We evaluated the safety and efficacy of protamine administration, guided by activated clotting time, for the immediate femoral arterial sheath removal in patients undergoing percutaneous coronary intervention with unfractionated heparin in order to propose an algorithm for clinical practice.
MethodsProspective study with consecutive patients with stable angina or low-to-moderate risk acute coronary syndrome. We compared patients with an early removal of the arterial sheath to those whose sheath removal was based on a standard protocol.
ResultsThe early removal group (n = 149) had lower access manipulation time than the conventional group (58.3 ± 21.4 minutes vs. 355.0 ± 62.9 minutes; p < 0.01), mainly due to a reduced time to sheath removal (42.3 ± 21.1 minutes vs. 338.6 ± 61.5 minutes; p < 0.01), with no impact on the duration of femoral compression (16.0 ± 3.6 minutes vs. 16.4 ± 5.1 minutes; p = 0.49). There was no stent thrombosis during hospitalization and no significant differences in the incidence of major vascular or bleeding events. The incidence of other bleeding events leading to a prolonged in-hospital length of stay was lower in the early removal group (1.3% vs. 5.1%; p = 0.05). Conclusions: The selective use of an approach for immediate femoral sheath removal, based on activated clotting time guidance and protamine administration, is a safe and effective option in patients undergoing percutaneous coronary intervention by femoral access.
Remoção Precoce do Introdutor Arterial Após Intervenção Coronária Percutânea por Via Femoral: Estudo de Segurança e Eficácia
IntroduçãoAvaliamos a seguranga e eficácia do uso depro-tamina, guiada pelo tempo de coagulação ativado, para a remoção imediata do introdutor arterial femoral em pacientes submetidos á intervenção coronária percutaâea com heparina não fracionada, com o objetivo de propor um algoritmo para a prática clínica.
MétodosEstudo prospectivo, com pacientes consecutivos, com angina estável ou com síndrome coronariana aguda de baixo ou moderado risco. Comparamos os pacientes com a retirada precoce do introdutor arterial áqueles nos quais o introdutor foi retirado de acordo como protocolo convencional. A decisão pela remoção precoce ou convencional do introdutor foi deixada a criterio do operador.
ResultadosO grupo de remoção precoce (n = 149) apresentou menor tempo de manuseio do sítio de punção que o grupo de remoção convencional (58,3 ± 21,4 minutos vs. 355 ± 62,9 minutos; p < 0,01), principalmente devido á redução do tempo até a retirada do introdutor (42,3 ± 21,1 minutos vs. 338,6 ± 61,5 minutos; p < 0,01), sem impacto sobre a duração da compressao femoral (16,0 ± 3,6 minutos vs. 16,4 ± 5,1 minutos; p = 0,49). Não houve trombose hospitalar de stent e nem diferenga significativa na incidênciade eventos vasculares ou hemorrágicos. A incidência de outras hemorragias, que levaram á hospitalização prolongada, foi menor no grupo de remoção precoce (1,3% vs. 5,1%; p = 0,05).
ConclusõesO uso seletivo de uma abordagem para a remoção imediata do introdutor femoral guiada pelo tempo de coagulação ativado e a administração de protamina são seguros e eficazes em pacientes submetidos á intervenção coronária percutânea pela via femoral.
The radial approach for percutaneous coronary intervention (PCI) has gained much attention in recent years, due to its potential to reduce the bleeding rates related to the procedure,1 especially in patients with acute coronary syndrome. However, the need for a femoral approach, after the failure of the radial approach, can reach up to 17% in certain subgroups of patients.2 In practice, contraindications or impossibility of the radial access, along with the preference of the doctor and patient, still place the femoral approach as an obligatory technique in the portfolio of any interventional cardiology laboratory, particularly for patients with stable coronary artery disease and low risk of bleeding complications.
