In Brazil, it is estimated that approximately 27% of women of childbearing age use oral contraceptives (OC). The presentation and clinical course of acute myocardial infarction (AMI) in these women has yet to be described in Brazil. The aim of this study was to analyze the clinical profile, angiographic characteristics, technical aspects of the procedure, and the outcomes in women using OC who had an AMI and were submitted to primary percutaneous coronary intervention (PCI).
MethodsWomen aged < 55 years who had acute ST segment elevation myocardial infarct and were referred to primary PCI were sequentially included and categorized into two groups: with and without current use of OC.
ResultsWe have included 257 patients, of whom 19 (7.4%) used OC. These patients were younger (42.3 ± 6.2 years vs. 48.4 ± 5.7 years; p < 0.001), with fewer traditional risk factors for coronary artery disease, but had higher serum levels of C-reactive protein and fibrinogen. The delta T was similar (4.00 [1.25 to 6.86] hours vs. 4.50 [2.50 to 7.64] hours; p = 0.54), but the door-to-balloon time was longer in patients taking OC (1.41 [0.58 to 1.73] hours vs. 1.16 [0.91 to 1.51] hour, p = 0.02). These patients were more frequently submitted to thrombus aspiration (52.6% vs. 25.6%; p = 0.04). After the index event, they had no atherothrombotic outcomes in up to 2 years of follow-up (0 vs. 15.2%; p = 0.08).
ConclusionsIn this study, different clinical profiles and outcomes were found among women of reproductive age, users or non-users of OC, and submitted to primary PCI. Studies with a larger number of patients are required to confirm these results.
Em nosso, país estima-se que aproximadamente 27% das mulheres em idade fértil utilizem anticoncepcional oral (ACO). A apresentação e a evolução clínica do infarto agudo do miocárdio (IAM) nessas mulheres ainda não foi descrita em nosso meio. O objetivo do presente estudo foi analisar o perfil clínico, as características angiográficas, os aspectos técnicos do procedimento e os desfechos de usuárias de ACO que tiveram IAM e foram encaminhadas à intervenção coronariana percutânea (ICP) primária.
MétodosMulheres < 55 anos que apresentaram IAM com supradesnivelamento do segmento ST e foram encaminhadas à ICP primária foram sequencialmente incluídas e categorizadas em dois grupos: com e sem uso atual de ACO.
ResultadosIncluímos 257 pacientes, sendo que 19 (7,4%) usavam ACO. Estas eram mais jovens (42,3 ± 6,2 anos vs. 48,4 ± 5,7 anos; p < 0,001), com menos fatores de risco tradicionais para doença arterial coronariana, mas apresentavam proteína C-reativa fibrinogênio séricos mais elevados. O delta T foi semelhante (4,00 [1,25 a 6,86] horas vs. 4,50 [2,50 a 7,64] horas; p = 0,54), mas o tempo porta-balão foi maior nas pacientes em uso de ACO (1,41 [0,58 a 1,73] hora vs. 1,16 [0,91 a 1,51] hora; p = 0,02). Estas pacientes foram mais frequentemente submetidas à tromboaspiração (52,6% vs. 25,6%; p = 0,04). Após o evento índice, elas não apresentaram desfechos aterotrombóticos em até 2 anos de acompanhamento (0 vs. 15,2%; p = 0,08).
ConclusõesNeste estudo, encontramos perfil clínico e desfechos diferentes entre mulheres em idade reprodutiva, usuárias ou não de ACO, e submetidas à ICP primária. Estudos com maior número de pacientes são necessários para confirmar tais resultados.
