Endovascular treatment has revolutionized the therapeutic approach to abdominal aortic aneurysms due to its low morbidity and mortality rates. Despite the technological advances, there still are anatomical limitations on the use of stent grafts. This study aimed to evaluate the immediate clinical results in patients with complex abdominal aortic aneurysms treated with a second generation stent graft.
METHODSThis is an observational, prospective, non-randomized, single-center study in a series of patients undergoing endovascular repair of complex infra-renal abdominal aortic aneurysms, using a stent graft with a dual-ring stent design (Anaconda™ – Vascutek, Terumo, Inchinnan, Scotland). Clinical and angiographic characteristics, technical and therapeutic success rates, morbidity and mortality and perioperative reintervention rates were evaluated.
RESULTSBetween February 2010 and December 2011, 108 consecutive patients with aortic aneurysms were treated, of whom 16 had complex abdominal aortic aneurysms, treated with the Anaconda™ AAA Stent Graft System. Mean age was 76±7 years and 75% were males. Technical success was observed in 94% and therapeutic success in 75% of cases. There was one postoperative death. The most prevalent perioperative complication was surgical wound bleeding (2/16) and peripheral embolism (2/16). Reinterventions were required in 12.5% of the patients during follow-up.
CONCLUSIONSIn this study, the second-generation Anaconda™ Stent Graft System was effective and provided satisfactory immediate results in the treatment of complex infra-renal abdominal aortic aneurysms.
Tratamento Endovascular dos Aneurismas da Aorta Abdominal com Anatomia Complexa:Resultados Preliminares com a Segunda Geração de Endoprótese com Arcabouço Metálico Circular
IntroduçãoO tratamento endovascular dos aneurismas da aorta abdominal tem revolucionado o tratamento dessa afecção, em decorrência das baixas taxas de morbidade e mortalidade. Apesar dos avanços tecnológicos ocorridos nas endopróteses, ainda existem limitações anatômicas para o emprego da técnica. Este estudo teve por objetivo avaliar os resultados imediatos do tratamento de pacientes portadores de aneurisma da aorta abdominal com anatomia complexa com uma endoprótese de segunda geração.
MétodosEstudo observacional, prospectivo, não randomizado, realizado em um único centro, em uma série de pacientes submetidos a tratamento endovascular de aneurismas da aorta abdominal infrarrenais complexos, com prótese com arcabouço metálico disposta em anéis (Anaconda™ – Vascutek, Terumo, Inchinnan, Escócia). Foram avaliados as características clínicas e angiográficas, o sucesso técnico, o sucesso terapêutico, a morbidade e a mortalidade, e a taxa de reintervenção perioperatória.
ResultadosForam analisados, no período de fevereiro de 2010 a dezembro de 2011, 108 pacientes consecutivos portadores de aneurisma da aorta, dos quais 16 eram portadores de aneurisma da aorta abdominal com anatomia complexa tratados com a prótese Anaconda™. A média de idade foi de 76 ± 7 anos e 75% eram do sexo masculino. Houve sucesso técnico em 94% e êxito terapêutico em 75% dos casos. Ocorreu um óbito no pós-operatório. As complicações perioperatórias mais prevalentes foram sangramento da ferida operatória (2/16) e embolia periférica (2/16). Foram necessárias reintervenções em 12,5% dos pacientes durante o seguimento.
ConclusõesNeste estudo, a segunda geração da endoprótese Anaconda™ foi efetiva e apresenta resultados imediatos satisfatórios no tratamento do aneurisma da aorta abdominal infrarrenal de anatomia complexa.
For many years, surgical treatment has been the standard therapy for patients with abdominal aortic aneurysm.1 Since the introduction of the endovascular repair technique by Parodi et al.2 in 1991, which aimed to decrease intra- and postoperative morbidity and mortality, the materials used for this treatment have been constantly improved. These improvements have led to better medium and long-term results.3
Endovascular repair is preferably indicated for high-risk surgical patients due to clinical comorbidities or for those patients with anatomic difficulties for an open surgical approach (hostile abdomen). Despite aggressive technological development, the ideal endograft has not yet been designed, and there are still technical limitations regarding the percutaneous procedure due to local anatomic variation, which hinders the adequate exclusion of the aneurysm.
