In clinical practice, type-1 (coronary thrombosis) and type-2 (imbalance between oxygen demand and supply) acute myocardial infarction (AMI) are not clearly differentiated. The aim of this study was to evaluate the prevalence and etiology of type-2 AMI and compare its profile with that of type-1 AMI.
MethodsPatients admitted with ST-segment elevation AMI (STEMI)<12hours of symptom onset, and referred for coronary angiography, from 2009 to 2013, were analyzed.
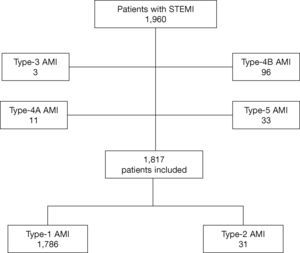
ResultsThere were 1,960 patients included; 1,817 were analyzed, of whom 1,786 (98.3%) had type-1 AMI, and 31 (1.7%), type-2. All patients with type-2 AMI showed no significant coronary lesions, and 36% of the cases had apical dyskinesia. Type-2 AMI patients had, in general, a clinical and laboratory profile that was similar to those with type-1, except for the younger age, lower levels of myocardial necrosis markers, higher probability of having pre-TIMI 3 flow and higher left ventricular ejection fraction. At 30 days, mortality (3.2 vs. 9.0%; p=0.23) and the occurrence of death, reinfarction, or need for target-vessel revascularization (3.2 vs. 13.0%; p=0.09) were numerically lower in type-2 AMI.
ConclusionsFew patients with STEMI were classified as type-2; they had structural abnormalities, isolated or associated with the absence of significant lesions; showed little difference regarding the clinical and laboratory profile, and similar clinical outcomes at 30 days, when compared to patients with type-1 AMI.
Na prática clínica, os tipos 1 (trombose coronariana) e 2 (desequilíbrio entre a demanda e oferta de oxigênio) de infarto agudo do miocárdio (IAM) não são claramente distinguidos. O objetivo deste estudo foi avaliar a prevalência e a etiologia do IAM tipo 2, e comparar seu perfil com o do tipo 1.
MétodosForam analisados pacientes admitidos com IAM com supradesnivelamento do segmento ST (IAMCST) com < 12 horas, encaminhados para coronariografia, no período de 2009 a 2013.
ResultadosForam incluídos 1.960 pacientes, sendo 1.817 analisados, dos quais 1.786 (98,3%) com IAM tipo 1 e 31 (1,7%) do tipo de 2. Todos os pacientes com IAM tipo 2 apresentaram coronárias sem lesões significativas e, em 36% dos casos, discinesia apical. Os pacientes com IAM tipo 2 apresentaram, em geral, perfil clínico e laboratorial semelhante aos do tipo 1, com exceção da idade mais jovem, menores níveis de marcadores de necrose miocárdica, maior probabilidade de apresentarem fluxo TIMI 3 pré e maior fração de ejeção do ventrículo esquerdo. Aos 30 dias, a mortalidade (3,2 vs. 9,0%; p=0,23) e a ocorrência de morte, reinfarto ou necessidade de revascularização do vaso-alvo (3,2 vs. 13,0%; p=0,09) foram numericamente menores no IAM tipo 2.
ConclusõesUma pequena fração de pacientes com IAMCST foi classificada como de tipo 2; exibiram anormalidades estruturais isoladas ou associadas à ausência de lesões significativas; mostraram poucas diferenças no perfil clínico e laboratorial, e desfechos clínicos semelhantes aos 30 dias, comparados aos pacientes com IAM tipo 1.
