Studies demonstrate that radial artery access reduces the risk of vascular and bleeding complications associated to percutaneous coronary intervention. Our objective was to evaluate in-hospital results of the transradial approach in elderly patients undergoing percutaneous coronary intervention.
MethodsProspective registry including patient’s≥70 years of age; safety and efficacy endpoints were compared for the radial and femoral artery access groups.
ResultsWe included 255 patients, 117 (52%) treated using the radial approach and 108 using the femoral approach. Except for age, the remaining clinical characteristics did not show differences between groups. Male patients prevailed (60%), 36.7% were diabetic and over one third were diagnosed with acute coronary syndrome. Angiographic and procedure-related variables did not show differences between groups. When vascular complication rates were compared only hematomas<5cm (5.1% vs. 17.6%; p<0.01) were more prevalent with the femoral access. Major bleedings, according to the ACUITY criteria (zero vs. 5.6%; p=0.01) and minor bleedings, according to the TIMI criteria (zero vs. 7.4%; p<0.01), were also more frequent in the femoral group. In-hospital clinical endpoints, death (0.9% vs. 5.6%; p=0.06) and non-fatal infarction (zero vs. 3.7%; p=0.05) were more frequent in patients treated by the femoral access.
ConclusionsIn a non-selected patient population≥70 years of age, percutaneous coronary intervention by radial access was associated to a lower incidence of in-hospital clinical endpoints, especially of bleeding events related to the vascular access route.
RESUMOAcesso Radial vs. Acesso Femoral em Pacientes com Idade Avançada Submetidos à Intervenção Coronária Percutânea
IntroduçãoEstudos demonstram que o acesso via artéria radial diminui o risco de complicações vasculares e hemorrágicas associadas à intervenção coronária percutânea. Nosso objetivo foi avaliar os resultados hospitalares da utilização da via radial em pacientes idosos submetidos à intervenção coronária percutânea.
MétodosRegistro prospectivo, que incluiu pacientes≥70 anos, tendo sido comparados os desfechos de segurança e de eficácia entre os grupos tratados pelas vias radial e femoral.
ResultadosIncluímos 225 pacientes, sendo 117 (52%) tratados por via radial e 108 por via femoral. À exceção da idade, as demais características clínicas não mostraram diferençãs entre os grupos. Predominaram os pacientes do sexo masculino (60%); 36,7% eram diabéticos e mais de um terço foi tratado na vigência de quadro de síndrome coronària aguda. As variáveis angiográficas e do procedimento não mostraram diferenças entre os grupos. Na comparação das taxas de complicaçães vasculares, somente os hematomas<5cm (5,1% vs. 17,6%; p<0,01) foram mais prevalentes no acesso femoral. Sangramentos maiores, pelo critèrio ACUITY (zero vs. 5,6%; p=0,01), e menores, pelo critèrio TIMI (zero vs. 7,4%; p<0,01), também foram mais frequentes no grupo femoral. Os desfechos clínicos hospitalares óbito (0,9% vs. 5,6%; p=0,06) e infarto não fatal (zero vs. 3,7%; p=0,05) incidiram mais frequentemente nos pacientes tratados por via femoral.
ConclusõesEm uma população não selecionada de pacientes com idade≥70 anos, a intervenção coronária percutânea por via radial esteve associada à menor incidencia de desfechos clínicos hospitalares, em especial de eventos hemorrágicos relacionados à via de acesso vascular.
The femoral approach has remained, for more than two decades, as the main access route in percutaneous coronary intervention (PCI). Recent studies show that the choice of radial access is associated with considerable reduction in the risk of vascular and bleeding complications.1–3 Nevertheless, the radial technique still represents less than 10% of the approaches used in PCI worldwide, which can be explained by the demand for greater skill of the interventionist and for a longer learning curve.1 These facts are related to the characteristics of the vessel (of smaller caliber than the femoral artery), the anatomic variations, and the potential to cause arterial spasm.4
Although increasingly potent antithrombotic and antiplatelet drugs have reduced ischemic events related to PCI, the increase of bleeding complications associated with the procedure can lead to increased morbimortality.1,4,5 In this scenario, no strategy has caused greater impact than the use of the radial artery rather than femoral access in the reduction of bleeding events related to PCI.6
Among the independent predictors of bleeding related to PCI, older age has been demonstrated as an independent risk factor in several studies.7,8 This fact should lead to greater use of the radial approach in this population; however, due to the greater degree of atherosclerosis, calcification, and tortuosity of small- and medium-caliber vessels in this age group, PCI by radial approach can lead to higher failure rate, prolonged procedure, use of a greater amount of contrast, and greater exposure to radiation.9
The present study aimed to compare the clinical in-hospital outcome of transradial access use when compared with the femoral approach in patients aged≥70 years submitted to PCI.