Despite the fact that anticoagulation with bivalirudin during PCI has been proven to be beneficial, especially in patients with acute coronary syndrome, unfractionated heparin (UFH) still remains as the main anticoagulant agent among many, if not the majority, of the procedures around the world.3 Previous studies have evaluated the use of protamine after PCI to reverse anticoagulation as a strategy to allow for an early removal of the sheath and potentially to reduce bleeding complications.45 In a meta-analysis with 6,762 patients, protamine significantly reduced bleeding without increasing thrombotic adverse events.4 Conversely, another study comparing bivalirudin with UFH in association with protamine showed better results with the first anticoagulation protocol.5
The present study was conducted with the aim of evaluating the efficacy and safety of a new algorithm for early femoral arterial sheath removal after PCI, compared to the conventional protocol, in patients treated in the daily practice of a laboratory of interventional cardiology with a large volume of procedures.
METHODSStudy design and populationBetween August 2012 and March 2013, 228 consecutive patients with stable angina or moderate- or low-risk acute coronary syndrome undergoing PCI were prospectively included in this study. The decision in favor of early or conventional removal of the sheath was left to the discretion of the surgeon. Patients with early removal of the arterial sheath (Early Removal Group) were compared versus those in which the sheath was removed according to the conventional protocol (Conventional Group) followed by the institution.
The exclusion criteria were: (1) PCI performed by radial approach; (2) use of subcutaneous enoxaparin in the last 12 hours; (3) use of oral anticoagulation; (4) high-risk coronary syndrome (Thrombolysis in Myocardial Infarction [TIMI] > 4);6 (5) presence of an intracoronary thrombus; (6) hemodynamic instability. Bivalirudin was not available in Brazil at the time of inclusion of patients; thus, all procedures were performed with the use of UFH.
At the time of the procedure, all patients were being treated with dual antiplatelet therapy with acetylsalicylic acid (100-300mg daily) and clopidogrel (loading dose 300 to 600 mg, at least 6 hours before the procedure, followed by 75mg daily). During the procedure, UFH was administered at a dose 70-100 IU/kg.
Baseline data, on the procedure and the in-hospital lenght of stay were prospectively collected as part of a dynamic registration approved by the ethics committee of our institution.
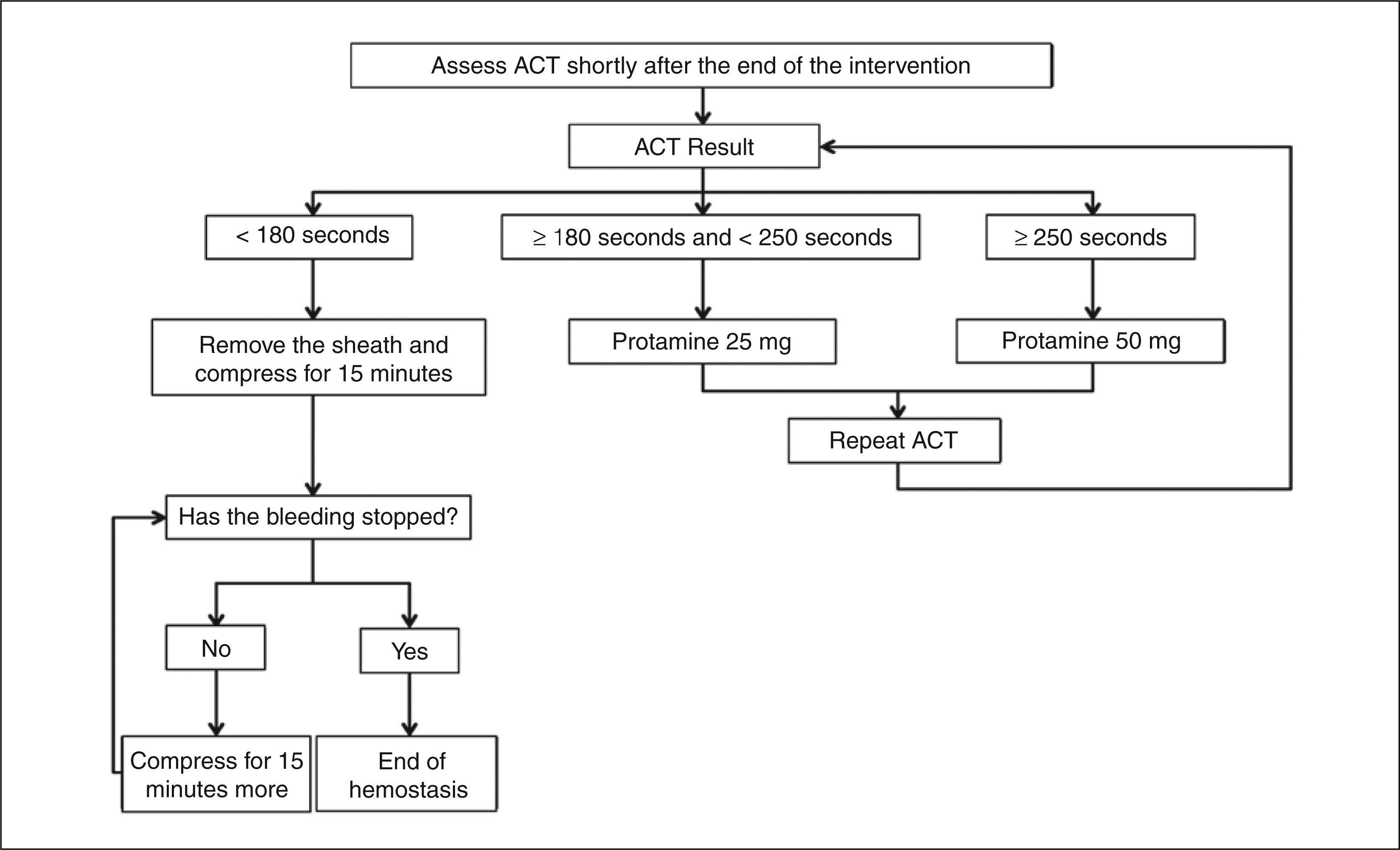