Data from the Department of Informatics of the Unified Health System (DATASUS) 2013 show that acute myocardial infarction (AMI) was the main cause of death from heart disease in Brazil, with an increase of 48% observed between 1996 and 2011.1 If this trend persists, it is expected that AMI will become the main isolated cause of death by 2020.2
The universal definition jointly developed by the European Society of Cardiology (ESC), American College of Cardiology Foundation (ACCF), American Heart Association (AHA), and World Heart Federation (WHF) subdivides AMI into five types.3,4 Type-1 AMI is a spontaneous event, resulting from coronary thrombosis, which results, in turn, from disruption, fracture, or erosion of the atherosclerotic plaque.5,6 The imbalance between oxygen demand and supply characterizes type-2 AMI, which occurs in several conditions not associated with atherosclerotic plaque events. This imbalance can occur due to endothelial dysfunction, coronary vasospasm, coronary embolism, tachyarrhythmias and bradyarrhythmias, anemia, respiratory failure, hypotension, and hypertension, with or without left ventricular hypertrophy. The other types include type-3 AMI, which is defined when patients suffer cardiac death, with symptoms suggestive of myocardial ischemia, accompanied by presumed new ischemic electrocardiographic changes or new left bundle branch block, but without available biomarker values. Type-4A is associated with percutaneous coronary intervention, and type 4B occurs in the presence of stent thrombosis. Type-5 characterizes the AMI associated with coronary artery bypass surgery.
In clinical practice, type-1 and type-2 AMI are not clearly differentiated,7 and the electrocardiographic and biochemical characteristics can be similar.8,9 Thus, the aim of this study was to evaluate the prevalence and etiology of type-2 AMI, compare the risk factors, clinical and laboratory characteristics, and outcomes of these patients with those of type-1, in a cohort of patients undergoing coronary angiography for ST-segment elevation AMI (STEMI) in a referral cardiology hospital.
MethodsAll patients were prospectively and sequentially enrolled at the hospital emergency department with STEMI, with < 12hours of symptom onset, and submitted to coronary angiography in the period from December 2009 to December 2013. The exclusion criteria included the patient's refusal to participate the study and age < 18 years. The project was approved by the local research ethics committee. All patients or their family members signed an informed consent. The initial interview with the patient, carried out upon arrival at the hospital emergency department, included the recording of demographic data, risk factors for ischemic heart disease, and clinical presentation of the event.
STEMI was defined by electrocardiographic abnormalities (presence of new, or presumably new, ST-segment elevation > 0.1mV in two or more contiguous leads), clinical presentation consistent with acute ischemia, and increase in myocardial necrosis markers (myocardial isoenzyme of creatine kinase - CK-MB with at least one value above the 99th percentile upper reference limit or, in the absence of CK-MB, total CK greater than twice the upper limit of normal, or troponin elevation) within the 24hours of symptom onset.10 Hypertension, diabetes mellitus, and dyslipidemia were classified according to the Guidelines of the Brazilian Society of Cardiology.11–13 The criterion used for family history of coronary artery disease (CAD) was the occurrence of AMI in first-degree male relatives younger than 55 years or in females younger than 65 years.14
Medications used in the initial patient care consisted of acetylsalicylic acid, loading dose of 300mg, and clopidogrel 300 to 600mg, administered immediately after the patient's arrival in the emergency room. Unfractionated heparin at a dose of 70 to 100 IU/kg was used in the emergency or cath lab room.
Angiographic evaluations were performed using a previously validated digital electronic system. The number of vessels with lesions > 50%, the culprit vessel, and the presence of coronary calcification were assessed. The AMI-type classification was performed after the angiography, by the interventionists, according to the previously mentioned criteria.3,4 All patients’ images and reports were reviewed to confirm type-2 AMI, and to assess other angiographic findings.
Patient follow-up was performed during hospital stay and after discharge, by telephone contact at 30 days.
Statistical analysisCategorical variables were expressed as frequencies and percentages, and were compared with the Chi-squared test or Fisher's exact test. Quantitative variables were expressed as mean and standard deviation, or median and interquartile range, and compared by analysis of variance (ANOVA) or the Tukey test for multiple comparisons, in the case of normal distribution, or the Kruskal-Wallis test for asymmetric distribution of variables. Data were analyzed using Statistical Package for the Social Sciences (SPSS) for Windows, version 19.0 (IBM Corp., Armonk, USA). The values considered significant were those with p<0.05.
