In addition to providing greater comfort and convenience for the patient, the radial approach is associated to lower rates of vascular complications and major bleeding, with potential impact on morbidity and mortality. Thus, the adoption of strategies that reduce the risk of arterial occlusion after invasive procedures, enabling it to be reused, is desirable.
MethodsControlled prospective registry evaluating the impact of routine adoption of a selective radial compression device in patients with acute coronary syndrome without ST-segment elevation undergoing early invasive stratification through the radial access. Arterial patency was assessed by the Barbeau test at hospital discharge and at the 30-day follow-up.
ResultsFifty-nine patients were evaluated, of which 83% underwent ad hoc percutaneous coronary intervention. Mean age was 64±12.2, 66.1% were male and 28.8% had diabetes mellitus. The right radial access was used in 98.3% of cases, the number of catheters was 2.4±0.6, with a diameter of 6F in all cases, and the duration of the procedure was 32.4±12.7minutes. Spasm was reported in 10.2% of cases, hematoma>5cm in 3.4% and occlusion of the radial artery after the procedure and at 30 days in 6.8% and 3.4% of the cases, respectively.
ConclusionsThe TR Band® radial compression device is safe and effective in obtaining reduced rates of radial artery occlusion after invasive coronary procedures.
Utilização de Pulseira Compressora Seletiva na Prevenção da Oclusão da Artéria Radial Após Procedimento Coronário Invasivo
IntroduçãoO acesso radial, além de propiciar maior conforto e comodidade, associa-se a menores taxas de complicações vasculares e sangramento grave, com potencial impacto na morbimortalidade. Assim, é desejável a adoção de estratégias que reduzam o risco de oclusão arterial após procedimentos invasivos, possibilitando sua reutilização.
MétodosRegistro prospectivo, controlado, que avaliou o impacto da utilização rotineira de pulseira compressora seletiva em pacientes com síndrome coronariana aguda sem supradesnivelamento do ST submetidos à estratificação invasiva pelo acesso radial. A patência arterial foi avaliada por meio do teste de Barbeau, na alta hospitalar e aos 30 dias de evolução.
ResultadosForam avaliados 59 pacientes, dos quais 83% realizaram intervenção coronária percutânea ad hoc. A média de idades foi de 64±12,2 anos, 66,1% eram do sexo masculino e 28,8% portadores de diabetes mellitus. O acesso radial direito foi utilizado em 98,3% das intervençôes, o número de cateteres foi 2,4±0,6, com diâmetro de 6F em todos os casos, e a duração dos procedimentos foi de 32,4±12,7 minutos. Espasmo foi reportado em 10,2%, hematoma>5cm em 3,4% e oclusâo da artéria radial após o procedimento e aos 30 dias em 6,8 e 3,4% dos casos, respectivamente.
ConclusõesA pulseira compressora TR Band® é dispositivo seguro e eficaz na obtenção de taxas reduzidas de oclusão radial, após procedimento coronário invasivo.
When compared to femoral access, the radial access is associated with a lower rate of complications at the arterial puncture site, allows for earlier ambulation, provides greater comfort to the patient after the procedure, and shows proven cost-effectiveness.1,2 Current trials indicate that the choice of the radial technique brings benefit in reducing mortality during percutaneous coronary intervention (PCI) and primary combined rate of death, myocardial infarction (AMI), and stroke in patients with acute coronary syndrome (ACS) undergoing invasive stratification in centers classified as having high-volume for this access route.3,4 Thus, the adoption of strategies that reduce the risk of radial artery occlusion after coronary procedure is desirable, allowing its reutilization.
In spite of device miniaturization increasing the ratio between the arterial diameter and the sheath, use of hydrophilic materials, systematic heparinization, and spasmolytic drug infusions, the rate of radial artery occlusion evaluated by plethysmography remains between 7 and 12%.5 The aim of this study was to determine the incidence of radial artery occlusion after routine use of a selective radial compression device, aiming to attain hemostasis while maintaining antegrade flow in patients with ACS managed through invasive procedure.
METHODSProspective registry, controlled, that assessed the efficacy and safety of the TR Band® (Terumo Medical, Tokyo, Japan) selective compression device in preventing vascular complications at the radial puncture site, with emphasis on the rate of arterial occlusion, after invasive coronary procedures.
The outcomes of interest, i.e., occlusion of the radial artery, hematoma, pseudoaneurysm, arteriovenous fistula, compartment syndrome, and severe bleeding, were evaluated during hospitalization and on the 30th day of follow-up, during medical consultation.
The pre-procedural permeability of the palmar arch was assessed through Allen’s test and the oximeter test.6 The plethysmographic patterns were classified as type A (no wave attenuation after radial artery compression), B (wave attenuation), C (transitory loss of tracing, reestablished within 2min) and D (loss of tracing without wave restoration).