Three major studies (Comparison of EndoVascular Aneurysm Repair open repair in patients with abdominal aortic aneurysm – EVAR 1, Endovascular Aneurysm Repair and outcome in patients unfit for open repair of abdominal aortic aneurysm – EVAR 2, and Dutch Randomized Endovascular Aneurysm Management – DREAM)4–6 have shown that perioperative morbidity and mortality rates (within 30 days after the procedure) were favourable for endovascular treatment; however, when mortality rates were compared with that of the surgical technique, they were similar after one year of aneurysm treatment. The reintervention rates were greater in the endovascular treatment group and varied from 14% to 26%. This fact motivated the development of more versatile and flexible endografts, which would better adapt to existing anatomic obstacles in the aneurysm neck and aortoiliac bifurcation, as well as promote better sealing of its connections. A better seal would help prevent undesired endoleaks and decrease reintervention rates.
The aim of this study was to conduct an analysis of the perioperative results achieved through the use of a second-generation stent graft with a dual-ring stent design (Anaconda™, Vascutek – Terumo, Inchinnan, Scotland) in the treatment of complex infra-renal abdominal aortic aneurysms.
METHODSThis was an observational, prospective, non-randomized study conducted at a cardiovascular disease centre in the state of São Paulo between February of 2010 and December of 2011. During the study period, 108 consecutive patients with aortic aneurysms were percutaneously treated with the Anaconda™ second-generation stent graft; 16 patients had complex infra-renal abdominal aortic aneurysms.
Inclusion and exclusion criteriaPatients with abdominal aortic aneurysm and indication for elective repair using the diameter criterion (> 55mm in men and > 50mm in women) or due to the presence of symptoms were included in the study. The anatomical criteria for using the stent graft were the presence of angulation in the proximal aortic neck (defined as the angle between the greater axis of the aneurysm neck and the greater axis of the aneurysm) and/or aortoiliac bifurcation of > 60 degrees. The study excluded patients presenting with a proximal neck < 15mm, thrombus, calcification > 50% of the neck circumference, diameter of external iliac arteries < 7mm, serum creatinine > 2mg/dL, or creatinine clearance < 30mL/min.
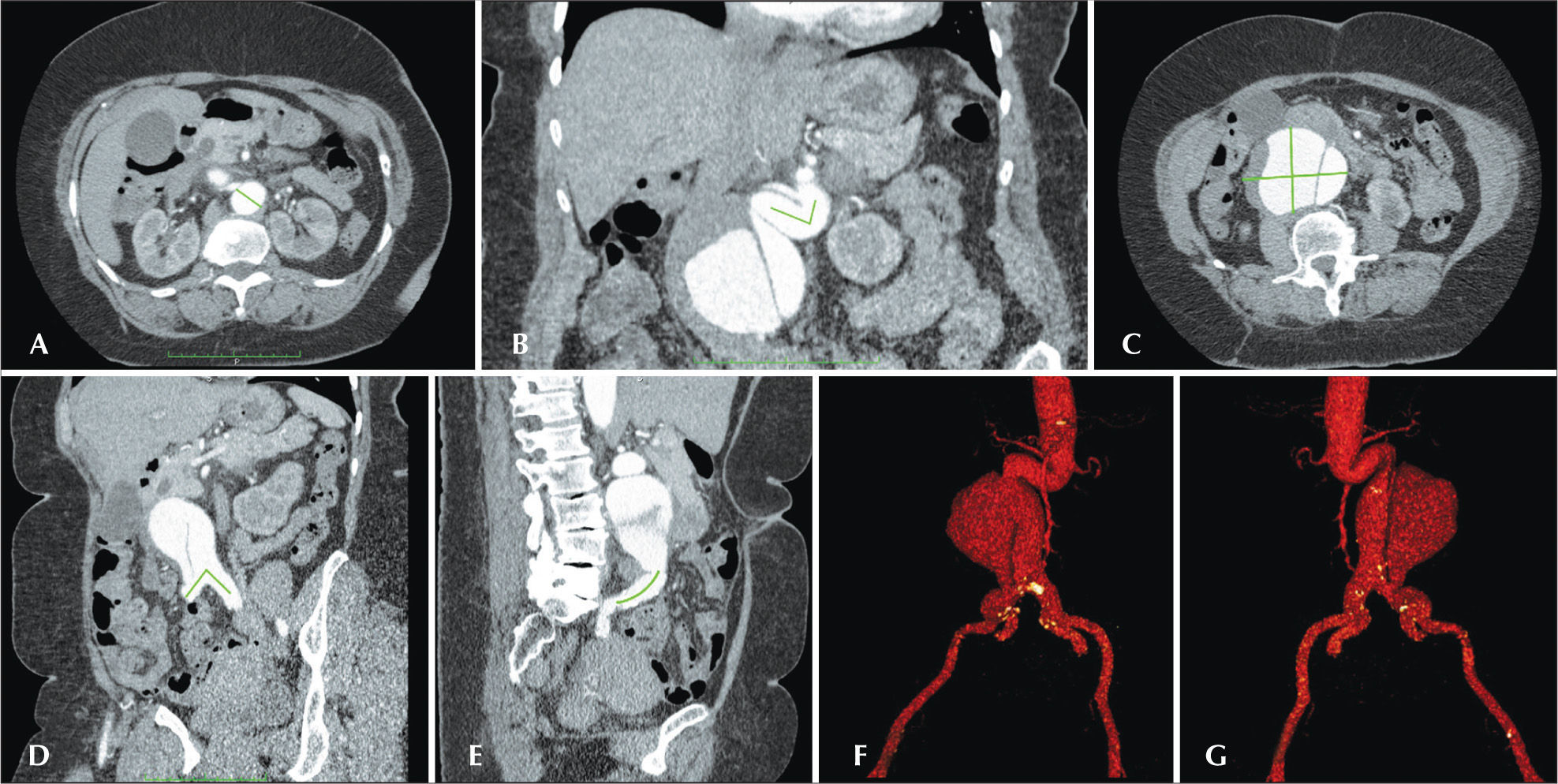