Acute myocardial infarction (AMI) affects more men than women. In women, during the reproductive years, the pathophysiology of the event is more often related to thrombosis.1 Among the known risk factors for thrombosis is the use of oral contraceptives (OC). This risk is increased in patients with associated conditions, such as smoking, hypertension, obesity, and dyslipidemia.2 The association between venous thrombosis and the use of OC is well defined, and there are several studies showing an increased risk of AMI and ischemic stroke.2–4
In Brazil, it is estimated that approximately 27% of women of childbearing age use OC.5 The presentation and clinical course of AMI in these women has not been described in Brazil, which would be useful to help doctors and patients with the management of this condition. The aim of this study was to analyze the clinical profile, angiographic characteristics, technical aspects of the procedure, and the outcomes in women using OC that had an AMI and were submitted to primary percutaneous coronary intervention (PCI).
MethodsPatientsAll women aged < 55 years who had an acute ST segment elevation myocardial infarction (STEMI) and were referred to primary PCI from 1 December 2009 to 30 May 2015, were considered for the study. Exclusion criteria were delta T > 12hours and refusal to participate. Patients were categorized into two groups: with and without current use of OC, based on the information obtained from medical records.
STEMI was defined according to the following criteria: presence of typical pain at rest associated with ST-segment elevation of at least 1mm in two contiguous leads in the frontal plane, or 2mm in the horizontal plane.
The study was approved by the Ethics Committee of the institution and all patients signed an informed consent form.
ProceduresThe primary PCI procedures were performed as described in the literature.6 Specific technical aspects, such as access route, drug administration, type of stent, and thrombus aspiration were at the discretion of the interventionists.
Trained researchers performed the clinical interviews. Demographic data, risk factors for ischemic heart disease, past medical history, and clinical presentation of the event were collected. Laboratory assessment was performed according to the routine of the institution.
Angiographic evaluations were performed with a previously validated digital electronic system (Siemens Axiom Artis, Siemens, Munich, Germany) and the following variables were assessed: number of vessels with > 50% luminal stenosis, treated coronary artery, and presence of thrombus and angiographic calcification.
Outcomes and definitionsPatients were followed during the in-hospital period and the occurrence of major cardiovascular events (MACE) and their individual components cardiovascular death, recurrent AMI or new PCI, stroke, stent thrombosis, major bleeding, minor bleeding, and acute renal failure were recorded. The follow-up at 1 year and 2 years after the event was carried out by telephone contact, recording the occurrence of MACE, cardiovascular death, recurrent myocardial infarction, ischemic stroke, and stent thrombosis.
Recurrent AMI was considered when ST elevation > 0,1mV recurs, or new Q waves appear, in at least two contiguous leads, particularly when associated with ischemic symptoms for 20minutes or longer. Stroke was defined as focal neurological deficit of sudden onset, irreversible, in the first 24hours. Stent thrombosis was classified as sudden occlusion of the treated vessel, confirmed by angiography. Major bleeding was defined as the occurrence of clinically evident bleeding with a decrease in hemoglobin levels > 5g/dL or hematocrit > 15%, or development of hemorrhagic stroke, or coronary artery bypass graft-related bleeding with transfusion ≥ 5 packed red blood cells in 48hours postoperatively or draining > 1mL in 24hours. Minor bleeding was considered as clinically evident bleeding with a decrease in hemoglobin between 3 and 5g/dL and hematocrit levels between 9 and 15%. Acute renal failure was defined as an increase in serum creatinine ≥ 0.3mg/dL within 48hours, or a 1.5-fold increase in the basal levels, or urine output < 0.5mL/kg/hour for 6hours.
Statistical analysisCategorical variables were described as absolute numbers and percentages, and compared using the Chi-squared test or Fisher's exact test, as appropriate. Continuous variables were described as mean and standard deviation and compared using the t-test. Continuous variables with non-normal distribution were expressed as median and interquartile range and compared using the Mann-Whitney test. The Statistical Package for Social Sciences (SPSS) v. 23.0 for Windows was used and statistical significance was defined by two-tailed p < 0.05.