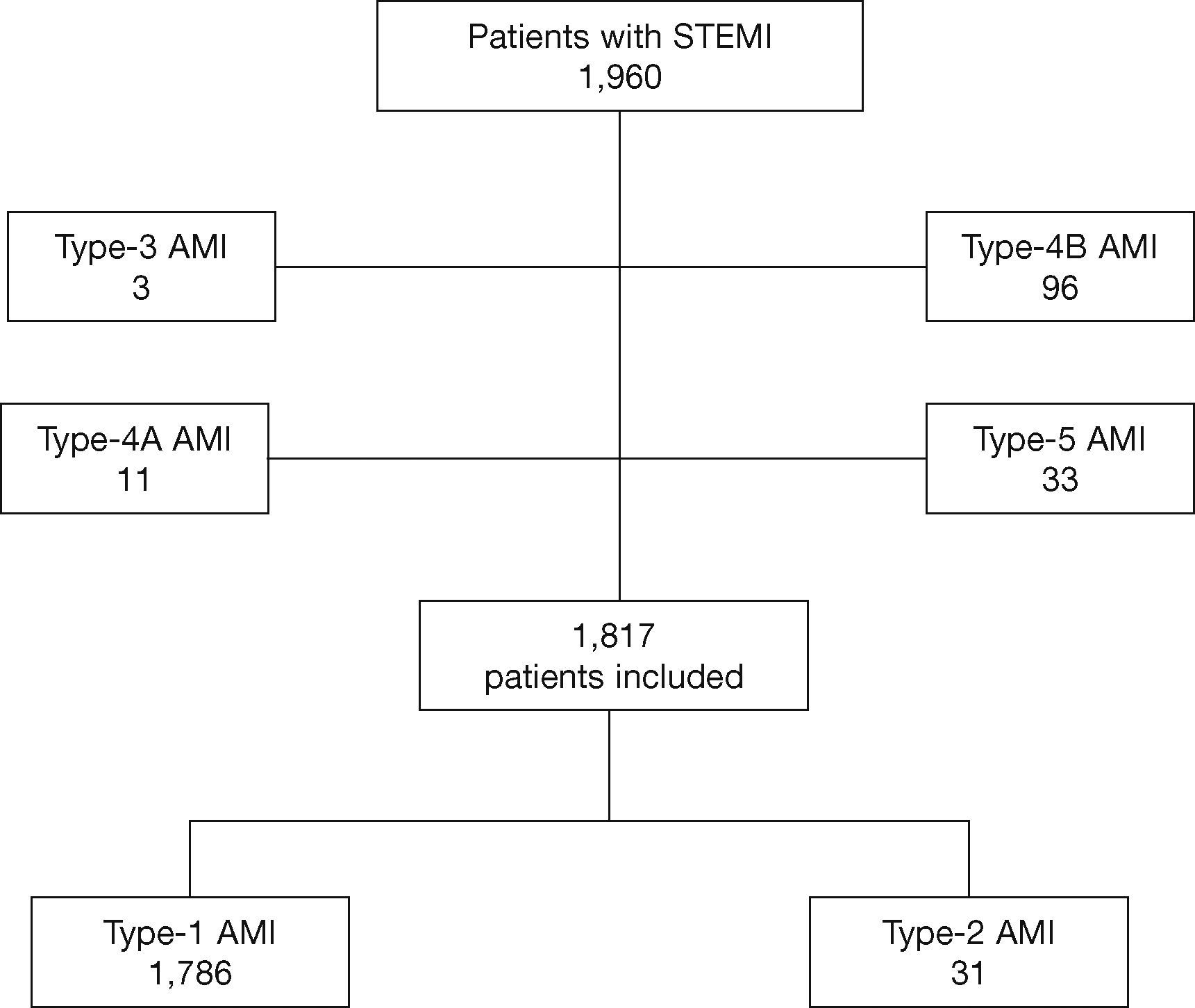
ResultsDuring the described period, 1,960 patients were assessed and 1,817 were included in this study: 1,786 (98.3%) with type-1 AMI and 31 (1.7%) with type-2 AMI (Fig. 1).