Protocol of early removal of the sheathThe early removal of the arterial sheath was based on an activated clotting time (ACT)-guided algorithm, which included the use of intravenous protamine to neutralize the effect of UFH, when necessary (Figure). Immediately after the procedure, the ACT was measured. The femoral sheath was removed if ACT < 180 seconds. If the ACT was between 180 and 250 seconds, or if > 250 seconds, 25mg or 50mg of protamine (diluted in 100mL of 0.9% saline) was administered intravenously during ten minutes, respectively. Five minutes after administration of protamine, a new ACT-guided cycle was repeated, as described above. An extra dose of protamine was administered, up to a maximum dose of 1mg/100 IU of UFH used in the procedure.
Patients included in the Conventional Group had the sheath removed after 4 to 6 hours of the last dose of UFH, without measurement of ACT.
In both groups, the femoral hemostasis was obtained by manual compression during at least 15 minutes. After removal of the sheath, patients remained on bed rest for 6 more hours.
DefinitionsThe treated lesions were classified according to the American College of Cardiology/American Heart Association (ACC/AHA). Success of the angiographic procedure was defined as the presence of a residual stenos is < 30%, absence of dissection, and final TIMI flow 3.
The primary efficacy endpoint was the total time of handling of the access site, defined as the sum of the time spent for removal of the sheath and the total time of compression. The time spent for removal of the sheath was computed from the end of the procedure until the time at which the sheath was removed.
The primary safety endpoint was composed by cardiovascular and cerebrovascular adverse events (death, myocardial infarction, stroke, and unplanned myocardial revascularization), and by major bleeding and vascular complications, combined during hospitalization. All causes of death were considered in the analysis. After the procedure, the level of CK-MB mass was systematically measured in all patients, and myocardial infarction was classified as: (1) spontaneous; (2) secondary to an imbalance between supply and demand; (3) leading to death, with no available biomarkers; (4) post-PCI; (5) post-coronary artery bypass graft surgery [CABG]; or (6) related to stent thrombosis, according to previously established criteria.7 All unplanned reoperations were considered in the analysis. Stent thrombosis was classified as definite, probable, or possible.8 Major vascular events and bleeding were defined as (1) associated with hemodynamic instability or leading to death; (2) requiring invasive therapeutic intervention and/or blood cell transfusions; (3) leading to prolonged hospitaliza- tion; (4) associated with a drop in hemoglobin level of > 3 g/dL; or (5) intracranial hemorrhage.
