The 3-year results of the Symplicity HTN-1 trial have shown the superiority of renal sympathetic denervation over drug treatment in patients with resistant hypertension. However, the efficacy of renal sympathetic denervation was not confirmed by Symplicity HTN-3, the first sham-controlled study. Our objective was to report the safety and efficacy of renal sympathetic denervation using the irrigated radiofrequency ablation catheter in patients with resistant hypertension.
MethodsTwenty-one patients were submitted to the procedure since July 2012, nine of them had a follow-up≥12 months and were included in this analysis. The primary endpoint was safety, evaluated by periprocedural adverse events, renal function and renal vascular abnormalities at 6 months. Secondary endpoints included changes in blood pressure obtained in office and in the number of anti-hypertensive drugs at 12 months.
ResultsMean age was 48.8±11.7years. In the first case, there was a renal artery dissection caused by the vascular sheath. There were no cases of thrombosis, renal infarction or death. Serum creatinine levels did not increase during the follow-up period. At 6 months, one case of significant renal stenosis without clinical impact was diagnosed. The average reduction in office blood pressure was 41.1±33.2/18.6±15.2mmHg (p=0.04 for systolic blood pressure and p=0.08 for diastolic blood pressure) and there was a mean reduction of 2.0±2.3 in the number of anti-hypertensive drugs at 12 months (p=0.03).
ConclusionsRenal sympathetic denervation using the irrigated radiofrequency ablation catheter proved to be feasible, safe and effective.
Denervação Renal com Cateter de Ablação porRadiofrequência de Ponta Irrigada em Hipertensos Resistentes
IntroduçãoResultados de 3 anos do Symplicity HTN-1 mostraram superioridade da denervação simpática renal percutânea comparada à terapia medicamentosa em hipertensos resistentes. Entretanto, os desfechos de eficácia da denervação simpática renal percutânea no Symplicity HTN-3, primeiro ensaio controlado com procedimento simulado, não foram alcançados. Nosso objetivo foi relatar os resultados de segurança e de eficácia da denervação simpática renal percutânea utilizando o cateter de ablação por radiofrequência de ponta irrigada em hipertensos resistentes.
MétodosVinte e um pacientes foram submetidos ao procedimento desde julho 2012, dentre eles nove com seguimento≥12 meses, os quais foram incluídos nesta análise. O desfecho primário foi a segurança, avaliada por eventos adversos peri-procedimento, função renal e anormalidade vascular renal aos 6 meses. Os desfechos secundários incluíram mudanças na pressão arterial obtida no consultório e no número de anti-hipertensivos aos 12 meses.
ResultadosA média de idades foi 48,8±11,7 anos. No primeiro caso, houve dissecção de artéria renal causada por trauma da bainha. Nenhum caso de trombose, infarto renal ou óbito foi observado. Não se constatou elevação dos níveis séricos de creatinina durante o seguimento. Aos 6 meses, diagnosticouse um caso de estenose significativa de artéria renal, sem repercussão clínica. A redução média da pressão arterial no consultório foi de 41,1±33,2/18,6±15,2mmHg (p=0,04 para pressão arterial sistólica e p=0,08 para pressão arterial diastólica) e houve redução de 2,0±2,3 no número de anti-hipertensivos aos 12 meses (p=0,03).
ConclusõesA denervação simpática renal percutânea, utilizando o cateter de ablação por radiofrequência de ponta irrigada, mostrou ser factível segura e eficaz.
Aiming to promote sympathetic nervous system activity inhibition or blockade, percutaneous renal sympathetic denervation (RSD) has emerged as an adjunct treatment for patients with resistant arterial hypertension. The medical community has enthusiastically followed the results of RSD since the publication of Schlaich et al.,1 which reported, for the first time, the reduction in blood pressure (BP) in resistant hypertensive patients (using seven different antihypertensive agents) from 161/107mmHg to 127/81mmHg after the procedure. The exponential growth of research and the number of publications related to the subject is remarkable.2 Medical device companies have evaluated RSD as a great innovation and a successful therapy for millions of patients, and currently there are more than 60 companies involved with this modality of treatment. Trials such as Symplicity HTN-13 and Symplicity HTN-24 showed significant decreases in BP, confirming the efficacy and safety of RSD. The three-year follow-up of Symplicity HTN-1 disclosed the maintenance of long-term results, with a reduction in BP of 32/14mmHg.5 These unprecedented results exceeded those achieved with drug therapy and contributed to increase enthusiasm for the new technique.