DefinitionsAsymptomatic arterial occlusion was defined as the interruption of arterial blood flow, without manifestations of cell metabolism impairment or blood tissue failure. Severe bleeding was defined as type 3 (3a – bleeding with hemoglobin decrease≥3g/dL and<5g/dL or packed red blood cell transfusion; 3b – bleeding with hemoglobin decrease≥5g/dL, or cardiac tamponade, or bleeding requiring surgical intervention, or bleeding requiring intravenous vasoactive drug use; or 3c – intracranial hemorrhage, or subcategories confirmed by autopsy, imaging assessment, or lumbar puncture, or intraocular bleeding with vision impairment) or type 5 (5a – likely fatal bleeding, and 5b-definitive fatal bleeding).6 The hematomas were graded as type I, ≤ 5cm in diameter; type II, ≤ 10cm; or type III, > 10cm, without reaching the elbow; type IV, hematoma extending beyond the elbow; or type V, any hematoma with ischemic injury to the hand.7 Clinical success was defined as PCI performance with reduction of target stenosis to a diameter<20%, while maintaining or restoring normal antegrade flow (Thrombolysis in Myocardial Infarction (TIMI) grade 3), and absence of severe clinical complications (death, AMI, or coronary artery bypass graft surgery [CABG]). Device success was defined as achievement of adequate hemostasis at the end of the procedure using the TR Band® selective compression device, with no need to change to a compressive dressing. The duration of the procedure and fluoroscopy time were measured from the beginning of arterial puncture until sheath withdrawal.
Hemostasis technique while maintaining antegrade flowTo achieve hemostasis, the TR Band® radial compression device was used according to the previously validated protocol.8 Immediately after the procedure, the sheath was withdrawn by approximately 2cm. The device was applied to the patient with a green marker (located in the center of the largest balloon) positioned exactly at the puncture orifice, facilitating the localization, visualization, and control of possible bleeding. The balloon was inflated with the appropriate syringe and 15mL of air was injected, with simultaneous and complete withdrawal of the sheath, observing, at the end, the absence of active bleeding. After the fourth hour and at each subsequent hour (fifth and sixth hours), 5mL of air were slowly released, keeping the balloon connected to the syringe and controlling the plunger with the thumb. In case of bleeding at any stage of device withdrawal, the required volume of air was once again injected to maintain hemostasis, repeating the process after 60 minutes.
The maintenance of antegrade flow was measured by the plethysmographic curve obtained at the ipsilateral thumb to the puncture. Once the compression device was applied, the ulnar wrist was compressed, and the oximetric curve was verified in a period of up to two minutes, indicating patent flow. If the curve was not restored, the bracelet balloon gradually emptied until it was restored, and the occurrence of bleeding was the limiting factor. In the event of device failure, hemostasis was obtained with compressive dressing, using a porous adhesive elastic bandage.
Assessment of radial artery patencyRadial artery patency was assessed 24 hours after the procedure and on the 30 day follow-up using Barbeau’s test.9 By placing a pulse oximeter on the patient’s thumb, the appearance of the plethysmographic wave was verified. Subsequently, radial and ulnar arteries were compressed until the disappearance of the signal. Releasing only the radial artery, wave restoration was verified, confirming its patency, and its lack of restoration was interpreted as arterial occlusion.
Statistical analysisQualitative variables were summarized as absolute frequencies and percentages. Quantitative data were described as means and standard deviations.
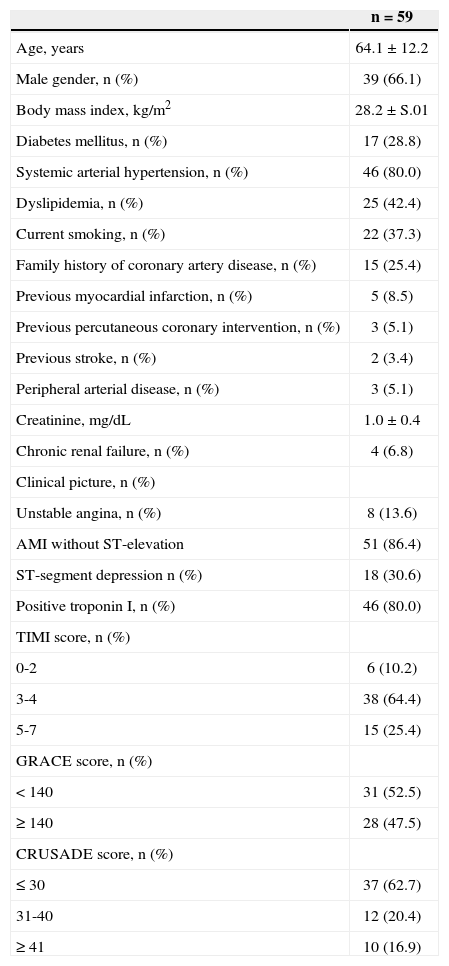
RESULTSFrom July 2013 to February 2014, 59 patients diagnosed with ACS without ST elevation were submitted to early invasive stratification. The mean age was 64±12.2years, 66.1% were male, and 28.8% had diabetes mellitus.