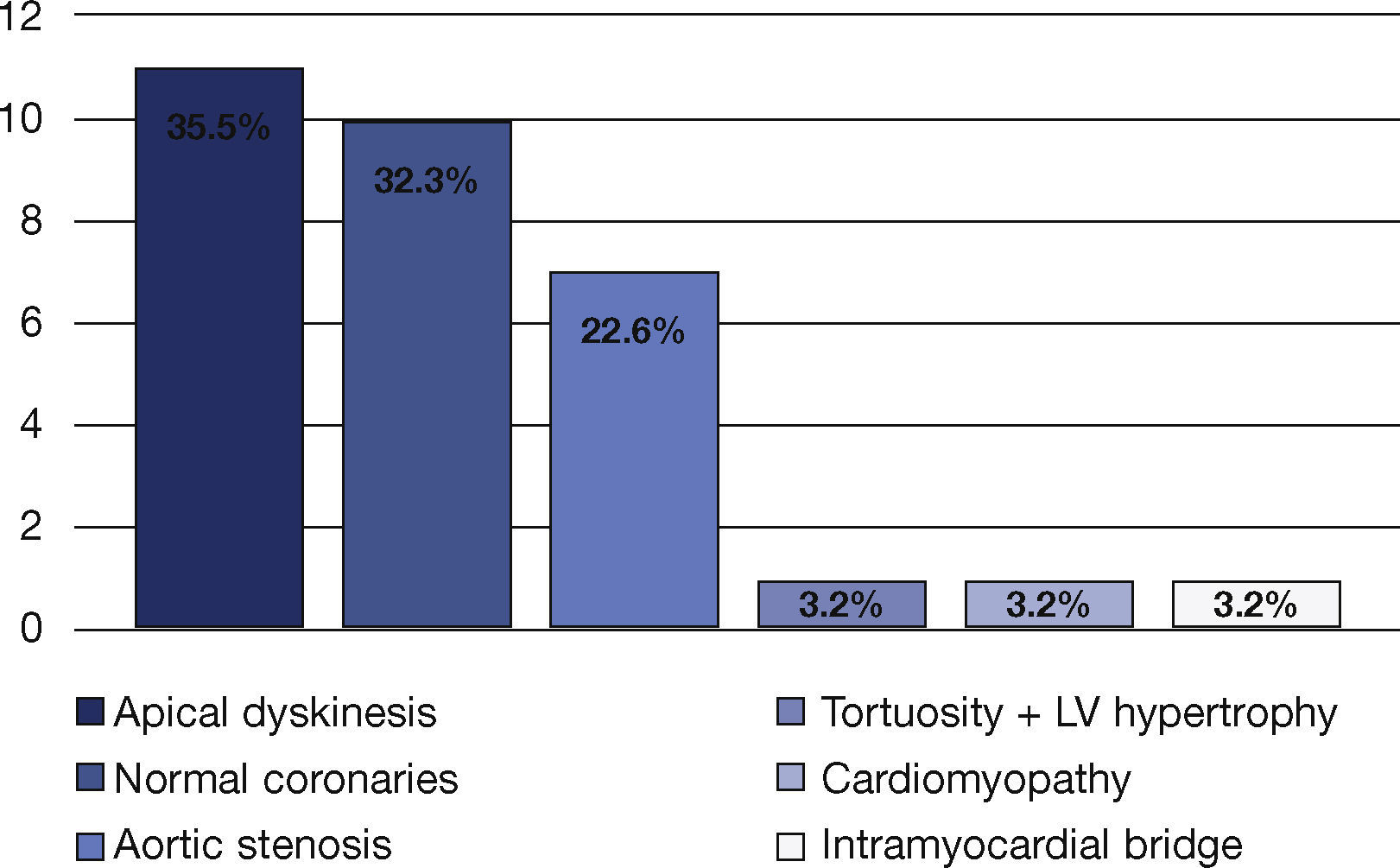
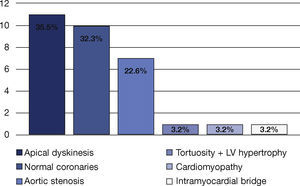
All patients with type-2 AMI had coronaries with absence of or no significant lesions. Additional findings included apical dyskinesia in 35.5% of cases, coronary tortuosity and left ventricular hypertrophy in 32.3%, and 22.6% with normal coronary arteries. One case of intramyocardial bridge (3.2%),another of cardiomyopathy (3.2%), and a third of aortic stenosis (3.2%) were also observed (Fig. 2).