Adverse reactions to protamine were classified as occurrence of hypotension, low back pain, broncho-spasm, or skin rash,9 during the procedure or within the first 12 hours after its completion.
Statistical AnalysisCategorical variables and adverse events were presented as absolute numbers and percentages, and compared using the Fisher’s exact test or the chi-squared test. Continuous variables were presented as means and standard deviations and compared using Student’s i-test. All p-values were two-tailed and considered significant if < 0.05.
RESULTSA total of 228 consecutive patients were included in the evaluation during the study period. Two-thirds of patients (n = 149) underwent early removal of the sheath (Early Removal Group) and the others (n = 79) followed the institutional protocol (Conventional Group). The clinical and angiographic characteristics were similar between the two groups, except for a higher dose of heparin and a tendency towards younger patients in the Early Removal Group (Table 1). Approximately one-third of patients were diabetic and most showed stable coronary disease. Only 6 or 7F sheaths were used, and most of the procedures were performed with 6F sheaths. Complex lesions were treated in approximately 70% of patients (types B2 or C).
Clinical, angiographic, and procedural characteristics
| Early removal (n = 149) | Conventional (n = 79) | p-value | |
|---|---|---|---|
| Age, years | 60.6 ± 17.9 | 64.8 ± 11.2 | 0.06 |
| Male, n (%) | 101 (67.8) | 46 (58.2) | 0.19 |
| Weight, kg | 75.9 ± 14.3 | 73.7 ± 15.5 | 0.28 |
| Height, m | 1.66 ± 0.09 | 1.64 ± 0.09 | 0.11 |
| Hypertension, n (%) | 129 (86.6) | 69 (87.3) | >0.99 |
| Previous or current smoking, n (%) | 60 (40.3) | 32 (40.5) | >0.99 |
| Diabetes mellitus, n (%) | 50 (33.6) | 28 (35.4) | 0.77 |
| Previous acute myocardial infarct, n (%) | 46 (30.9) | 21 (26.6) | 0.54 |
| Previous coronary artery bypass graft surgery, n (%) | 24 (16.2) | 12 (15.2) | > 0.99 |
| Previous percutaneous coronary intervention, n (%) | 37 (25.0) | 22 (27.8) | 0.64 |
| Platelets, 103× cells/mL | 244.0 ± 75.5 | 236.0 ± 61.9 | 0.42 |
| Acute coronary syndrome at presentation, n (%) | 25 (16.8) | 9 (11.4) | 0.33 |
| Classification of lesions, n (%) | |||
| Type A | 9 (6.0) | 7 (8.9) | |
| Type B1 | 29 (19.5) | 17 (21.5) | |
| Type B2 | 51 (34.2) | 23 (29.1) | |
| Type C | 60 (40.3) | 32 (40.5) | |
| Number of stents | 1.4 ± 0.7 | 1.6 ± 1.0 | 0.08 |
| Mean stent nominal diameter, mm | 3.1 ± 0.7 | 3.0 ± 0.6 | 0.10 |
| Total length of stents, mm | 28.3 ± 16.7 | 32.5 ± 24.0 | 0.12 |
| Heparin dose, IU | 9.205 ± 1.389 | 8.741 ± 1.391 | 0.02 |
| Sheath diameter, n (%) | 0.88 | ||
| 6F | 108 (72.5) | 56 (70.9) | |
| 7F | 41 (27.5) | 23 (29.1) | |
| Ipsilateral puncture ≤ 7 days, n (%) | 13 (8.8) | 5 (6.3) | 0.61 |
In the Early Removal Group, immediately after the procedure ACT was < 180 seconds in five patients (3.3%), who had the femoral sheath removed without the need of protamine administration. For the others, an initial dose of 25 or 50 mg of protamine was infused in 64 and 80 patients (43.0% and 53.7%, respectively), according to the ACT value. A second dose of protamine was required in 37 patients (24.8%), and only one patient (0.7%) required a third dose. In total, the mean required dose of protamine was 45.8 ± 18.8mg.