Symplicity HTN-3, a randomized, blinded, and sham-controlled trial was presented at the American College of Cardiology Congress and published online in the New England Journal of Medicine on the same day in March 2014. Bhatt et al.6 caused controversy by presenting their results. At six months, the relative reduction in systolic BP (SBP) was similar for both groups (p<0.001 for changes related to blood pressure levels pre-RSD in both groups), with a difference between groups of only –2.39mmHg in favor of RSD. In addition, a prespecified difference in SBP measured by 24-hour ambulatory BP monitoring (ABPM) of only 2mmHg was not achieved. Thus, the primary and secondary endpoints of RSD efficacy were not achieved in Symplicity HTN-3. The results contradicted most of previously published studies, despite a recent study suggesting inferiority of the RSD compared to adjusted drug treatment.7
Initially, the most plausible explanation for the unfavorable results of the Symplicity HTN-3 was the inclusion of a control group with sham procedure. In clinical trials testing medical devices and interventions, control with sham procedure is analogous to the use of a placebo in pharmaceutical trials. However, for ethical reasons, the control sham procedure is usually discouraged. Both the Symplicity HTN-1 and HTN-2 had no control group with sham procedure.
For this reason, the placebo effect can explain all or most of the observed differences in BP in the first two trials. The lack of efficacy of RSD may also have been caused by incomplete or ineffective denervation. There is no mention of markers of RSD efficacy, such as microneurography and spillover of norepinephrine, methods that measure direct and indirect sympathetic activity, respectively. However, the ablation catheter used in Symplicity HTN-3 was also used in Symplicity HTN-1 and HTN-2.
In Brazil, however, catheters dedicated to RSD were not available until recently. Nevertheless, although two systems, the Symplicity® (Medtronic®, Minneapolis, United States) and EnligHTN® (St. Jude Medical®, Minneapolis, United States), have already been approved by the Brazilian National Sanitary Surveillance Agency (Agência Nacional de Vigilância Sanitária – ANVISA), for clinical use, they are not yet routinely used in Brazil. Supported by the potential benefits of irrigated catheter in cardiac ablations, which cause deeper lesions with less risk of thrombus formation at the catheter tip, this center has been using this type of catheter for RSD for nearly two years, based on the hypothesis that irrigated-tip catheters may be beneficial in this context, and to evaluate the feasibility and safety of RSD with irrigated catheters in patients with resistant systemic arterial hypertension (SAH). The authors recently published results from the first ten patients undergoing the procedure; with a six-month follow-up.8 The present objective was to report the results of up to 12 months of RSD using the irrigated catheter in this population.
METHODSSamplePatients with resistant SAH followed at the Clinic of Nephrology and Hypertension of Instituto Dante Pazzanese de Cardiologia were evaluated for inclusion in the study. The definition of resistant hypertension was based on the consensus of the American Heart Association:9 patients should have SBP measured at the office>140mmHg, despite the use of three or more antihypertensive drugs, or controlled BP with≥four antihypertensive agents with synergistic action. The diagnosis of resistant hypertension should have been confirmed by at least one ABPM during follow-up.
All BP measurements were performed with an automatic brachial sphygmomanometer and in accordance with the standards of VI Brazilian Guidelines on Arterial Hypertension.10 The choice of drug treatment for BP control was at the discretion of the attending physician, according to the tolerance profile and associated comorbidities. Treatment compliance was encouraged in all medical appointments.
Poor adherence to drug treatment was excluded by hospitalization for at least five days before surgery. Hospital stay was also used to supplement and update the investigation of secondary causes of hypertension.
The exclusion criteria comprised patients with glomerular filtration rate<45mL/min; severe liver disease; coagulation disorders; functional class III or IV heart failure (according to the functional classification of the New York Heart Association-NYHA); severe ventricular dysfunction (ejection fraction [EF]<0.30); moderate or severe valvular heart disease; severe arrhythmias; acute myocardial infarction or stroke in the last six months; unresolved angina and/or myocardial ischemia; renal artery abnormalities (stenosis>50%, presence of previous angioplasty or stent, solitary kidney); renal artery diameter<4mm; surgical history in the last two months; hypersensitivity to contrast media; suspected pregnancy; history of alcoholism in period of less than one year; mental illness that would compromise monitoring; and life expectancy<one year.
The protocol for this research project, as well as the informed consent were duly approved by the Ethics Committee in Research of Instituto Dante Pazzanese de Cardiologia. All patients signed an informed consent.
Clinical outcomesThe primary study endpoint was the safety of the procedure, assessed by the rate of periprocedural adverse events (vascular complications at the puncture site and renal artery), analysis of renal function (comparison between baseline and six months after the intervention), and occurrence of stenosis/aneurysm in the renal artery at six months after the intervention, assessed by angiography.
Secondary endpoints comprised changes in BP measured at the office at 12 months of follow-up, as well as analysis of the procedure effect on the number of antihypertensive drugs used during this period.