METHODSPopulationThis study included consecutive patients aged≥70 years undergoing PCI in two high-volume hospital services in Curitiba (PR) from January 2012 to November 2013. Clinical and epidemiological data, as well as in-hospital clinical events, were collected and stored in the database, comparing the outcomes of safety and efficacy of the cohort submitted to PCI by radial approach vs. femoral access. The interventionists performing the procedures were skilledin both techniques.
At least 24 hours pre-PCI, patients treated electively received acetylsalicylic acid (loading dose of 300mg and maintenance dose of 100mg/day) and clopidogrel (loading dose of 300mg and maintenance dose of 75mg/day). Urgency or emergency cases, without enough time for the pre-treatment, received a loading dose of clopidogrel of 600mg or ticagrelor (loading dose of 180mg and maintenance dose of 90mg every 12 hours). All patients were instructed to maintain the dual antiplatelet therapy for at least one month in the case of bare-metal stent implantation, and for one year, if drug-eluting stents were used.
The stent implantation technique, the vascular access route, stent type, and the medications used during the procedure were chosen at the discretion of the interventionist.
DefinitionsRegarding efficacy endpoints, combined cardiovascular and cerebrovascular events (ECCAM), death, stroke, acute myocardial infarction (AMI), and target vessel revascularization (TVR) were evaluated, as well as the rates of these isolated events. Death was defined as death from any cause that occurred during hospitalization. Periprocedural AMI was defined as the presence of new Q-waves in two or more contiguous leads, or as elevation of creatine kinase MB isoenzyme (CK-MB) at least three times higher than the normal upper level. In cases of AMI, the 20% increase in CK-MB in comparison to previous levels was considered a diagnostic of reinfarction.
Regarding safety outcomes, vascular and bleeding complications were evaluated according to the Thrombolysis in Myocardial Infarction (TIMI)10 and ACUITY11 criteria. According to ACUITY, bleeding events were considered major (intracranial hemorrhage, intraocular hemorrhage, hematoma≥5cm in diameter, bleeding at the puncture site requiring intervention, any apparent bleeding with decrease in hemoglobin≥3mg/dL, decrease in hemoglobin≥4mg/dL without apparent site of bleeding, or need for transfusion) or minor (any bleeding which did not fit the above definition). According to the TIMI criteria, bleeding was considered as major (intracranial hemorrhage, clinically significant bleeding associated with a decrease in hemoglobin>5g/dL, or fatal bleeding), minor (any clinical signs of bleeding associated with the decrease in hemoglobin of 3g/dL to 5g/dL), or minimal (any clinical signs of bleeding associated with a decrease in hemoglobin<3g/dL).
STATISTICAL ANALYSISContinuous variables were described as means±standard deviations and compared by Student’s t-test for independent variables or the Mann-Whitney test, according to their distribution. Categorical variables were presented as percentages and compared using the chi-squared test or Fisher’s exact test, when appropriate. The effect of the access routeon vascular and bleeding complications was determined using a multivariate logistic regression model, adjusted for variables with p<0.05 as determined by the univariate analysis. The final model was adjusted for the presence of diabetes, gender, and body mass index. Statistically significant results were those with p<0.05. The SPSS version 12.0 (SPSS Inc., Chicago, United States) was used in the analyses.
Ethical aspectsThis study was approved by the Ethics Committee of the Pontificia Universidade Católica do Paraná (PUC-PR), number 459.434, with CAAE identification number 24075513.8.0000.0020 in the Brazil platform. Patients were included in the study after signing an informed consent.