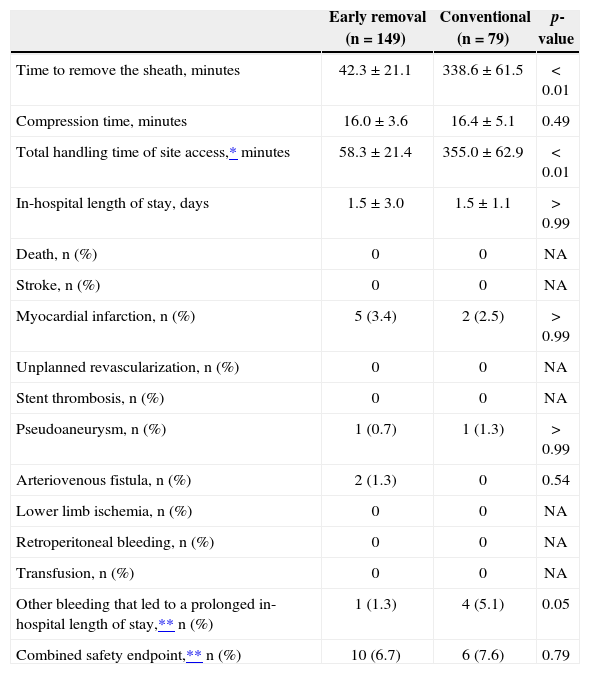
Patients in the Early Removal Group had a time of access manipulation significantly lower than in the Conventional Group (58.3 ± 21.4 minutes vs. 355.0 ± 62.9 minutes, respectively; p < 0.01), mainly due to the reduction in the time until removal of the sheath (42.3 ± 21.1 vs. 338.6 ± 61.5 minutes, respectively; p < 0.01), with no impact on the duration of femoral compression (16.0 ± 3.6 vs. 16.4 ± 5.1 minutes, respectively; p = 0.49) (Table 2).
Access site and in-hospital clinical outcomes
| Early removal (n = 149) | Conventional (n = 79) | p-value | |
|---|---|---|---|
| Time to remove the sheath, minutes | 42.3 ± 21.1 | 338.6 ± 61.5 | <0.01 |
| Compression time, minutes | 16.0 ± 3.6 | 16.4 ± 5.1 | 0.49 |
| Total handling time of site access,* minutes | 58.3 ± 21.4 | 355.0 ± 62.9 | <0.01 |
| In-hospital length of stay, days | 1.5 ± 3.0 | 1.5 ± 1.1 | >0.99 |
| Death, n (%) | 0 | 0 | NA |
| Stroke, n (%) | 0 | 0 | NA |
| Myocardial infarction, n (%) | 5 (3.4) | 2 (2.5) | >0.99 |
| Unplanned revascularization, n (%) | 0 | 0 | NA |
| Stent thrombosis, n (%) | 0 | 0 | NA |
| Pseudoaneurysm, n (%) | 1 (0.7) | 1 (1.3) | >0.99 |
| Arteriovenous fistula, n (%) | 2 (1.3) | 0 | 0.54 |
| Lower limb ischemia, n (%) | 0 | 0 | NA |
| Retroperitoneal bleeding, n (%) | 0 | 0 | NA |
| Transfusion, n (%) | 0 | 0 | NA |
| Other bleeding that led to a prolonged in-hospital length of stay,** n (%) | 1 (1.3) | 4 (5.1) | 0.05 |
| Combined safety endpoint,** n (%) | 10 (6.7) | 6 (7.6) | 0.79 |
NA: not applicable.