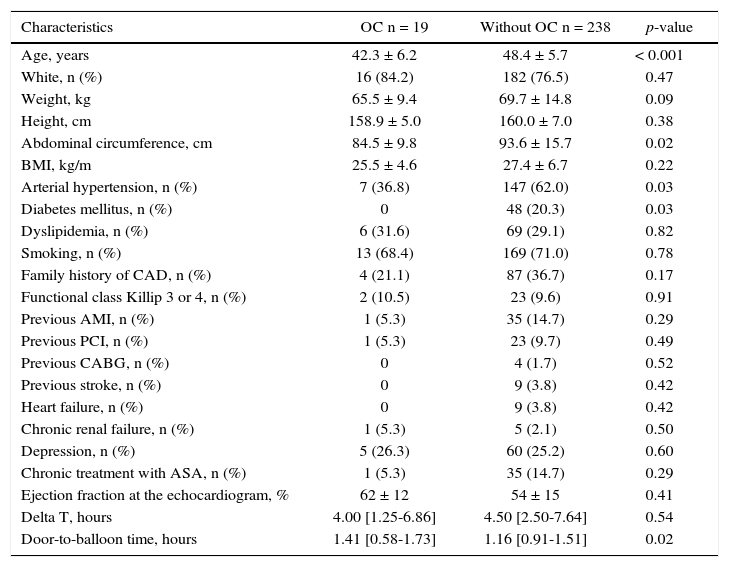
ResultsDuring the study period, 257 patients were included, 19 (7.4%) using OC and 238 who do not make use of OC. Patients using OC were younger (42.3 ± 6.2 years vs. 48.4 ± 5.7 years; p < 0.001), less frequently had arterial hypertension and diabetes, and had a smaller abdominal circumference (Table 1). The time of arrival at the hospital after symptom onset was similar between the groups (4.00 [1.25 to 6.86] hours vs. 4.50 [2.50 to 7.64] hours; p = 0.54), but the door-to-balloon time was longer in patients using OC (1.41 [0.58 to 1.73] hour vs. 1.16 [0.91 to 1.51] hour; p = 0.02).
Clinical characteristics.
| Characteristics | OC n = 19 | Without OC n = 238 | p-value |
|---|---|---|---|
| Age, years | 42.3 ± 6.2 | 48.4 ± 5.7 | < 0.001 |
| White, n (%) | 16 (84.2) | 182 (76.5) | 0.47 |
| Weight, kg | 65.5 ± 9.4 | 69.7 ± 14.8 | 0.09 |
| Height, cm | 158.9 ± 5.0 | 160.0 ± 7.0 | 0.38 |
| Abdominal circumference, cm | 84.5 ± 9.8 | 93.6 ± 15.7 | 0.02 |
| BMI, kg/m | 25.5 ± 4.6 | 27.4 ± 6.7 | 0.22 |
| Arterial hypertension, n (%) | 7 (36.8) | 147 (62.0) | 0.03 |
| Diabetes mellitus, n (%) | 0 | 48 (20.3) | 0.03 |
| Dyslipidemia, n (%) | 6 (31.6) | 69 (29.1) | 0.82 |
| Smoking, n (%) | 13 (68.4) | 169 (71.0) | 0.78 |
| Family history of CAD, n (%) | 4 (21.1) | 87 (36.7) | 0.17 |
| Functional class Killip 3 or 4, n (%) | 2 (10.5) | 23 (9.6) | 0.91 |
| Previous AMI, n (%) | 1 (5.3) | 35 (14.7) | 0.29 |
| Previous PCI, n (%) | 1 (5.3) | 23 (9.7) | 0.49 |
| Previous CABG, n (%) | 0 | 4 (1.7) | 0.52 |
| Previous stroke, n (%) | 0 | 9 (3.8) | 0.42 |
| Heart failure, n (%) | 0 | 9 (3.8) | 0.42 |
| Chronic renal failure, n (%) | 1 (5.3) | 5 (2.1) | 0.50 |
| Depression, n (%) | 5 (26.3) | 60 (25.2) | 0.60 |
| Chronic treatment with ASA, n (%) | 1 (5.3) | 35 (14.7) | 0.29 |
| Ejection fraction at the echocardiogram, % | 62 ± 12 | 54 ± 15 | 0.41 |
| Delta T, hours | 4.00 [1.25-6.86] | 4.50 [2.50-7.64] | 0.54 |
| Door-to-balloon time, hours | 1.41 [0.58-1.73] | 1.16 [0.91-1.51] | 0.02 |
OC: oral contraceptives; BMI: body mass index; CAD: coronary artery disease; AMI: acute myocardial infarction; PCI: percutaneous coronary intervention; CABG: coronary artery bypass surgery; ASA: acetyl salicylic acid.