RESULTSBetween January 2012 and November 2013, 832 consecutive patients underwent PCI at the participating institutions, performed by interventionists skilled in both techniques. Of these, 225 (27%) were aged≥70 years, of whom 117 (52%) were treated by transradial and 108 by femoral approach.
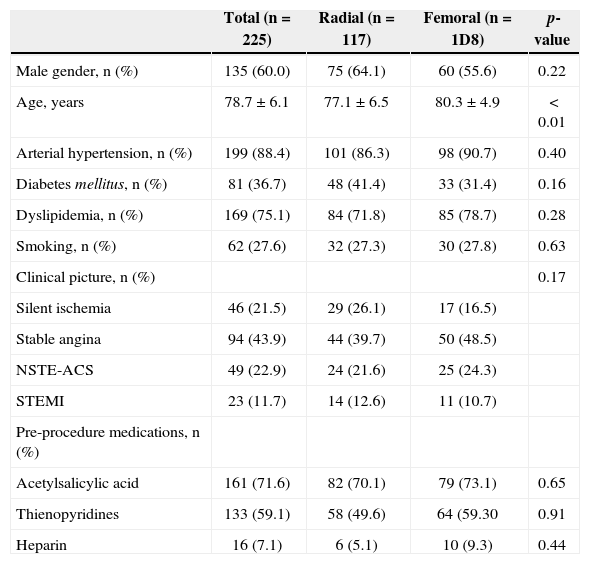
Except for age (77.1±6.5years vs. 80.3±4.9years; p<0.01), the other clinical characteristics did not differ between the groups (Table 1).
Clinical Characteristics
| Total (n=225) | Radial (n=117) | Femoral (n=1D8) | p-value | |
|---|---|---|---|---|
| Male gender, n (%) | 135 (60.0) | 75 (64.1) | 60 (55.6) | 0.22 |
| Age, years | 78.7±6.1 | 77.1±6.5 | 80.3±4.9 | < 0.01 |
| Arterial hypertension, n (%) | 199 (88.4) | 101 (86.3) | 98 (90.7) | 0.40 |
| Diabetes mellitus, n (%) | 81 (36.7) | 48 (41.4) | 33 (31.4) | 0.16 |
| Dyslipidemia, n (%) | 169 (75.1) | 84 (71.8) | 85 (78.7) | 0.28 |
| Smoking, n (%) | 62 (27.6) | 32 (27.3) | 30 (27.8) | 0.63 |
| Clinical picture, n (%) | 0.17 | |||
| Silent ischemia | 46 (21.5) | 29 (26.1) | 17 (16.5) | |
| Stable angina | 94 (43.9) | 44 (39.7) | 50 (48.5) | |
| NSTE-ACS | 49 (22.9) | 24 (21.6) | 25 (24.3) | |
| STEMI | 23 (11.7) | 14 (12.6) | 11 (10.7) | |
| Pre-procedure medications, n (%) | ||||
| Acetylsalicylic acid | 161 (71.6) | 82 (70.1) | 79 (73.1) | 0.65 |
| Thienopyridines | 133 (59.1) | 58 (49.6) | 64 (59.30 | 0.91 |
| Heparin | 16 (7.1) | 6 (5.1) | 10 (9.3) | 0.44 |
NSTE-ACS, non-ST-segment elevation acute coronary syndrome;
STEMI, ST-segment elevation myocardial infarction
The male gender predominated (60%), 36.7% were diabetics, and more than one-third underwent PCI in the presence of an acute coronary syndrome.