Techniques usedThe diagnosis and treatment of abdominal aortic aneurysm were based on angio-tomography, employing a 64-channel multi-slice computed tomography scan with 1mm slices in all cases. Preoperative arteriography was an optional diagnostic method. All computed tomography scans were reproduced using OSIRIX® software in 3D and multi-planar reconstruction (MPR) modes. Therefore, it was possible to obtain the diameters, angles, and lengths of the proximal aortic neck, aneurysm, and aortoiliac bifurcation (Figure 1).
– Angio-tomography showing a three-dimensional multi-planar reconstruction of a complex aortic aneurysm. A shows a 30-mm diameter aortic neck. B shows the neck angle (71 degrees). C shows the greatest diameter of the aneurysm (75mm). D shows the angle of the aortoiliac bifurcation (82 degrees). E shows the length of the right common iliac artery (46mm). F shows a three-dimensional reconstruction (anterior view). G shows a three-dimensional reconstruction (posterior view).
Anaconda™ is a tri-modular stent graft consisting of a nitinol dual-ring design and coated with woven Dacron. The proximal part of the graft body consists of two nitinol rings that provide radial strength for passive sealing of the proximal neck. Active fixation is provided by four pairs of hooks (two anterior pairs and two lateral pairs), which are not required for suprarenal or juxta-renal fixation. The stent graft diameter must be 10% to 20% greater than the internal diameter of the proximal aortic neck. The main body is connected to a system of nitinol rings, which make it possible for the stent graft to be collapsed and repositioned. The iliac leg consists of a woven Dacron® prosthesis with a series of nitinol rings whose distance varies according to its diameter. The contralateral iliac leg is connected through catheterization and is facilitated by a magnetic guide wire connected to the body of the stent graft. Dilation with a compliant balloon during the operation is only recommended in the case of an initial endoleak, and should not be frequently performed.
All procedures were performed in a haemodynamic monitoring laboratory. Patients were treated under general inhalation anaesthetics. Antimicrobial prophylaxis was administered with 1.5g of cefuroxime at the moment of anaesthesia induction. The preferred approach was by the bilateral common femoral artery through open surgical dissection. When this approach was not possible, the external iliac artery was accessed via a retroperitoneal approach.