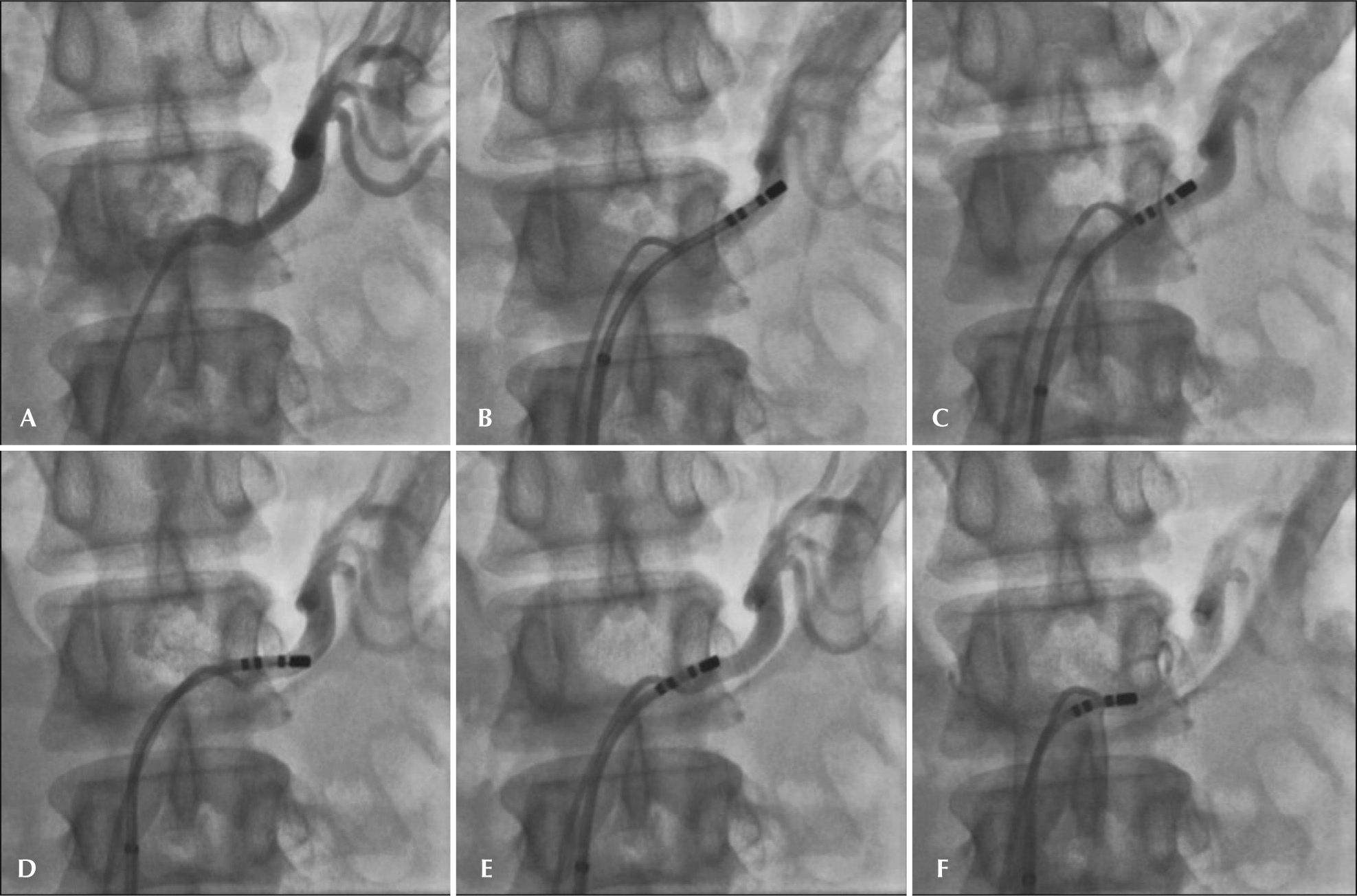
Procedure descriptionTwo vascular accesses were obtained by the team according to standardized method, one in the right femoral artery and another in the left femoral artery. The left femoral artery was used for catheter insertion to inject a contrast medium for renal arteriography. The right femoral artery was used for insertion of a sheath through which the Therapy Cool Point® ablation catheter (St. Jude Medical®, Minneapolis, United States) or Celsius Thermocool® (Biosense-Webster Inc.®, Diamond Bar, United States) was inserted and placed in the renal artery. After obtaining vascular access, unfractionated heparin was administered at a dose of 100 U/kg for anticoagulation. Aortography along the renal arteries, followed by catheterization and selective renal arteriography for anatomy evaluation and positioning of the ablation catheter in the distal portion were performed after the intravascular administration of nitroglycerin (200 mcg). Four to six sequential applications of radiofrequency were performed along both renal arteries to promote renal denervation. The catheter was retracted 5mm and rotated after each application, configuring a helical disposition of ablations (Figure 1).
– Sequential radiofrequency lesions in the renal artery. (A) Selective angiography of the left renal artery; (B to F) sequential applications initiated in the distal segment; the catheter was retracted and rotated after each application to promote sequential lesions with helical configuration.
Due to intense visceral pain generated by the ablation, sedation/analgesia with narcotics and opioids was performed in all cases. At the end of the procedure, renal arteriography was performed for evaluation of vascular integrity after intravascular administration of nitroglycerin (200 mcg).