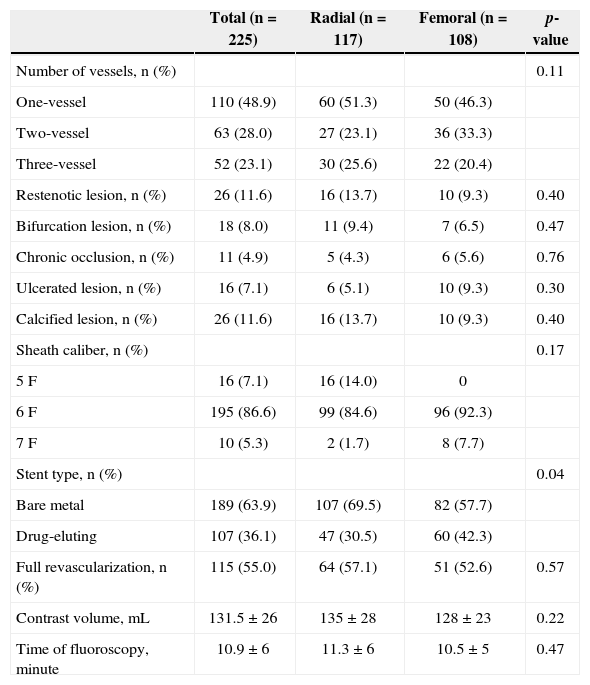
Regarding the procedure and angiographic variables (Table 2), approximately half the patients had involvement of two or three vessels, of which 11.6% were restenotic lesions; 8.0% had bifurcations lesions, and 4.9% had chronic occlusions, with no differences between the groups. Drug-eluting stents were used less often in the transradial than in the femoral group (30.5% vs. 42.3%; p=0.04). The amount of contrast medium used was 135±28mL in the radial group and 128±23mL in the femoral group (p=0.22). There was no difference between the fluoroscopy time between the groups (11.3±6 vs. 10.5±5 minutes; p=0.47).
Angiographic and procedural characteristics
| Total (n=225) | Radial (n=117) | Femoral (n=108) | p-value | |
|---|---|---|---|---|
| Number of vessels, n (%) | 0.11 | |||
| One-vessel | 110 (48.9) | 60 (51.3) | 50 (46.3) | |
| Two-vessel | 63 (28.0) | 27 (23.1) | 36 (33.3) | |
| Three-vessel | 52 (23.1) | 30 (25.6) | 22 (20.4) | |
| Restenotic lesion, n (%) | 26 (11.6) | 16 (13.7) | 10 (9.3) | 0.40 |
| Bifurcation lesion, n (%) | 18 (8.0) | 11 (9.4) | 7 (6.5) | 0.47 |
| Chronic occlusion, n (%) | 11 (4.9) | 5 (4.3) | 6 (5.6) | 0.76 |
| Ulcerated lesion, n (%) | 16 (7.1) | 6 (5.1) | 10 (9.3) | 0.30 |
| Calcified lesion, n (%) | 26 (11.6) | 16 (13.7) | 10 (9.3) | 0.40 |
| Sheath caliber, n (%) | 0.17 | |||
| 5F | 16 (7.1) | 16 (14.0) | 0 | |
| 6F | 195 (86.6) | 99 (84.6) | 96 (92.3) | |
| 7F | 10 (5.3) | 2 (1.7) | 8 (7.7) | |
| Stent type, n (%) | 0.04 | |||
| Bare metal | 189 (63.9) | 107 (69.5) | 82 (57.7) | |
| Drug-eluting | 107 (36.1) | 47 (30.5) | 60 (42.3) | |
| Full revascularization, n (%) | 115 (55.0) | 64 (57.1) | 51 (52.6) | 0.57 |
| Contrast volume, mL | 131.5±26 | 135±28 | 128±23 | 0.22 |
| Time of fluoroscopy, minute | 10.9±6 | 11.3±6 | 10.5±5 | 0.47 |
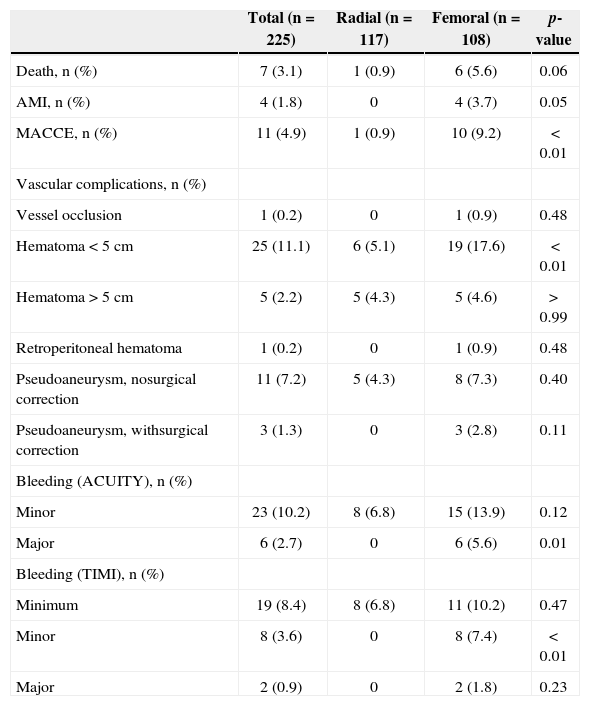
The in-hospital clinical outcomes (Table 3) death (0.9% vs. 5.6%; p=0.06), non-fatal AMI (3.7% vs. 0; p=0.05), and MACCE (0.9% vs 9.2%; p<0.01) were more frequently observed in the group undergoing PCI through the femoral artery. There was no stroke nor TVR in any of the patients analyzed.