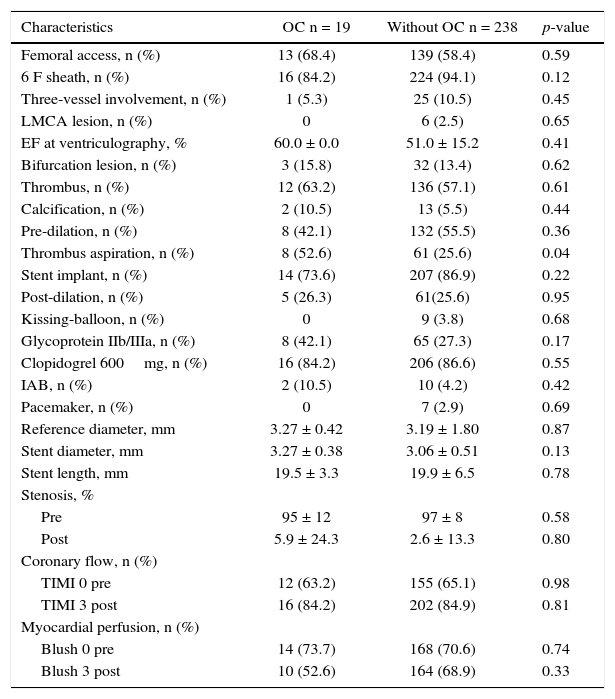
Regarding the angiographic and procedure characteristics, the groups were similar in most characteristics (Table 2). The femoral access was the most often used (68.4% vs. 58.4%; p = 0.59), as well as the 6 F sheath (84.2% vs. 94.1%; p = 0.12). A minority of patients had three-vessel involvement (5.3% vs. 10.5%; p = 0.45) and preserved left ventricular ejection fraction (60.0 ± 0.0% vs. 51.0 ± 15.2%; p = 0.41). The treated vessels had a reference diameter of 3.27 ± 0.42mm vs. 3.19 ± 1.80mm (p = 0.87), percentage of stenosis of 95 ± 12% vs. 97 ± 8% (p = 0.58), and Thrombolysis in Myocardial Infarction (TIMI) flow 0 in 63.2% vs. 65.1% (p = 0.98). A visible thrombus was detected in 63.2% vs. 57.1% (p = 0.61) of cases and thrombus aspiration was most often performed in the group of women using OC (52.6% vs. 25.6%; p = 0.04). TIMI 3 post flow was obtained in 84.2% vs. 84.9% (p = 0.81).
Angiographic and procedural characteristics.