Post-procedural evaluation and clinical follow-upThe sheaths were removed when the activated coagulation time reached values<200sec. Manual hemostatic compression was conducted for at least 20 minutes, followed by compression bandage. Walking was permitted after four hours of rest, in the absence of bleeding at the puncture site. After the procedure, attention was given to the occurrence of vascular complications at the femoral access, such as hematomas and pseudoaneurysms. The medications were adjusted and patients were advised regarding the need for regular monitoring.
The first return visit was conducted 7±2 days after the procedure and aimed at evaluating puncture site complications, kidney function, hemoglobin/hematocrit levels, and adjusting the dose of antihypertensive drugs. The following visits were carried out at 30±7, 90±10, 180±10, and 360±10 days. BP measurement was the same as described for the preprocedure evaluation. Laboratory tests were ordered at all visits. Angiography of the renal arteries was repeated at six months of follow-up.
Statistical AnalysisContinuous variables were expressed as mean and standard deviation and compared using the Student’s t-test; categorical variables were expressed as absolute and relative frequencies. For all parameters, p-values≤0.05 were considered statistically significant. Data were analyzed using SPSS® software, version 16, for Windows® (SPSS® Inc., Chicago, Illinois, United States).
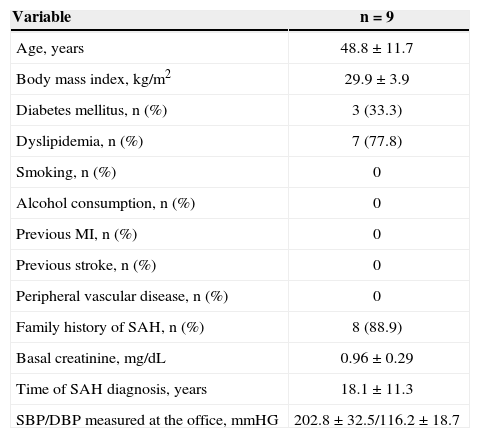
RESULTSClinical characteristicsTwenty-one patients underwent RSD for the adjunct treatment of resistant SAH. Among them, nine patients (eight women) with follow-up≥12 months were included in this analysis. The mean age was 48.8±11.7years. The mean time from diagnosis of SAH was 18.1±11.3years. Mean SBP and diastolic BP (DBP) measures at the office were 202.8±32.5mmHg and 116.2±18.7mmHg, respectively. The mean number of anti-hypertensive drugs before the procedure was 7.7±1.3. The clinical characteristics of the patients are shown in Table 1.
Basal characteristics
| Variable | n=9 |
|---|---|
| Age, years | 48.8±11.7 |
| Body mass index, kg/m2 | 29.9±3.9 |
| Diabetes mellitus, n (%) | 3 (33.3) |
| Dyslipidemia, n (%) | 7 (77.8) |
| Smoking, n (%) | 0 |
| Alcohol consumption, n (%) | 0 |
| Previous MI, n (%) | 0 |
| Previous stroke, n (%) | 0 |
| Peripheral vascular disease, n (%) | 0 |
| Family history of SAH, n (%) | 8 (88.9) |
| Basal creatinine, mg/dL | 0.96±0.29 |
| Time of SAH diagnosis, years | 18.1±11.3 |
| SBP/DBP measured at the office, mmHG | 202.8 ± 32.5/116.2±18.7 |
MI, myocardial infarction; SAH, systemic arterial hypertension; SBP, systolic blood pressure; DBP, diastolic blood pressure.
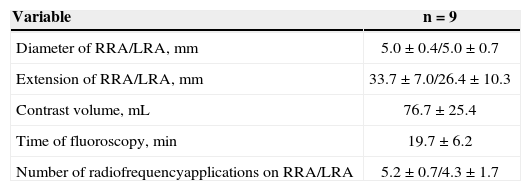
The mean diameters of the left and right renal arteries were 5.0±0.4mm and 5.0±0.7mm, respectively. The mean length of the left and right renal arteries was 33.7±7.0mm and 26.4±10.3mm, respectively.
One case had one polar artery on the left, and another, three polar arteries were observed, two on the left and one on the right. Two patients had mild proximal renal artery stenosis (Table 2).
Angiographic and technical characteristics of the procedure
| Variable | n=9 |
|---|---|
| Diameter of RRA/LRA, mm | 5.0±0.4/5.0±0.7 |
| Extension of RRA/LRA, mm | 33.7±7.0/26.4±10.3 |
| Contrast volume, mL | 76.7±25.4 |
| Time of fluoroscopy, min | 19.7±6.2 |
| Number of radiofrequencyapplications on RRA/LRA | 5.2±0.7/4.3±1.7 |
RRA, right renal artery; LRA, left renal artery.