Among the clinical findings, this study found patients who had used cocaine (n=1), using oral contraceptives (n=1), with anemia (n=1), ventricular fibrillation (n=1), respiratory disease (n=2), seropositivity for the human immunodeficiency virus (HIV; n=2), under acute psychological stress (n=3), or with suspected myocarditis (n=3).
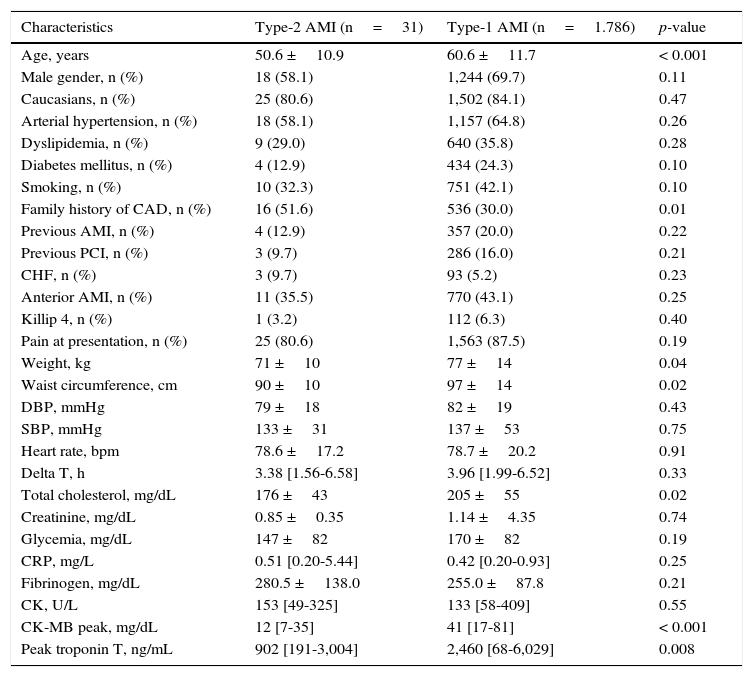
When comparing the groups, patients with type-2 AMI were younger (50.6 ±10.9 years vs. 60.6 ±11.7 years; p<0.001), more frequently had a family history of CAD (51.6% vs. 30.0%; p=0.01), and had lower abdominal circumference (90 ±10cm vs. 97 ±14cm; p=0.02). They also had lower values of myocardial necrosis markers, such as CK-MB (12 [7-35] mg/dL vs. 41 [17-81] mg/dL; p<0.001) and ultrasensitive troponin T (902 [191–3,004] ng/mL vs. 2,460 [68–6,029] ng/mL; p=0.008). Although C reactive protein was numerically higher in patients with type-2 AMI, the difference was not significant (0.51 [0.21–5.44] mg/L vs. 0.42 [0.20–0.93] mg/L; p=0.25). Regarding the lipid profile, a difference was found only in the total cholesterol, which was lower (176 ±43mg/L vs. 205 ±55mg/dL; p=0.02) in these patients (Table 1).
Clinical and laboratory characteristics.