| Characteristics | OC n = 19 | Without OC n = 238 | p-value |
|---|---|---|---|
| Femoral access, n (%) | 13 (68.4) | 139 (58.4) | 0.59 |
| 6 F sheath, n (%) | 16 (84.2) | 224 (94.1) | 0.12 |
| Three-vessel involvement, n (%) | 1 (5.3) | 25 (10.5) | 0.45 |
| LMCA lesion, n (%) | 0 | 6 (2.5) | 0.65 |
| EF at ventriculography, % | 60.0 ± 0.0 | 51.0 ± 15.2 | 0.41 |
| Bifurcation lesion, n (%) | 3 (15.8) | 32 (13.4) | 0.62 |
| Thrombus, n (%) | 12 (63.2) | 136 (57.1) | 0.61 |
| Calcification, n (%) | 2 (10.5) | 13 (5.5) | 0.44 |
| Pre-dilation, n (%) | 8 (42.1) | 132 (55.5) | 0.36 |
| Thrombus aspiration, n (%) | 8 (52.6) | 61 (25.6) | 0.04 |
| Stent implant, n (%) | 14 (73.6) | 207 (86.9) | 0.22 |
| Post-dilation, n (%) | 5 (26.3) | 61(25.6) | 0.95 |
| Kissing-balloon, n (%) | 0 | 9 (3.8) | 0.68 |
| Glycoprotein IIb/IIIa, n (%) | 8 (42.1) | 65 (27.3) | 0.17 |
| Clopidogrel 600mg, n (%) | 16 (84.2) | 206 (86.6) | 0.55 |
| IAB, n (%) | 2 (10.5) | 10 (4.2) | 0.42 |
| Pacemaker, n (%) | 0 | 7 (2.9) | 0.69 |
| Reference diameter, mm | 3.27 ± 0.42 | 3.19 ± 1.80 | 0.87 |
| Stent diameter, mm | 3.27 ± 0.38 | 3.06 ± 0.51 | 0.13 |
| Stent length, mm | 19.5 ± 3.3 | 19.9 ± 6.5 | 0.78 |
| Stenosis, % | |||
| Pre | 95 ± 12 | 97 ± 8 | 0.58 |
| Post | 5.9 ± 24.3 | 2.6 ± 13.3 | 0.80 |
| Coronary flow, n (%) | |||
| TIMI 0 pre | 12 (63.2) | 155 (65.1) | 0.98 |
| TIMI 3 post | 16 (84.2) | 202 (84.9) | 0.81 |
| Myocardial perfusion, n (%) | |||
| Blush 0 pre | 14 (73.7) | 168 (70.6) | 0.74 |
| Blush 3 post | 10 (52.6) | 164 (68.9) | 0.33 |
OC: oral contraceptives; LMCA: left main coronary artery; EF: ejection fraction; IAB: intra-aortic balloon; TIMI: Thrombolysis in Myocardial Infarction.
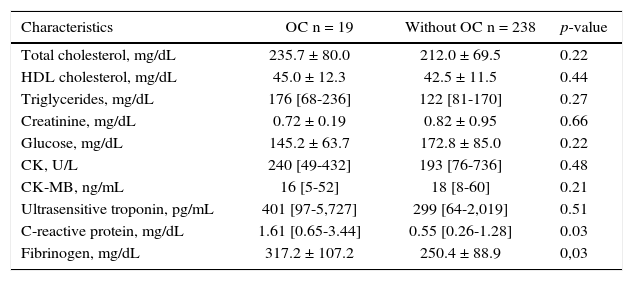
Table 3 compares the laboratory parameters between groups. Women using OC had higher levels of C-reactive protein and fibrinogen.
Laboratory characteristics.
| Characteristics | OC n = 19 | Without OC n = 238 | p-value |
|---|---|---|---|
| Total cholesterol, mg/dL | 235.7 ± 80.0 | 212.0 ± 69.5 | 0.22 |
| HDL cholesterol, mg/dL | 45.0 ± 12.3 | 42.5 ± 11.5 | 0.44 |
| Triglycerides, mg/dL | 176 [68-236] | 122 [81-170] | 0.27 |
| Creatinine, mg/dL | 0.72 ± 0.19 | 0.82 ± 0.95 | 0.66 |
| Glucose, mg/dL | 145.2 ± 63.7 | 172.8 ± 85.0 | 0.22 |
| CK, U/L | 240 [49-432] | 193 [76-736] | 0.48 |
| CK-MB, ng/mL | 16 [5-52] | 18 [8-60] | 0.21 |
| Ultrasensitive troponin, pg/mL | 401 [97-5,727] | 299 [64-2,019] | 0.51 |
| C-reactive protein, mg/dL | 1.61 [0.65-3.44] | 0.55 [0.26-1.28] | 0.03 |
| Fibrinogen, mg/dL | 317.2 ± 107.2 | 250.4 ± 88.9 | 0,03 |
OC: oral contraceptives; HDL: high density lipoprotein; CK: creatine kinase; CK-MB: creatine kinase MB isoenzyme.