All procedures were performed via transfemoral access according to the protocol described herein. On average, 76.7±25.4mL of contrast medium was used for 19.7±6.2minutes of fluoroscopy. The mean number of RF applications was 5.2±0.7 in the right renal artery and 4.3±1.7 in the left renal artery (Table 2).
Safety of the procedureThe procedure was performed without complications in eight cases. In the first case of this series, a renal artery dissection was detected after the ablation was performed due to mechanical trauma caused by the sheath. She was treated with stenting without subsequent increase in complications or hospital stay. At six months, renal arteriography showed patency and no significant in-stent hyperplasia.
Focal parietal irregularities in the renal artery were observed in some cases immediately after radiofrequency application, having been attributed to spasms and/or edema. None was considered limiting to blood flow after the procedure.
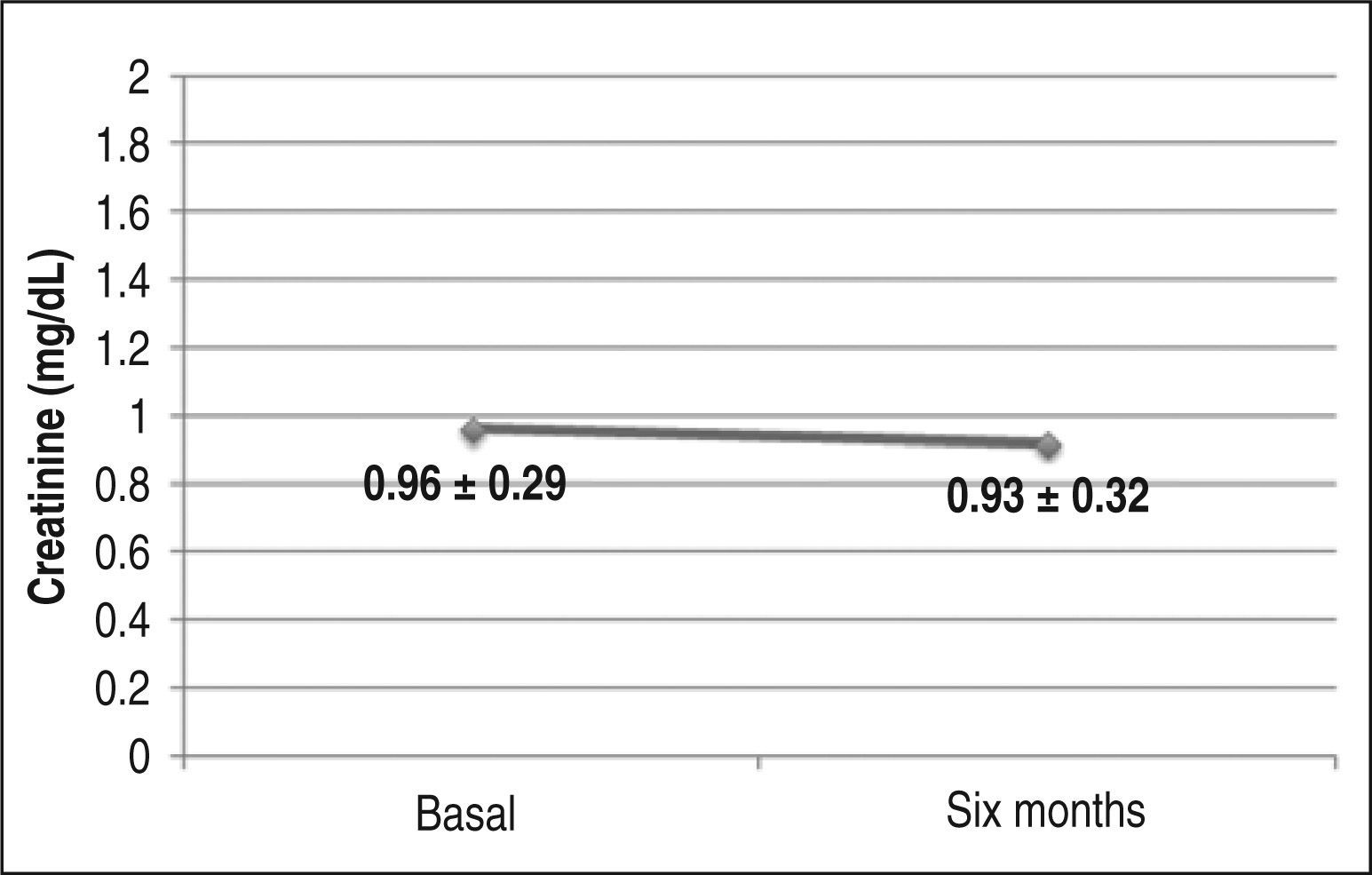
There were no complications related to femoral puncture during the periprocedural period. There was no increase in serum creatinine (basal 0.96±0.29mg/ dL vs. 0.93±0.32mg/dL at 6 months), indicating maintenance of glomerular filtration rate during follow-up (Figure 2).