| Characteristics | Type-2 AMI (n=31) | Type-1 AMI (n=1.786) | p-value |
|---|---|---|---|
| Age, years | 50.6 ±10.9 | 60.6 ±11.7 | < 0.001 |
| Male gender, n (%) | 18 (58.1) | 1,244 (69.7) | 0.11 |
| Caucasians, n (%) | 25 (80.6) | 1,502 (84.1) | 0.47 |
| Arterial hypertension, n (%) | 18 (58.1) | 1,157 (64.8) | 0.26 |
| Dyslipidemia, n (%) | 9 (29.0) | 640 (35.8) | 0.28 |
| Diabetes mellitus, n (%) | 4 (12.9) | 434 (24.3) | 0.10 |
| Smoking, n (%) | 10 (32.3) | 751 (42.1) | 0.10 |
| Family history of CAD, n (%) | 16 (51.6) | 536 (30.0) | 0.01 |
| Previous AMI, n (%) | 4 (12.9) | 357 (20.0) | 0.22 |
| Previous PCI, n (%) | 3 (9.7) | 286 (16.0) | 0.21 |
| CHF, n (%) | 3 (9.7) | 93 (5.2) | 0.23 |
| Anterior AMI, n (%) | 11 (35.5) | 770 (43.1) | 0.25 |
| Killip 4, n (%) | 1 (3.2) | 112 (6.3) | 0.40 |
| Pain at presentation, n (%) | 25 (80.6) | 1,563 (87.5) | 0.19 |
| Weight, kg | 71 ±10 | 77 ±14 | 0.04 |
| Waist circumference, cm | 90 ±10 | 97 ±14 | 0.02 |
| DBP, mmHg | 79 ±18 | 82 ±19 | 0.43 |
| SBP, mmHg | 133 ±31 | 137 ±53 | 0.75 |
| Heart rate, bpm | 78.6 ±17.2 | 78.7 ±20.2 | 0.91 |
| Delta T, h | 3.38 [1.56-6.58] | 3.96 [1.99-6.52] | 0.33 |
| Total cholesterol, mg/dL | 176 ±43 | 205 ±55 | 0.02 |
| Creatinine, mg/dL | 0.85 ±0.35 | 1.14 ±4.35 | 0.74 |
| Glycemia, mg/dL | 147 ±82 | 170 ±82 | 0.19 |
| CRP, mg/L | 0.51 [0.20-5.44] | 0.42 [0.20-0.93] | 0.25 |
| Fibrinogen, mg/dL | 280.5 ±138.0 | 255.0 ±87.8 | 0.21 |
| CK, U/L | 153 [49-325] | 133 [58-409] | 0.55 |
| CK-MB peak, mg/dL | 12 [7-35] | 41 [17-81] | < 0.001 |
| Peak troponin T, ng/mL | 902 [191-3,004] | 2,460 [68-6,029] | 0.008 |
AMI: acute myocardial infarction; CAD: coronary artery disease; PCI: percutaneous coronary intervention; CHF: congestive heart failure; DBP: diastolic blood pressure; SBP: systolic blood pressure; CRP: C reactive protein; CK: creatine-kinase; CK-MB: creatine kinase myocardial isoenzyme.
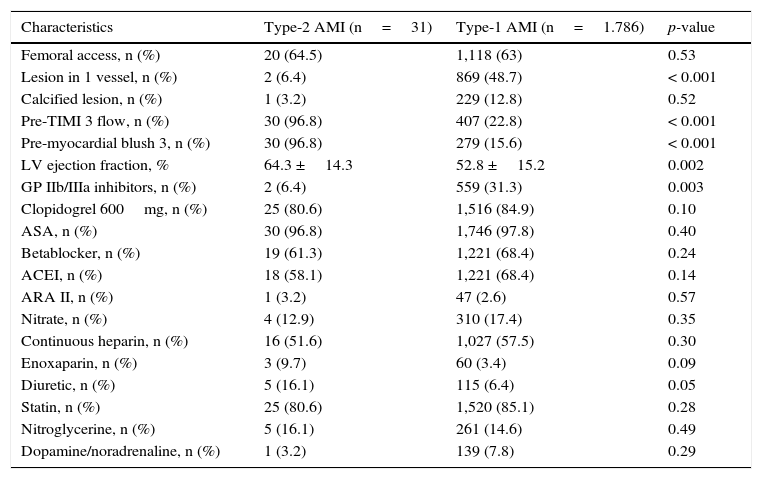
In Table 2, it can be observed that the group of patients with type-2 AMI had fewer patients with single-vessel involvement (6.4% vs. 48.7%; p<0.001), higher probability of having pre-TIMI 3 flow (96.8% vs. 22.8%; p<0.001) and pre-myocardial blush grade 3 (96.8% vs. 15.6%; p<0.001), as well as higher ejection fraction (64.3 ±14.3% vs. 52.8 ±15.2%, p=0.002). As for medications, patients with type-2 AMI received less glycoprotein IIb/IIIa inhibitors (6.4% vs. 31.3%; p=0.003).