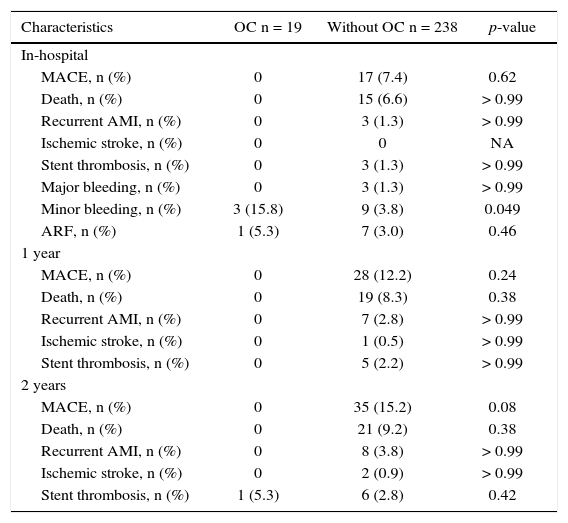
Table 4 shows the clinical outcomes. During the in-hospital phase, there were no differences regarding MACE or its individual components, only higher occurrence of minor bleeding in patients using OC. During the 2-year follow-up, there were no clinical events after hospital discharge in the group using OC, with the exception of one case of very late stent thrombosis. The other group had a cumulative event occurrence resulting in a tendency to a higher MACE (0 vs. 15.2%; p = 0.08).
Clinical data.
| Characteristics | OC n = 19 | Without OC n = 238 | p-value |
|---|---|---|---|
| In-hospital | |||
| MACE, n (%) | 0 | 17 (7.4) | 0.62 |
| Death, n (%) | 0 | 15 (6.6) | > 0.99 |
| Recurrent AMI, n (%) | 0 | 3 (1.3) | > 0.99 |
| Ischemic stroke, n (%) | 0 | 0 | NA |
| Stent thrombosis, n (%) | 0 | 3 (1.3) | > 0.99 |
| Major bleeding, n (%) | 0 | 3 (1.3) | > 0.99 |
| Minor bleeding, n (%) | 3 (15.8) | 9 (3.8) | 0.049 |
| ARF, n (%) | 1 (5.3) | 7 (3.0) | 0.46 |
| 1 year | |||
| MACE, n (%) | 0 | 28 (12.2) | 0.24 |
| Death, n (%) | 0 | 19 (8.3) | 0.38 |
| Recurrent AMI, n (%) | 0 | 7 (2.8) | > 0.99 |
| Ischemic stroke, n (%) | 0 | 1 (0.5) | > 0.99 |
| Stent thrombosis, n (%) | 0 | 5 (2.2) | > 0.99 |
| 2 years | |||
| MACE, n (%) | 0 | 35 (15.2) | 0.08 |
| Death, n (%) | 0 | 21 (9.2) | 0.38 |
| Recurrent AMI, n (%) | 0 | 8 (3.8) | > 0.99 |
| Ischemic stroke, n (%) | 0 | 2 (0.9) | > 0.99 |
| Stent thrombosis, n (%) | 1 (5.3) | 6 (2.8) | 0.42 |
OC: oral contraceptives; MACE: major cardiovascular events; AMI: acute myocardial infarction; NA: not applicable; ARF: acute renal failure.