Renal vascular safetyRenal arteriography was performed in all patients at six months follow-up. In one case, there was evidence of significant degree of left renal artery stenosis (70%). Although it had no clinical significance, it was uneventfully treated with stent implant.
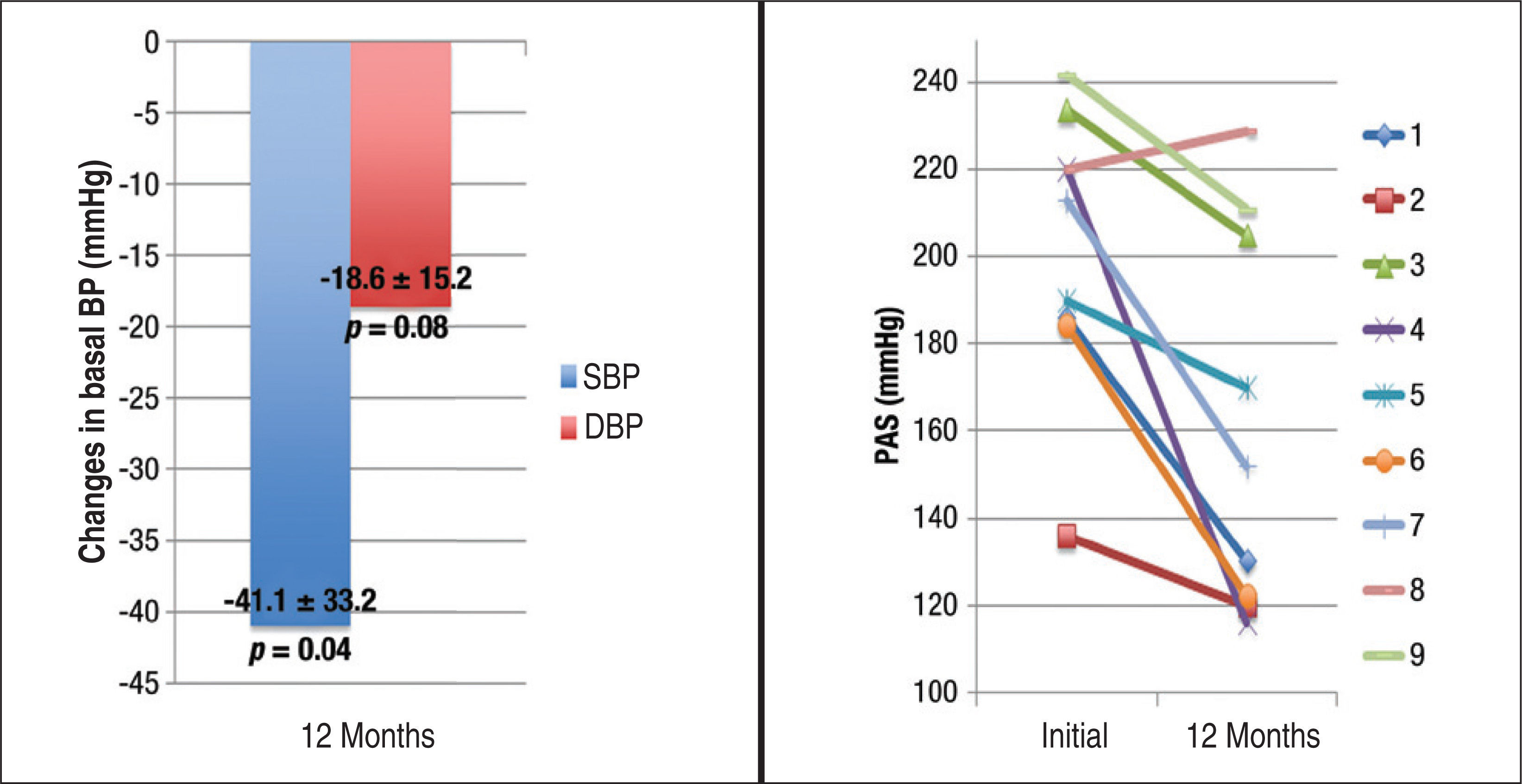
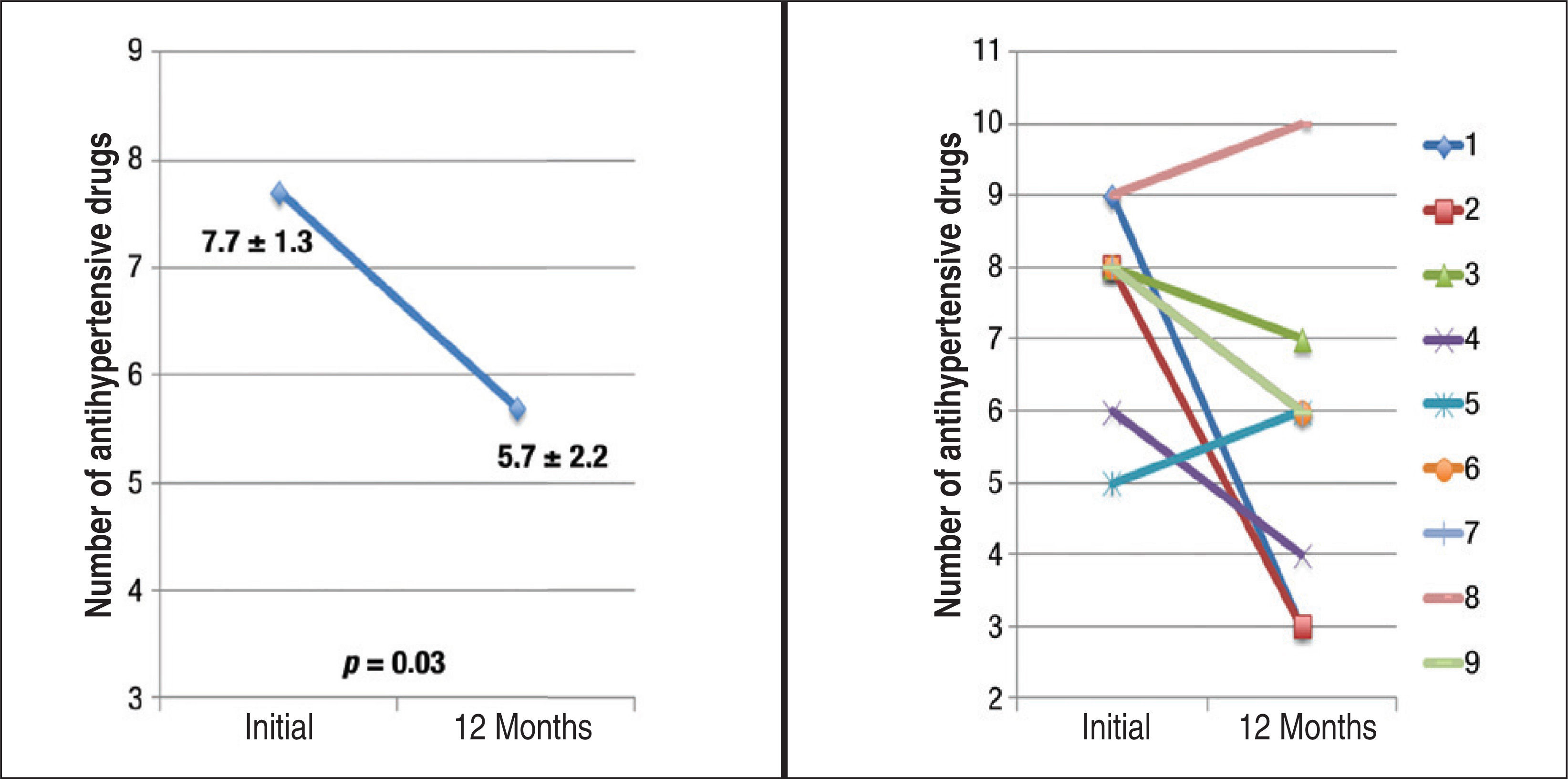
Effects on blood pressure and number of antihypertensive drugs at 12 monthsAfter 12 months of follow-up, RSD reduced BP measured at the office, on average, by 41.1±32.2/18.6±15.2mmHg (p=0.04 for SBP, and p=0.08 for DBP) (Figure 3). There was a mean reduction of 2±2.3 antihypertensive drugs prescribed at 12 months (basal 7.7±1.3 vs. 5.7±2.2 at 12 months, p=0.03) (Figure 4).
– On the left, effect of renal sympathetic denervation on blood pressure (BP) measured in the office. On the right, effect of renal sympathetic denervation on systolic blood pressure (SBP) measured in the office in each of the nine patients submitted to the procedure. DBP, diastolic blood pressure.
Anti-hypertensive response was observed in eight (88.9%) patients, with a reduction of up to 104mmHg for SBP. Only one patient did not show a reduction in BP levels. A reduction of up to six anti-hypertensive drugs at the 12-month follow-up was also observed.
DISCUSSIONThis study was conducted at a tertiary cardiology center, which used irrigated ablation catheter for radiofrequency application in the context of RSD in patients with resistant hypertension. The results showed that ablation of the renal sympathetic activity using an irrigated catheter is feasible, safe, and effective.
The procedure reduced SBP and DBP measured in the office, on average, by 41.1±32.2mmHg and 18.6±15.2mmHg, respectively. There was a mean reduction of 2±2.3 anti-hypertensive drugs. A reduction of up to six anti-hypertensive drugs and up to 104mmHg in SBP was observed during follow-up. Symplicity HTN-3 did not report changes in the number of anti-hypertensive drugs, and the mean reduction in SBP was only 2.4mmHg compared to the control group.