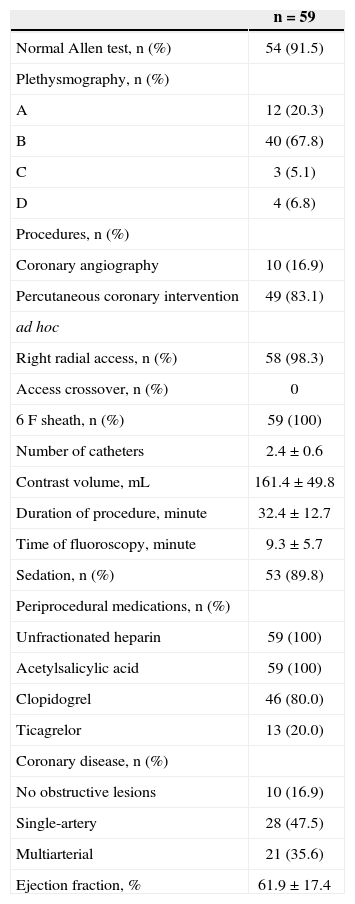
Regarding the indications, risk scores, and characteristics of the procedures, the high percentage of patients with AMI without ST elevation (86.4%), GRACE score≥140 in 47.5% of cases and ad hoc PCI in 83.1% of cases are noteworthy. (Tables 1 and 2).
Baseline clinical characteristics
| n=59 | |
|---|---|
| Age, years | 64.1±12.2 |
| Male gender, n (%) | 39 (66.1) |
| Body mass index, kg/m2 | 28.2±S.01 |
| Diabetes mellitus, n (%) | 17 (28.8) |
| Systemic arterial hypertension, n (%) | 46 (80.0) |
| Dyslipidemia, n (%) | 25 (42.4) |
| Current smoking, n (%) | 22 (37.3) |
| Family history of coronary artery disease, n (%) | 15 (25.4) |
| Previous myocardial infarction, n (%) | 5 (8.5) |
| Previous percutaneous coronary intervention, n (%) | 3 (5.1) |
| Previous stroke, n (%) | 2 (3.4) |
| Peripheral arterial disease, n (%) | 3 (5.1) |
| Creatinine, mg/dL | 1.0±0.4 |
| Chronic renal failure, n (%) | 4 (6.8) |
| Clinical picture, n (%) | |
| Unstable angina, n (%) | 8 (13.6) |
| AMI without ST-elevation | 51 (86.4) |
| ST-segment depression n (%) | 18 (30.6) |
| Positive troponin I, n (%) | 46 (80.0) |
| TIMI score, n (%) | |
| 0-2 | 6 (10.2) |
| 3-4 | 38 (64.4) |
| 5-7 | 15 (25.4) |
| GRACE score, n (%) | |
| <140 | 31 (52.5) |
| ≥140 | 28 (47.5) |
| CRUSADE score, n (%) | |
| ≤30 | 37 (62.7) |
| 31-40 | 12 (20.4) |
| ≥41 | 10 (16.9) |
TIMI; Thrombolysis in Myocardial Infarction.
Characteristics of procedures
| n=59 | |
|---|---|
| Normal Allen test, n (%) | 54 (91.5) |
| Plethysmography, n (%) | |
| A | 12 (20.3) |
| B | 40 (67.8) |
| C | 3 (5.1) |
| D | 4 (6.8) |
| Procedures, n (%) | |
| Coronary angiography | 10 (16.9) |
| Percutaneous coronary intervention | 49 (83.1) |
| ad hoc | |
| Right radial access, n (%) | 58 (98.3) |
| Access crossover, n (%) | 0 |
| 6F sheath, n (%) | 59 (100) |
| Number of catheters | 2.4±0.6 |
| Contrast volume, mL | 161.4±49.8 |
| Duration of procedure, minute | 32.4±12.7 |
| Time of fluoroscopy, minute | 9.3±5.7 |
| Sedation, n (%) | 53 (89.8) |
| Periprocedural medications, n (%) | |
| Unfractionated heparin | 59 (100) |
| Acetylsalicylic acid | 59 (100) |
| Clopidogrel | 46 (80.0) |
| Ticagrelor | 13 (20.0) |
| Coronary disease, n (%) | |
| No obstructive lesions | 10 (16.9) |
| Single-artery | 28 (47.5) |
| Multiarterial | 21 (35.6) |
| Ejection fraction, % | 61.9±17.4 |
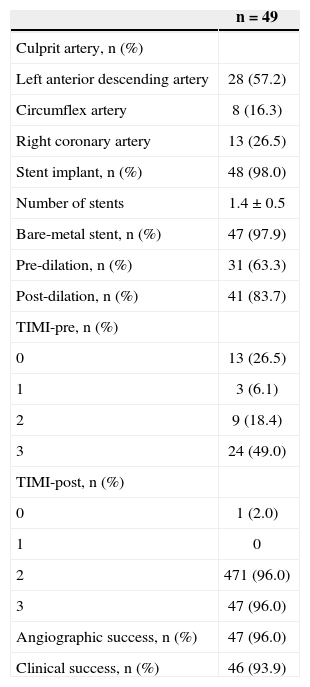
Angiographic and clinical success was achieved in 96.0% and 93.9% of the PCIs, respectively (Table 3).