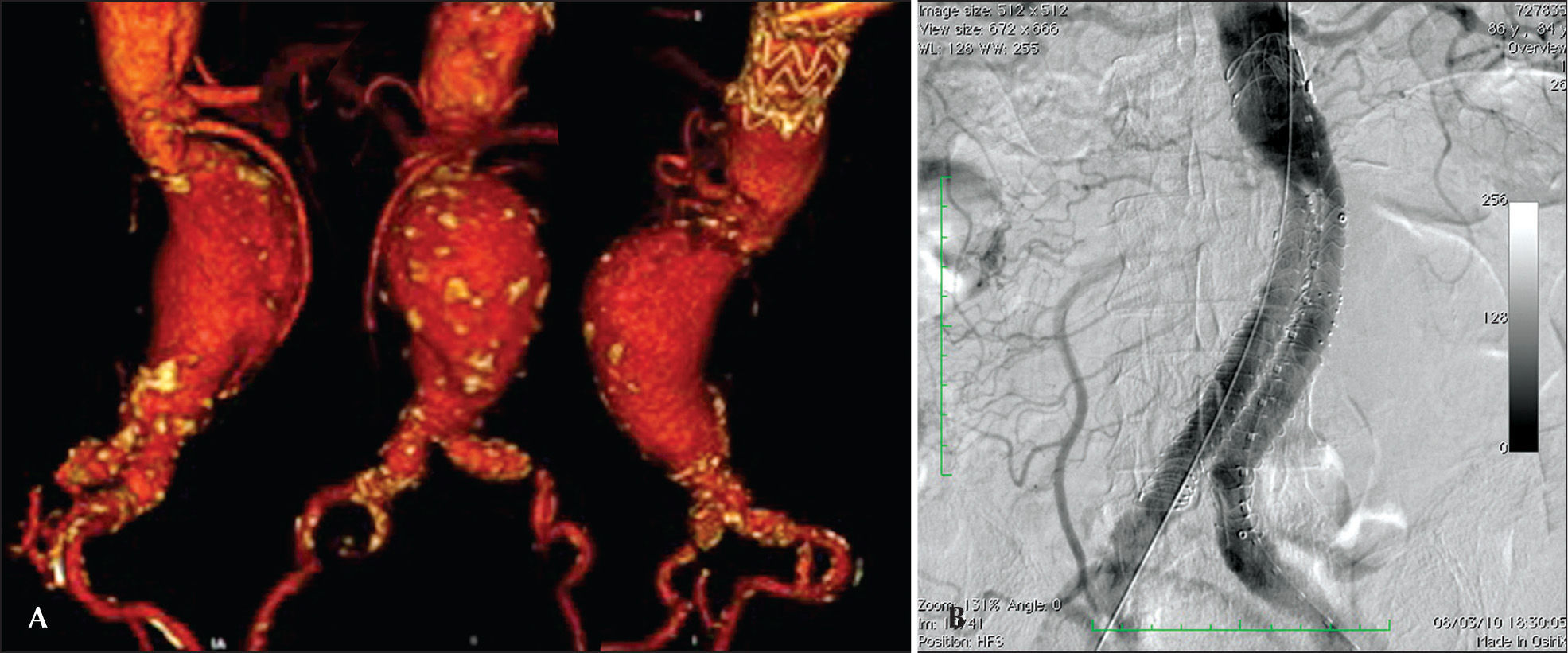
Radiographic control was performed with the Artis® Flat Panel detector (Siemens, Munich, Germany). When the location of the device was not considered satisfactory during the positioning of the proximal neck, the device was repositioned in the craniocaudal direction or according to its longitudinal axis. When the first stage was finished, the contralateral iliac leg was introduced after magnetic catheterization of the stent body and then released. When the second stage was finished, the catheterization of the ipsilateral leg was performed, which was finally released and fixed to the stent body. Intraoperative arteriography was performed in all patients (Figure 2). All patients were transferred to the intensive care unit immediately after the procedure.
Outpatient follow-up occurred 15 and 30 days after the procedure. Angio-tomography was performed on the 30th day of outpatient follow-up. Colour-Doppler ultrasound was performed when angio-tomography was contraindicated.
DefinitionsComplex infra-renal abdominal aortic aneurysms present with a proximal aortic neck and/or aortoiliac bifurcation > 60 degrees. Initial or primary endoleaks were defined as those occurring during the initial procedure or those diagnosed within the first 30 days.
Technical success was achieved with the release of the stent graft in the affected area, regardless of the presence of endoleaks or other incidents that could negatively influence the outcome. Therapeutic success was achieved when the release of the stent graft occurred without endoleaks or other incidents that could influence clinical outcomes of the patients.
Peri-procedural complications were classified as intraoperative complications when they occurred during the intervention procedure in the haemodynamic monitoring room, and were classified as perioperative complications when they occurred during the hospital stay, outside the hemodynamic monitoring room, and within 30 days after intervention. The following were considered complications: local bleeding (presence of inguinal or retroperitoneal haematoma); uni- or bilateral occlusion of the renal arteries; presence of peripheral embolization causing acute arterial occlusion; presence of mesenteric ischemia causing vascular acute abdomen; infections (whether surgical site infections or lower respiratory tract infections); acute renal failure (> two times the increase in the basal creatinine before the procedure); occlusion of the stent graft due to thrombosis; and death.
Reintervention was defined as an intervention performed to maintain the appropriate function of the stent graft and exclude the aneurysm sac, or to resolve complications related to the initial intervention.
In-hospital lenght of stay was defined as the time period between hospital admission and discharge. Procedure time was defined as the period between the beginning of anaesthesia induction and the closure of the operative surgical site.