Angiographic characteristics and medications used in the first 24hours.
| Characteristics | Type-2 AMI (n=31) | Type-1 AMI (n=1.786) | p-value |
|---|---|---|---|
| Femoral access, n (%) | 20 (64.5) | 1,118 (63) | 0.53 |
| Lesion in 1 vessel, n (%) | 2 (6.4) | 869 (48.7) | < 0.001 |
| Calcified lesion, n (%) | 1 (3.2) | 229 (12.8) | 0.52 |
| Pre-TIMI 3 flow, n (%) | 30 (96.8) | 407 (22.8) | < 0.001 |
| Pre-myocardial blush 3, n (%) | 30 (96.8) | 279 (15.6) | < 0.001 |
| LV ejection fraction, % | 64.3 ±14.3 | 52.8 ±15.2 | 0.002 |
| GP IIb/IIIa inhibitors, n (%) | 2 (6.4) | 559 (31.3) | 0.003 |
| Clopidogrel 600mg, n (%) | 25 (80.6) | 1,516 (84.9) | 0.10 |
| ASA, n (%) | 30 (96.8) | 1,746 (97.8) | 0.40 |
| Betablocker, n (%) | 19 (61.3) | 1,221 (68.4) | 0.24 |
| ACEI, n (%) | 18 (58.1) | 1,221 (68.4) | 0.14 |
| ARA II, n (%) | 1 (3.2) | 47 (2.6) | 0.57 |
| Nitrate, n (%) | 4 (12.9) | 310 (17.4) | 0.35 |
| Continuous heparin, n (%) | 16 (51.6) | 1,027 (57.5) | 0.30 |
| Enoxaparin, n (%) | 3 (9.7) | 60 (3.4) | 0.09 |
| Diuretic, n (%) | 5 (16.1) | 115 (6.4) | 0.05 |
| Statin, n (%) | 25 (80.6) | 1,520 (85.1) | 0.28 |
| Nitroglycerine, n (%) | 5 (16.1) | 261 (14.6) | 0.49 |
| Dopamine/noradrenaline, n (%) | 1 (3.2) | 139 (7.8) | 0.29 |
TIMI: Thrombolysis In Myocardial Infarction; LV: left ventricle; GP: glycoprotein; ASA: acetylsalicylic acid; ACEI: angiotensin-converting enzyme inhibitors; ARA II: angiotensin-II receptor antagonists.
At 30 days of follow-up, patients with type-2 AMI had numerically lower mortality (3.2% vs. 9.0%; p=0.23) and occurrence of death, reinfarction, and need for new revascularization of the target vessel (3.2% vs. 13.0%, p=0.09) than type-1 AMI patients, but without reaching statistical significance.
DiscussionThe main findings of this study demonstrate risk profile, previous history, clinical presentation, and laboratory characteristics that are generally similar between patients with type-1 and type-2 AMI, which confirms the difficulty in the differential diagnosis between such patients. Studies comparing angiographic data in type-1 and type-2 AMI are scarce in the literature.7,9,15 The prevalence of type-2 AMI is quite controversial, ranging from 2 to 26%.16–18 Other studies show an AMI incidence of 2.8% in patients with normal coronary arteries.19
Regarding the absence of a significant obstructive lesion, Kang et al.20 reported that approximately 4% of 8,500 patients with AMI showed normal coronary arteries, and that the clinical features, outcomes, and prognosis were similar to those of patients with lesions in one or two vessels. The difference in mortality was only observed for patients with three-vessel involvement. The present study observed a prevalence of approximately 2% of patients with type-2 AMI. Similar to the findings of Kang et al.,20 the group of patients with type-2 AMI was younger, had a family history of CAD, and had lower waist circumference when compared to the type-1 patients.
In the present study, it was observed that, despite the absence of significant lesions, the patients had coronary tortuosity, left ventricular hypertrophy, and apical dyskinesia, among others. Macruz et al.21 developed an index to determine the ratio between the length of the tortuous artery and its normal length, thereby defining coronary tortuosity. Other studies used the index by Macruz et al., such as Bastos and Cunha,22 who found 17 isolated or associated abnormalities in patients with normal coronary arteries. Isolated tortuosity was found in 19 patients among the 105 assessed patients; ventricular hypertrophy, together with tortuosity, was found in 24 patients, and intramyocardial bridge in six patients, only to name a few findings. In the present cases, ventricular hypertrophy and tortuosity were found in ten patients, and intramyocardial bridge in only one.
