a mean of 1.1 ± 0.6 stents per patient.
No-reflow occurred in 4% of the patients in the group DBT < 90minutes and in 7.7% of the group DBT ≥ 90minutes (p = 0.33) (Table 2).
Angiographic and procedure characteristics.
| Characteristics | DBT < 90minutes (n = 77) | DBT ≥ 90minutes (n = 64) | p-value |
|---|---|---|---|
| Number of affected vessels, n (%) | 0.02 | ||
| 1 | 36 (46.8) | 21 (32.8) | |
| 2 | 30 (39) | 21 (32.8) | |
| 3 | 11 (14.3) | 22 (34.4) | |
| Culprit artery, n (%) | 0.36 | ||
| Left anterior descending artery | 40 (51.9) | 33 (51.6) | |
| Left circumflex artery | 14 (18.2) | 9 (14.0) | |
| Right coronary | 23 (29.9) | 18 (28.1) | |
| LMCA | 0 | 1 (1.6) | |
| Saphenous vein graft | 0 | 3 (4.7) | |
| Use of glycoprotein IIb/IIIa, n (%) | 71.4 (55) | 44 (68.8) | 0.88 |
| Thrombus aspiration, n (%) | 29 (37.7) | 10 (15.6) | 0.01 |
| Stent diameter, mm | 2.7 ± 1.2 | 3.0 ± 1.1 | 0.19 |
| Stent length, mm | 17.6 ± 8.9 | 16.1 ± 7.8 | 0.29 |
| Pre TIMI flow, n (%) | 0.39 | ||
| 0 | 53 (68.8) | 44 (68.8) | |
| 1 | 12 (15.6) | 5 (7.8) | |
| 2 | 4 (5.2) | 6 (9.4) | |
| 3 | 8 (10.4) | 9 (14.1) | |
| Post TIMI flow, n (%) | 0.73 | ||
| 0 | 3 (3.9) | 2 (3.1) | |
| 1 | 4 (5.2) | 4 (6.3) | |
| 2 | 2 (2.6) | 4 (6.3) | |
| 3 | 68 (88.3) | 54 (84.4) | |
| No-reflow, n (%) | 4 (5.2) | 6 (9.4) | 0.26 |
DBT: door-to-balloon time; LMCA, left main coronary artery; TIMI: Thrombolysis in Myocardial Infarction.
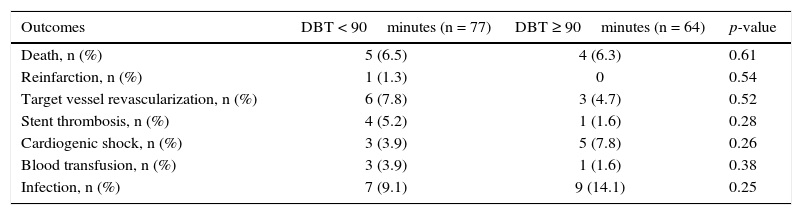
There was no significant difference in the mean length of stay or the clinical outcomes between the groups (Table 3).
In-hospital clinical evolution.
| Outcomes | DBT < 90minutes (n = 77) | DBT ≥ 90minutes (n = 64) | p-value |
|---|---|---|---|
| Death, n (%) | 5 (6.5) | 4 (6.3) | 0.61 |
| Reinfarction, n (%) | 1 (1.3) | 0 | 0.54 |
| Target vessel revascularization, n (%) | 6 (7.8) | 3 (4.7) | 0.52 |
| Stent thrombosis, n (%) | 4 (5.2) | 1 (1.6) | 0.28 |
| Cardiogenic shock, n (%) | 3 (3.9) | 5 (7.8) | 0.26 |
| Blood transfusion, n (%) | 3 (3.9) | 1 (1.6) | 0.38 |
| Infection, n (%) | 7 (9.1) | 9 (14.1) | 0.25 |
DBT: door-to-balloon time.
The overall mean costs of the procedures was R$ 34,883.24 ± 27,749.46, with the mean cost for DBT < 90minutes of R$ 33,194.24 ± 27,387.61 and for DBT ≥ 90minutes of R$ 36,947.58 ± 28,267.80 (p = 0.43). The mean cost according to the affected artery was R$ 29,588.53 ± 16,358.85 for the right coronary artery (RCA), R$ 48,494.62 ± 44,015.04 for the left circumflex artery (LCx) and R$ 34,016.96 ± 26,503.94 for the LAD. There was a significant difference between the costs of the procedures related to the LCx when compared to the RCA (p = 0.01) or the LAD (p = 0.01), but there was no significant difference between the costs of the procedures for the RCA when compared to the LAD (p = 0.68).
DiscussionThis study showed no difference regarding hospital costs in a private hospital when the analyzed groups were divided regarding the DBT. The groups were similar considering clinical outcomes, with a difference found regarding costs in patients with a culprit artery in the LCx territory.
Hospital costs verified in this analysis are consistent with those reported by national and international literature.15–18 The increase in health care costs is currently approximately two times higher than the annual economic growth of developed countries.19,20 In Brazil, the VCMH/IESS has also been higher than the National Broad Consumer Price Index (IPCA) since 2007. Since 2012, while the VCMH/IESS rose 15.4%, inflation in the same period was 5.4% as measured by the IPCA.15
In a systematic review, we found only one study that evaluated the costs of implementing a quality program specifically designed to improve the care of patients with STEMI, which showed a reduction in costs with improved DBT.21 In the present study, there was a reduction, but without statistical significance.
In the sub-analysis of the HORIZONS-AMI study, Prasad et al. showed that while the DBT is one of the predictors of microvascular injury (evaluated by the resolution of ST-segment elevation and myocardial blush at angiography), the total ischemic time (time of symptom onset until reperfusion) is more important. After 2hours of total ischemia, patients with DBT < 90minutes had a microvascular perfusion resolution rate similar to those with time ≥ 90minutes. As the present patients had a mean total time of ischemia > 2hours, this could possibly explain the negative result of the study, in terms of reduction of clinical outcomes in the group DBT < 90minutes.22
In the present series, patients with DBT > 90minutes, although older, with multivessel disease, and longer ischemic time, showed no difference in lenght of hospital stay. In accordance with Pepe et al., in the sample under analysis, the higher cost was related to the invasive treatment (68%), with a lower impact from daily hospital fees (10%) and drugs (25%).23
LCx treatment showed a higher cost than LAD and RCA treatments, a finding that may be random, as the total number of patients in the sample was small. However, the LCx is an artery whose diagnostic difficulty is higher,24,25 and moreover, it has a higher incidence of post-infarction mechanical complications (mitral regurgitation),26,27 which could also explain this finding.
This work aimed to call attention to the implications of costs when treating patients with acute myocardial infarction. Although health professionals are not trained to make decisions while taking costs into account, it is essential to remember that the resources, whether from the patient or the health insurance, are limited.
The major limitation of this study was probably the sample size (possible type 1 error). By increasing the sample, one could demonstrate a statistical difference between the groups. Although it is a retrospective analysis, it would be unethical to carry out a prospective study to answer this question, considering the patient would be exposed to risk in the group with DBT ≥ 90minutes. The strong point of this study was the fact that doctors were not affected by the costs in decision-making, therefore reflecting daily clinical practice.
ConclusionsThere was no difference in hospital costs when groups were divided according to the door-to-balloon time. Clinical outcomes were similar and a difference in costs was found for patients with the circumflex artery as the culprit vessel.
Funding sourceNone declared.
Conflicts of interestThe authors declare no conflicts of interest.
Peer review under the responsibility of Sociedade Brasileira de Hemodinâmica e Cardiologia Intervencionista.