There were no adverse cardiac or cerebrovascular events during hospitalization, except for a minority of patients who had periprocedural myocardial infarction (3.4% vs. 2.5%; p > 0.99). The incidence of major vascular events and of bleeding was not different between the two groups (3.3% vs. 6.4% respectively; p = 0.32), as well as the incidence of a combined safety endpoint, which was also similar among groups (6.7% vs. 7.6% respectively; p = 0.79). The incidence of other bleeding that led to a prolonged hospitalization was lower in the Early Removal Group (1.3% vs. 5.1%; p = 0.05).
Only one patient presented an adverse effect related to the administration of protamine, which consisted of low back pain, quickly resolved with hydration and analgesia.
DISCUSSIONThe main result of the present study was that the selective use of a stepwise approach for the immediate removal of the femoral arterial sheath, based on an ACT value and followed by the use of protamine to antagonize heparin, is safe and effective in reducing the manipulation time of the access route in patients undergoing PCI.
Previous studies have examined the use of protamine after PCI through femoral route.4,5 In these studies, however, protamine was only indistinctly prescribed after the procedure, without individualization of its use, as proposed in this study. Indeed, the present study centered the strategy for early removal of the sheath upon the reversal of anticoagulation, rather than only a simplistic strategy of a separate administration of protamine. As seen in these patients, when sheath removal was guided by an ACT value, there were patients who did not require the use of protamine; others require halfdose, full dose, or even repeating the dose of protamine to obtain an early, safe, and effective removal of the sheath after PCI via the femoral artery.
Intuitively, the immediate reversal of heparin effect after implantation of a coronary stent may increase the chances of a hyperacute stent thrombosis. In the present series, there were no cases of thrombotic complication after protamine administration. It is important to emphasize that, in this study, only patients who already were treated with dual antiplatelet therapy, who had a stable pre- and post-procedure clinical condition, and whose result of the intervention was considered satisfactory were included. Thus, these findings cannot be extrapolated to other clinical settings.
A relatively large list of potent antithrombotic agents is currently available for use in patients treated with PCI. However, an aggressive antithrombotic therapy proves more beneficial in patients with acute coronary syndrome, with less evidence supporting its routine use in stable patients.3,10 Similarly, PCI by radial approach has been shown to reduce adverse events in acute pa- tients,11 with few studies showing benefit in those with stable coronary disease. Thus, PCI through femoral access with the use of UFH for the treatment of patients with stable coronary artery disease still remains the primary strategy in a large number of countries and institutions. In this context, the present study prospectively evaluated the use of protamine to obtain an early removal of the femoral sheath in a population of patients with stable coronary disease, or with acute coronary syndrome of low or moderate risk.
The present study had intrinsic limitations, due to the fact that it was not randomized, and also due to its sample size. Although the incidence of adverse events was similar between both groups, the possibility that significant differences in complications of low incidence could arise, if the sample size was increased, cannot be ruled out. However, due to the minimal absolute and relative differences in the observed outcomes between both groups, it is unlikely that these results would be substantially changed, if the sample was increased. The patients included in this study were not randomly assigned. Thus, the influence of a selection bias in the results cannot be completely ruled out. However, this study was intended primarily to evaluate the clinical performance of the proposed algorithm in a daily clinical practice, according to which the strategy of an early removal can be used selectively, by analyzing each case. Finally, the administration of protamine may be associated with side effects. The approach described in our study tends to minimize the unwanted effects of protamine, reducing the final dose to the minimum needed to neutralize the effect of UFH. In fact, the protamine dose used in this study was less than half the theoretically recommended dose to neutralize the total dose of UFH administered during the procedure.
CONCLUSIONSThe selective use of an approach for immediate removal of the femoral arterial sheath, guided by the value of activated coagulation time and followed by the administration of protamine, is a safe and effective option in patients with stable coronary artery disease undergoing percutaneous coronary intervention by femoral access.
ACKNOWLEDGMENTSThe authors thank Mrs. Patricia Pereira, Paula Fields, and Irineia Aleixo, for their invaluable support.
CONFLICTS OF INTERESTThe authors declare no conflicts of interest.
FUNDING SOURCENone.
Instituto do Coração, Universidade de São Paulo, São Paulo, SP, Brazil.