Apical dyskinesia, which was found in a little more than one-third of the patients with type-2 AMI, is a characteristic compatible with Takotsubo syndrome, whose clinical presentation is chest pain, ST-segment elevation on the electrocardiogram, and increase in biomarkers, simulating an acute coronary syndrome, but with normal coronary arteries,23,24 with or without ventricular dysfunction. Absence of significant obstructive coronary artery disease and reversibility of left ventricular contractility dysfunction are the important aspects for this diagnosis.25–27 Perhaps, due to the possible inclusion of these patients in the type-2 AMI sample, a higher ejection fraction was obtained in this group, contrary to the findings of Saaby et al.,17 but corroborating those by Collste et al.,28 who also found patients with typical characteristics of Takotsubo in their study.
Coronary spasm may result in ST-segment elevation, although it is often associated with ST-segment depression, indicating subendocardial myocardial ischemia. Coronary vasospasm is associated with several arrhythmias, including sinus bradycardia, total atrioventricular block, paroxysmal atrial fibrillation, ventricular tachycardia, ventricular fibrillation, and extrasystoles.29 The vasospasm may be precipitated by stress, magnesium deficiency, consumption of alcohol, and drugs such as cocaine – conditions found in some of the present study's patients.
The elevation of troponin in patients with normal coronary arteries can occur due to tachyarrhythmias, left ventricular hypertrophy, and coronary vasospasm, being relatively common in patients with sepsis or systemic inflammation.30 It can also occur due to other non-ischemic conditions, such as myocarditis and pericarditis. In patients with HIV, a condition found in two of the patients, T-troponin elevation may occur due to flow-related complications, such as hypercoagulability, endothelial dysfunction, and vasculitis.
The present study observed, at a lower prevalence among the clinical findings, that approximately 10% of patients had suspected myocarditis. Of the 176 patients in the study by Collste et al.,28 7% showed typical signs of myocarditis when submitted to cardiac magnetic resonance assessment.
Regarding the clinical outcomes, Alpert et al.15 described a higher mortality in patients with type-2 AMI when compared to their type-1 group. However, they included several patients with anemia, several types of arrhythmias, acute pulmonary edema, and respiratory failure, i.e., more severe conditions that may have increased mortality in this group of patients. However, De Ferrari et al.31 reported that death or AMI was less frequent among patients without significant obstructive disease (2.2%), in opposition to those with obstructive disease (13.3%) at 30 days of follow-up. This difference was also observed in the present study, although it did not reach statistical significance.
Although there are few studies on type-2 AMI,15 the present authors have observed some discrepancies in these studies, which may be due to the interpretation of classification criteria and the diversity of conditions included in that classification.15,30,31 According to Canty et al.,32 different pathologies can cause imbalance in myocardial oxygen supply and demand. Further studies are needed to assist in the identification and improvement of this classification,8,9,15,29,30 and even to question it, since type-2 AMI is not recognized in the International Classification of Diseases (ICD).8
Study limitationsOne of the limitations was associated to the inclusion of a pre-selected population of patients with STEMI, which favors the occurrence of type-1 AMI and thus, this study may not reflect the true epidemiology of type-2 AMI.
Another limitation lies in the fact that patients with type 2 AMI have not been evaluated by intracoronary vascular ultrasound. This imaging modality, often detect hidden lesions in patients with angiographically “normal” coronary artery disease, and the unavailability of these results may have caused misclassification.
ConclusionsIn this study, few patients with ST-segment elevation myocardial infarction were classified as type-2 infarction; had isolated structural abnormalities or associated with the absence of significant lesions at the coronary angiography; showed few differences in the clinical and laboratory profile, when compared to patients with type-1 myocardial infarction; and had similar clinical outcomes at 30 days.
Funding sourceNone.
Conflicts of interestThe authors declare no conflicts of interest.
Peer Review under the responsability of Sociedade Brasileira de Hemodinâmica e Cardiologia Intervencionista.