RESULTSAll patients were asymptomatic, and were electively treated. The average duration of the procedure was 112 minutes (varying from 76 minutes to 155 minutes), and the average in-hospital length of stay period was 4.2days (minimum: three days; maximum: 14 days).
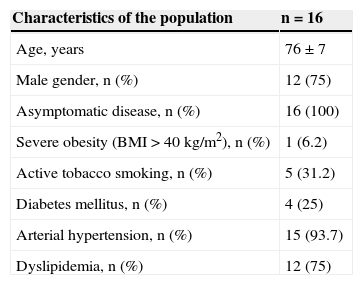
Sixteen patients who underwent a complex infrarenal abdominal aortic aneurysm repair were analysed. The mean age was 76±7 years, and 75% of the patients were male (Table 1). Among the co-morbidities, the incidence of coronary artery disease was 43.7%, chronic obstructive pulmonary disease was 37.5%, and chronic renal failure was 18.7%. Half of the population were ASA surgery risk≥3 (according to the criteria of the American Society of Anesthesiology).
Clinical Data
| Characteristics of the population | n=16 |
|---|---|
| Age, years | 76±7 |
| Male gender, n (%) | 12 (75) |
| Asymptomatic disease, n (%) | 16 (100) |
| Severe obesity (BMI>40kg/m2), n (%) | 1 (6.2) |
| Active tobacco smoking, n (%) | 5 (31.2) |
| Diabetes mellitus, n (%) | 4 (25) |
| Arterial hypertension, n (%) | 15 (93.7) |
| Dyslipidemia, n (%) | 12 (75) |
BMI=body mass index; n=number of patients.
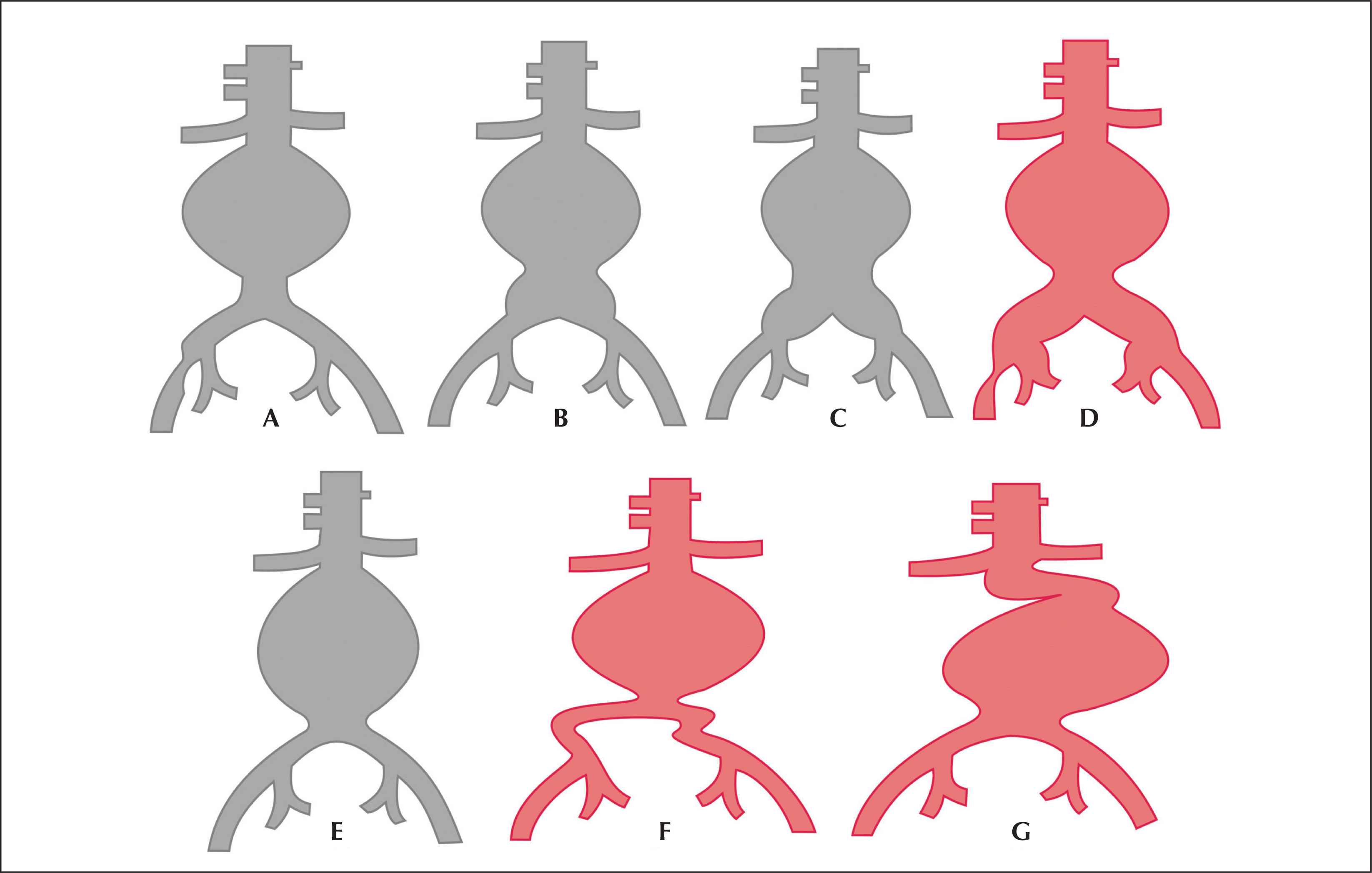
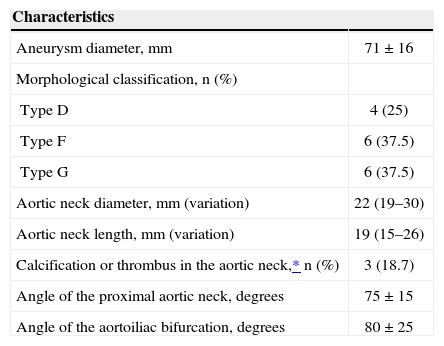
In all cases, aneurysm morphology was fusiform. The types of aneurysm treated according to the classification used by the European Collaborators on Stent/graft Techniques for Aortic Aneurysm Repair (EUROSTAR)7 (Figure 3) were: type D in four patients (25%), type F in six patients (37.5%) and type G in six patients (37.5%). Table 2 shows the average diameter of the aneurysm and the characteristics of the proximal neck and the aortoiliac bifurcation.
– Classification of abdominal aortic aneurysms – EUROSTAR.
Angiographic Characteristics
| Characteristics | |
|---|---|
| Aneurysm diameter, mm | 71±16 |
| Morphological classification, n (%) | |
| Type D | 4 (25) |
| Type F | 6 (37.5) |
| Type G | 6 (37.5) |