In-hospital clinical outcomes
| Total (n=225) | Radial (n=117) | Femoral (n=108) | p-value | |
|---|---|---|---|---|
| Death, n (%) | 7 (3.1) | 1 (0.9) | 6 (5.6) | 0.06 |
| AMI, n (%) | 4 (1.8) | 0 | 4 (3.7) | 0.05 |
| MACCE, n (%) | 11 (4.9) | 1 (0.9) | 10 (9.2) | < 0.01 |
| Vascular complications, n (%) | ||||
| Vessel occlusion | 1 (0.2) | 0 | 1 (0.9) | 0.48 |
| Hematoma<5cm | 25 (11.1) | 6 (5.1) | 19 (17.6) | < 0.01 |
| Hematoma>5cm | 5 (2.2) | 5 (4.3) | 5 (4.6) | >0.99 |
| Retroperitoneal hematoma | 1 (0.2) | 0 | 1 (0.9) | 0.48 |
| Pseudoaneurysm, nosurgical correction | 11 (7.2) | 5 (4.3) | 8 (7.3) | 0.40 |
| Pseudoaneurysm, withsurgical correction | 3 (1.3) | 0 | 3 (2.8) | 0.11 |
| Bleeding (ACUITY), n (%) | ||||
| Minor | 23 (10.2) | 8 (6.8) | 15 (13.9) | 0.12 |
| Major | 6 (2.7) | 0 | 6 (5.6) | 0.01 |
| Bleeding (TIMI), n (%) | ||||
| Minimum | 19 (8.4) | 8 (6.8) | 11 (10.2) | 0.47 |
| Minor | 8 (3.6) | 0 | 8 (7.4) | <0.01 |
| Major | 2 (0.9) | 0 | 2 (1.8) | 0.23 |
AMI, acute myocardial infarction
MACCE, major adverse cerebrovascular and cardiovascular events
TIMI, Thrombolysis in Myocardial Infarction.
In the total sample, 21% of patients had a vascular complication, which ranged from minor hematomas to pseudoaneurysm formation requiring surgical intervention. It is noteworthy that no patient undergoing intervention through the radial access had major bleeding by any of the criteria, and there was no need for surgical correction of vascular complications in this group.
When comparing the rates of vascular complications, no differences were found between the groups, except for hematomas<5cm, which were more prevalent in the femoral access group (5.1% vs. 17.6%; p<0.01).
Bleeding defined by ACUITY and TIMI scores was numerically more frequent in the femoral group, showing statistical significance for the highest ACUITY criterion (0 vs. 5.6%; p=0.01), and the lowest of the TIMI criterion (0 vs. 7.4%; p<0.01).
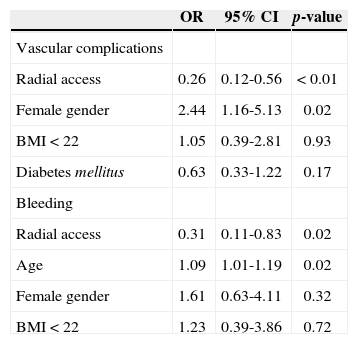
In the multivariate analysis, female gender was an independent predictor of vascular complications, and age was an independent predictor of bleeding. The only protective factor for the occurrence of the two complications was the use of radial access route (Table 4).