Women using OC referred to primary PCI had less severe clinical profile than women of reproductive age who do not use OC, but had higher levels of inflammatory and thrombogenic markers. They were submitted to myocardial reperfusion at a later date and required more thrombus aspiration procedures. After the index event, they tended to not have new atherothrombotic events in up to 2 years of follow-up.
The lower mean age and the fewer number of comorbidities in women using OC were similar to those described in previous studies, and could be explained by differences in the pathophysiology of AMI in both groups. In women using OC, the influence of thrombosis would be greater, whereas in those who did not use OC, the natural progression of atherosclerosis with atherosclerotic plaque rupture and/or erosion, associated with increased cardiovascular risk by multiple risk factors, would have a leading role.1,9
Recently, Karabay et al.10 evaluated women submitted to primary PCI using fourth-generation OC and demonstrated greater thrombotic burden, lower incidence of final TIMI 3 flow, and more frequent multivessel thrombosis. In the present study, the rate of angiographically visible thrombus in the two groups was not statistically different, but no dedicated score was used to assess thrombotic burden. However, a very significant difference was found regarding the use of thrombus aspiration, which was two times higher in women using OC; that, in turn, would suggest that the criteria used to define thrombus were not sensitive enough to detect a significant difference. The observation of elevated C-reactive protein levels in women using OC suggests an increase in the inflammatory status of these patients, which has already been demonstrated in the study by Zakharova et al.11
OC have been used in clinical practice for family planning for more than 60 years. Since then, great advances have been made regarding therapeutic options, doses, and safety of used formulations.12 However, women in special clinical situations and/or in the presence of comorbidities require attention regarding the use of hormonal contraceptives. In the present study, among the women with AMI who used OC, 68.4% were smokers, 36.8% were hypertensive, and 5.3% had a previous AMI – clinical conditions that classify the use of OC as category 3 (risks outweigh the benefits) or 4 (unacceptable use), according to the eligibility criteria for use of contraceptive methods of the World Health Organization.13 Thus, these findings emphasize the importance of careful assessment and identification of cardiovascular risk factors when choosing and prescribing OC.
Furthermore, the probable suspension of these drugs after the acute coronary episode contributed to the rare occurrence of other atherothrombotic events in up to 2 years of follow-up, which did not happen in the other group, with a more severe cardiovascular risk profile and cumulative occurrence of new events, which resulted in a higher MACE.
In the present study, there was no available information on the oral contraceptive formulation, dose, or type of estrogen or progestogen that the patients used, which can be considered a limitation of this analysis. Data were prospectively collected by a team of dedicated researchers, but the decision to analyze and compare users and non-users of OC was performed retrospectively and based on medical records. More accurate analyses of thrombotic burden through dedicated scores or optical coherence tomography were not available, and can also be considered limitations of the present analysis. The number of patients using OC included in this study was small, although it can be favorably compared with several reports in the literature.10
ConclusionsWomen who use oral contraceptives submitted to primary percutaneous coronary intervention were younger and had fewer traditional risk factors for coronary artery disease than those who did not use oral contraceptives, in addition to having higher serum levels of fibrinogen and C-reactive protein. They underwent myocardial reperfusion at a later stage and required more thrombus aspiration procedures. After the index event, they tended to not have atherothrombotic outcomes in up to 2 years of follow-up. Studies with a larger number of patients are required to confirm these results.
Funding sourceNone declared.
Conflicts of interestThe authors declare no conflicts of interest.
The authors would like to thank their colleagues André Manica, Alexandre Azmus, Carlos Roberto Cardoso, Cristiano Oliveira Cardoso, Cláudio Antonio Ramos de Moraes, Cláudio Vasquez de Moraes, Flavio Celso Leboute, Henrique Basso Gomes, Julio Teixeira, La Hore Correa Rodrigues, Mauro Regis Silva Moura, and Rogério Sarmento Leite for their participation in the performance of primary percutaneous coronary intervention procedures.
Peer review under the responsibility of Sociedade Brasileira de Hemodinâmica e Cardiologia Intervencionista.