| Aortic neck diameter, mm (variation) | 22 (19–30) |
| Aortic neck length, mm (variation) | 19 (15–26) |
| Calcification or thrombus in the aortic neck,* n (%) | 3 (18.7) |
| Angle of the proximal aortic neck, degrees | 75±15 |
| Angle of the aortoiliac bifurcation, degrees | 80±25 |
n=number of patients.
The tri-modular pattern of the stent graft was used in all cases. It was necessary to use unilateral extensions in five (31.2%) of the patients and bilateral extensions in four (25%) of the patients. Stent graft repositioning was performed in three cases (18.6%).
Technical success was achieved in 94%; it was possible to release the stent graft at the desired site in 15 patients. In one case it was necessary to convert to an open surgical approach. Therapeutic success was observed in 75% of the cases; in 12 patients the stent graft was released without an endoleak or other incidents that could negatively influence the outcome.
In three cases (18.7%), it was necessary to embolize the hypogastric artery during the procedure in order to anchor the iliac leg of the stent graft or its extension in the ipsilateral external iliac artery. There were no cases of pelvic or intestinal ischemia, erectile dysfunction, or buttock claudication at follow-up.
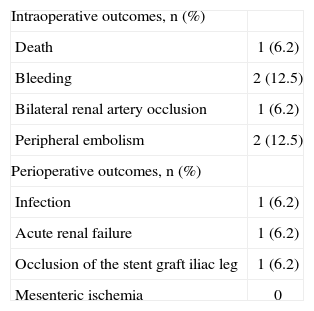
The complication rate was 31.2%, and the most frequent intraoperative complications were operative site bleeding in two cases (12.5%), peripheral embolism in two cases (12.5%), and occlusion of the bilateral renal arteries in one case (6.2%), which required conversion to open surgery. Perioperative infection occurred in one case (6.2%). This was an operative site infection that was treated with the use of systemic antibiotics without clinical repercussions for the patient (Table 3). Perioperative mortality was 6.2%. Despite conversion to an open surgery, one patient died because the bilateral renal arteries were occluded due to stent body migration during the operation.