The SBP decrease in Symplicity HTN-3 was observed both in the RSD group and in the control group – a divergent finding when compared to previous studies; moreover, the decrease was approximately half of that observed in the Symplicity HTN-2, despite the fact that the basal blood pressures were similar in the two studies. This is intriguing, as the degree of BP reduction is related to pretreatment BP levels. Comparison between the control groups of the Symplicity HTN-3 and HTN-2 studies shows a greater reduction in BP in the former study. It is plausible that greater exposure to spironolactone (28.7% vs. 17% of patients) in Symplicity HTN-3 facilitated this decrease. Differently from the mentioned trials, most patients in the present population were taking spironolactone (88.9%).
The great variability in response to RSD raises the question of how this procedure could be more effective in selected patients, especially those with sympathetic hyperactivity. The rate of non-responders to treatment with RSD (defined as reduction in SBP<10mmHg six months after the procedure) varies from 8% to 37% in the main clinical trials. The causes of this finding are not yet fully understood; however, some assumptions can be made based on knowledge of the physiopathology of SAH and the RSD procedure. Among them, the following are emphasized: (1) significant variability of devices and techniques, including RF power used, number of electrodes, and duration of ablation; (2) the actual relevance of sympathetic hyperactivity in the physiopathology of resistant hypertension, as this is a multifactorial disease and, in some cases, the sympathetic nervous system contribution may not be as important for disease expression; (3) the inadequate selection of patients, including patients with pseudo-resistance and secondary hypertension; and (4) patient-related conditions such as non-adherence to pharmacological treatment and failure to change lifestyle. The standard deviations of changes in the initial SBP measured at the office for both groups (RSD and control) in Symplicity HTN-1 and HTN-2 were broad and very similar, indicating a large variation in response. The change in SBP in 95% of patients in Symplicity HTN-2 was between –78mmHg and 14mmHg in the RSD group, and between –43mmHg and 41mmHg in the control group. In Symplicity HTN-3, the mean BP reduction was also within this range for both groups. In the present population, the standard deviation was 33.2mmHg and the change in SBP ranged between –104mmHg and 9mmHg. A satisfactory response was not obtained in only one patient (11.1%).
Other differences between Symplicity HTN-3 and the present study deserve to be mentioned. First, the present patients needed a greater number of antihypertensive drugs at baseline (7.6±1.3 vs. 5.1±1.4). Second, due to the smaller number of patients, it was possible to confirm resistant SAH based on hospital admissions, while Symplicity HTN-3 established the diagnosis in outpatient consultations, which may have overestimated basal blood pressure levels. Third, in Symplicity HTN-3, changes in doses of anti-hypertensive drugs were allowed only if the patient had symptoms related to hypotension. In the present study, the drug dose was changed aiming at the control recommended by the VI Brazilian Guidelines on Hypertension;10 in patients in whom baseline BP was controlled with four or more antihypertensive drugs, there was no significant reduction in BP, but a decrease in the number of drugs at the follow-up. Finally, the present study used a nondedicated catheter for RSD – the irrigated tip catheter designed for cardiac ablation. It is believed this represents the major difference regarding the present study’s approach to RSD, allowing for the achievement of superior results.
The authors have published the effects of three different catheters, usually used for cardiac ablation, in an in vitro experiment with porcine renal arteries.11 It was verified that the irrigated catheter (usually indicated for ablation of arrhythmias in heart chambers located on the left) results in deeper lesions, causing full destruction of nerves, useful for promoting the ablation of those located beyond 4mm of the arterial intimal layer, which can comprise up to 40% of the nerves in the renal arteries. These results were consistent with those published by Ahmed et al.,12 who described ten patients with resistant SAH submitted to RSD with irrigated catheter. The authors demonstrated reductions in SBP and DBP of 21 and 11mmHg, respectively, at six months of follow-up, as well as absence of severe complications.
The enthusiasm about RSD has been widespread, as shown by the statements: “the potential of renal denervation is huge” and “it can be used not only to treat hypertension, but also diseases that are characterized by sympathetic overactivity, such as diabetes and hyperinsulinemia, heart failure, arrhythmias, and chronic renal failure”.13 These carefully phrased words mention the benefits of renal denervation for these metabolic or cardiovascular alterations. In contrast, the current findings of Symplicity HTN-3 by the same authors, six months later, attest that “no significant effect was observed on SBP”. Additional assessment in strictly designed clinical trials will be necessary to confirm the previously reported benefits of RSD in patients with resistant SAH. The unanswered question is what the real role of RSD is as an adjunct treatment in SAH. Science requires caution and time will answer this question.
LimitationsAmong the main limitations of this study are its nonrandomized design, the small sample size, and lack of a control group. Despite these limitations, the results appear promising and are consistent with the existing literature. Randomized controlled trials with a sham procedure are necessary to confirm the present results.
CONCLUSIONSPercutaneous RSD using the irrigated radiofrequency ablation catheter proved to be feasible, safe, and effective.
CONFLICTS OF INTERESTThe authors declare no conflicts of interest.
SOURCES OF FUNDINGNone.