Predictors of vascular complications and bleeding
| OR | 95% CI | p-value | |
|---|---|---|---|
| Vascular complications | |||
| Radial access | 0.26 | 0.12-0.56 | <0.01 |
| Female gender | 2.44 | 1.16-5.13 | 0.02 |
| BMI<22 | 1.05 | 0.39-2.81 | 0.93 |
| Diabetes mellitus | 0.63 | 0.33-1.22 | 0.17 |
| Bleeding | |||
| Radial access | 0.31 | 0.11-0.83 | 0.02 |
| Age | 1.09 | 1.01-1.19 | 0.02 |
| Female gender | 1.61 | 0.63-4.11 | 0.32 |
| BMI<22 | 1.23 | 0.39-3.86 | 0.72 |
OR, odds ratio
95% CI
95% Confidence Interval
BMI, body mass index.
When comparing radial and femoral access in the performance of the PCI, the ideal strategy should offer reduced vascular and bleeding complications, which obviously affect post-procedure clinical evolution, while avoiding increased procedure time and/or radiation exposure.12,13
The first studies to compare the radial and femoral techniques suggested that the first, albeit safer, might not be suitable for widespread use in interventional procedures, as it increased procedure time and the amount of contrast; induced arterial spasm and caused discomfort to the patient; and promoted greater radiation exposure.14 However, with the increasing experience of the interventionist, improved materials, and drug therapy used in the prevention of vasospasm, that which was unreachable became attainable. The most influential factor regarding technical success has been the interventionist’s experience. In the present study, only interventionists skilled in the radial technique participated in the procedures.
In a previously reported registry, it was demonstrated that a volume>80 cases/year per surgeon significantly decreased failure of the radial approach and the time of procedure.15 Other studies similarly showed a reduction of radiation exposure, as surgeons’ experience increased.14,16
The use of the radial approach reduces the percentage of vascular complications when compared to the femoral approach.3,6 In the present study, 11% of patients had major complications related to the vascular access site, such as pseudoaneurysm, large hematoma (at the puncture site or even retroperitoneal), and vessel occlusion. The use of the radial access reduced not only the major vascular complications, but also bleeding complications, defined by the two different pre-specified classifications. Several analyses have demonstrated the superiority of the radial approach in reducing rates of bleeding, particularly in high-risk populations, such as women,17 the elderly,18 and patients with acute coronary syndrome.19
Few studies have evaluated the radial vs. femoral approach in the subgroup of elderly patients undergoing PCI. These studies included diagnostic procedures in the comparison, which does not require such a vast array of antiplatelet and antithrombotic drugs, a condition that greatly increases the risk of bleeding.9 Another study, which compared the two approaches in the elderly population undergoing PCI, did not analyze detailed outcomes related to bleeding.18 In a national series, of a group with extensive experience in radial access, there was no comparison with a control group of patients treated via femoral approach.20 Thus, the data of this study’s population corroborate the fact that the greater the potential for bleeding and vascular complications of a patient, the greater the benefit of considering the radial access as a priority when performing PCI.
In the studied population, an overall rate of in-hospital mortality of 3.1% was observed, with a marginal statistical difference between the radial and femoral groups.
Although the RIVAL study, with over 7,000 patients enrolled, demonstrated a reduction in mortality in the subgroup analysis of patients with STEMI, only a population>17,000 patients could consistently demonstrate this reduction in the presence of acute coronary syndrome.3 The authors consider the higher overall mortality in the femoral access group a result of selection bias. As this was a pragmatic observational study with broad inclusion, the use of femoral access may have been preferred in clinically more severe patients with hemodynamic instability.
Study limitationsLimitations included: the fact that this was an observational registry of clinical practice, subject to selection bias observed in non-randomized samples; the small number of patients included in the study; and the lack of late clinical follow-up.
CONCLUSIONSIn an unselected population of patients aged≥70 years undergoing percutaneous coronary intervention, radial approach was associated with a lower incidence of in-hospital clinical outcomes, especially bleeding events related to the access route.
CONFLICTS OF INTERESTThe authors declare no conflicts of interest.
FUNDING SOURCENone.