Intra and Perioperative Complications
| Intraoperative outcomes, n (%) | |
| Death | 1 (6.2) |
| Bleeding | 2 (12.5) |
| Bilateral renal artery occlusion | 1 (6.2) |
| Peripheral embolism | 2 (12.5) |
| Perioperative outcomes, n (%) | |
| Infection | 1 (6.2) |
| Acute renal failure | 1 (6.2) |
| Occlusion of the stent graft iliac leg | 1 (6.2) |
| Mesenteric ischemia | 0 |
n=number of patients.
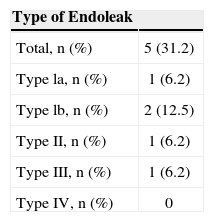
The total endoleak rate was 31.2%, and type I and II endoleaks were present in 25% (Table 4). The perioperative reintervention rate was 12.5% due to the treatment of 2 type Ib endoleaks. One patient with a type Ia endoleak was treated during the operation by insufflating the compliant balloon in the proximal neck, which led to resolution of the endoleak. A type III endoleak, which is caused by inappropriate sealing of the anchoring zone of the iliac legs, was treated in the same way. A type II endoleak, with branches filling the aneurysm sac, was observed in one case on postoperative angio-tomography. Additional interventions due to an increase in the size of the aneurysm sac were not necessary. Two reinterventions to treat a type Ib endoleak and the endoleak of the stent graft iliac leg were necessary; iliac leg extensions were used after surgery.
DISCUSSIONEndovascular treatment of abdominal aortic aneurysms is a less invasive alternative compared to open surgery, and it is indicated for high-risk patients and for those with appropriate anatomy.8 Open surgery is associated with a mortality rate of 2% to 6%. A mortality rate of 2% is associated with low-risk cases, but the mortality can be as high as 50% in cases of ruptured aneurysms.9 According to several publications, technological innovations and the experience gained with the use of endovascular techniques over the last 20 years have reduced the mortality rate and have led to results that are similar to or even better than those observed with traditional surgical treatment.4–6,10–13
Not all patients can undergo endovascular treatment, and unfavourable anatomy is the main limitation to using this technique. These limitations must be evaluated individually, taking into account the team’s experience, the characteristics observed on computed tomography, and the stent graft used. The most important anatomic features that determine endovascular treatment are the tortuosity of the aorta and the diameter, the length of the proximal neck (fixation area for the stent graft), and the access to the iliac-femoral segment. Secondary factors include angulation of the aorta (proximal neck) and iliac arteries, calcification, and the presence of mural thrombus in the proximal neck.14
Nowadays, endovascular treatment of abdominal aortic aneurysms with infra-renal fixation devices is recommended for aortas with an anchorage zone > 15mm, a landing neck diameter < 32mm, and an aortic neck angulation < 60 degrees.8 Stent grafts with suprarenal fixation have been indicated to provide better sealing to the proximal neck when its morphology is unfavourable due to the short length of the landing neck, severe angulation, extensive calcification, and mural thrombus. Despite the advantages of using stent grafts with suprarenal fixation for complex abdominal aortic aneurysms, it is still necessary to wait for long-term follow-up in order to document the incidence of embolization or renal occlusion.8,15
The Anaconda™ stent graft is a device that uses infra-renal fixation and consists of a ring design that provides more flexibility and radial strength to adapt to landing necks with unfavourable anatomy. The easy manoeuvring of the delivery system and the hydrophilic coating facilitate navigation through tortuous iliac vessels. The repositionable deployment system enables position correction in the aortic neck. The catheterization system with the contralateral leg facilitates the procedure in patients with pronounced aortoiliac angulations. These features make the stent graft more attractive for the treatment of more complex infra-renal abdominal aortic aneurysms.
In a comparative study using aortic stent grafts in humans aimed at evaluating iliac and aortic fixation, Melas et al.16 verified the improved proximal fixation with the Anaconda™ stent graft versus six other stents from different manufacturers. The improved proximal fixation is due to the presence of four pairs of hooks and the nitinol coating, which provides greater radial strength and an improved proximal seal.
The present study analysed 108 consecutive patients; 16 had complex abdominal aortic aneurysms. Despite anatomic difficulties, technical success was achieved in 94.1% of the cases. In one patient it was not possible to position and release the stent graft at the appropriate site, and surgical conversion was necessary. In this case, the degree of aortic tortuosity and calcification of the access arteries were underestimated. The literature reports a technical success rate of 94%–99%.13,17 In the EUROSTAR registry7 it was not possible to advance the delivery system of the stent graft in 0.8% of the cases. Brazilian authors have published a study with 105 patients with abdominal aortic aneurysm undergoing endovascular repair, with a technical success rate of 97.2%.18
In a study published by Perdikides et al.19 in 2009, the stent graft with a dual-ring design was used in 20 patients with a complex abdominal aortic aneurysm and the technical success rate was 95%. The mean angulation of the aneurysms of these patients was 62 degrees, the length of the proximal neck ranged from 18mm to 30mm, and the average angulation of the aortoiliac bifurcation was 59 degrees.
The initial technical success rate of the present study was 75%, which was calculated based on the incidence of endoleaks in the primary procedures. In the EUROSTAR registry,7 the incidence of an initial endoleak was 4.4% in type I, 9% in type II, and 2.4% in type III. In the population of this study, an initial endoleak was observed in 31.2% of the cases: 6.2% were type Ia (1 case), 12.5% (2 cases) were type Ib, 6.2% (1 case) were type II, and 6.2% (1 case) were type III endoleaks. Analysing these statistics, four cases (25%) of type I and III endoleaks were observed. Of these, types Ia and III were resolved during the procedure by insufflating the balloon in the proximal neck in the case of the type Ia endoleak and by using the same technique in the iliac leg connection in the case of the type III endoleak. These endoleaks were considered primary endoleaks in this study, since post-dilation with a compliant balloon was not recommended during the initial procedure and was only performed in the case of an endoleak during the aneurysm repair. Angio-tomography performed one month after the procedure confirmed that there was no endoleak in these cases. The remaining two cases of type Ib endoleak were successfully treated with an extension of the iliac leg during the postoperative period, leading to a reintervention rate of 12.5%.
In a study performed by Freyrie et al.,3 49 patients with abdominal aortic aneurysm were treated with the Anaconda™ stent graft. They reported a technical success rate of 100%, with no incidence of type I or II endoleak; 25% had a type II endoleak. In that study, most of the aneurysms had an aortic neck > 20mm and a neck angle < 40 degrees. Other studies using the same stent graft showed a primary endoleak incidence rate of 10%, and a type I and II endoleak rate between 4.8% and 7.7%. All endoleaks showed favourable aortic anatomy.20
In the present study, the mortality rate within 30 days of the procedure was 6.2%. A patient died during conversion to an open surgery due to occlusion of the renal arteries provoked by stent body migration during the procedure. In a Brazilian study, Palma et al.18 reported a mortality rate of 5.6% for patients who had an initial endovascular treatment for an abdominal aortic aneurysm.
The EVAR 1 study4 showed a 4.7% decrease in the perioperative mortality rate for open surgery versus 1.7% for endovascular treatment, a relative risk reduction of 65%. The EUROSTAR registry7 presented a 30-day mortality rate of 1.7% for minimally invasive treatment, while the DREAM trial13 showed a perioperative mortality rate of 4.6% for open surgery and 1.2% for endovascular treatment. Brazilian authors showed a less significant decrease in the perioperative mortality rate of 6.5% and 5.5% for conventional and endovascular treatment, respectively.21,22
According to May and White,23 approximately 20% of the patients treated with an endovascular procedure develop intraoperative complications. Some of them are inversely proportional to the length of the aneurysm neck, that is, the smaller the aneurysm neck, the harder it is to position the endovascular device. At the same time, the greater the number of comorbidities, the greater the risk of intra- and postoperative complications. The DREAM study,13 which compared operative mortality and complications after surgical treatment and endovascular treatment, concluded that endovascular treatment is more appropriate due to the lower mortality rate, the type of complications, and due to the significant reduction in systemic complications. The complication rate was 35% in the EVAR 1 study and 33% in the EVAR 2 study.4,6
In this study, the total complication rate was 31.2% within 30 days after the procedure. Intraoperative bleeding at the surgical site occurred in two cases (two in the inguinal region, in which surgical intervention was not necessary) and peripheral embolization occurred in two cases (one case treated with embolectomy during surgery and the other case, a microembolism, treated with conservative management). These were the most frequent complications. Occlusion of an iliac leg was also observed. This was due to the presence of a calcified plaque close to the iliac extension, which led to thrombosis seven days after the surgery. The occlusion was successfully treated with a crossover femoro-femoral graft.
Limitations of the studyThe limitations of this study were the small sample size and the short follow-up, which limited the conclusions and the possibility of comparing the results with more comprehensive studies.
CONCLUSIONSIn this study, the second-generation stent graft with a dual-ring design was effective in the treatment of complex infra-renal abdominal aortic aneurysms. Studies with a greater number of patients and with medium-and long-term follow-up may define its applicability.
CONFLICTS OF INTERESTThe authors declare no conflicts of interest.