Characteristics of the percutaneous coronary intervention
| n=49 | |
|---|---|
| Culprit artery, n (%) | |
| Left anterior descending artery | 28 (57.2) |
| Circumflex artery | 8 (16.3) |
| Right coronary artery | 13 (26.5) |
| Stent implant, n (%) | 48 (98.0) |
| Number of stents | 1.4±0.5 |
| Bare-metal stent, n (%) | 47 (97.9) |
| Pre-dilation, n (%) | 31 (63.3) |
| Post-dilation, n (%) | 41 (83.7) |
| TIMI-pre, n (%) | |
| 0 | 13 (26.5) |
| 1 | 3 (6.1) |
| 2 | 9 (18.4) |
| 3 | 24 (49.0) |
| TIMI-post, n (%) | |
| 0 | 1 (2.0) |
| 1 | 0 |
| 2 | 471 (96.0) |
| 3 | 47 (96.0) |
| Angiographic success, n (%) | 47 (96.0) |
| Clinical success, n (%) | 46 (93.9) |
TIMI; Thrombolysis in Myocardial Infarction.
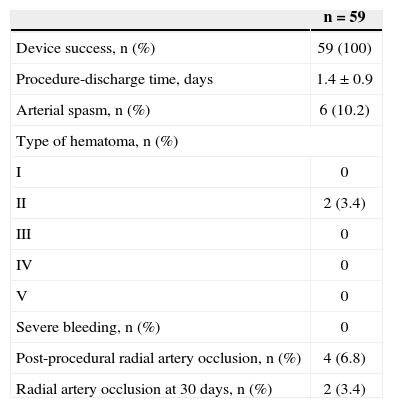
Radial hemostasis with antegrade flow maintenance was achieved in 84.7% of patients. In the remaining patients, despite the use of the selective compression device, an oximetric curve consistent with arterial patency was not identified. The rate of hematoma at the puncture site was 3.4% (all type II), and the arterial occlusion incidence after the procedure and at 30 days was 6.8% and 3.4%, respectively, with no evidence of ischemic injury to the hand (Table 4).
Device success and vascular complications at the arterial puncture site
| n=59 | |
|---|---|
| Device success, n (%) | 59 (100) |
| Procedure-discharge time, days | 1.4±0.9 |
| Arterial spasm, n (%) | 6 (10.2) |
| Type of hematoma, n (%) | |
| I | 0 |
| II | 2 (3.4) |
| III | 0 |
| IV | 0 |
| V | 0 |
| Severe bleeding, n (%) | 0 |
| Post-procedural radial artery occlusion, n (%) | 4 (6.8) |
| Radial artery occlusion at 30 days, n (%) | 2 (3.4) |
Radial artery occlusion is the most reported complication with this access route, whose incidence has ranged from 1.5 to 33%.10,11 Although asymptomatic in most cases, with rare reports of severe ischemia, this occurrence prevents its use in future procedures. Once diagnosed, up to 50% of cases may show spontaneous recanalization at 30 days; validated strategies for its prevention include 3,000-5,000 U of unfractionated heparin during the procedure, the use of hydrophilic sheaths and devices with lower diameter, and, more recently, the use of hemostasis techniques with antegrade flow maintenance.5,12,13
Its physiopathology is associated with an interaction of factors, such as local trauma, spasm, and occlusive thrombus formation. Predictors for its occurrence comprise female gender, young individuals, patients with diabetes mellitus, non-heparinization during the procedure, and absence of antegrade flow when attaining hemostasis.14
In fact, compared to the conventional technique of hemostasis with compression bandage in 436 patients undergoing transradial coronary angiography, hemostasis with antegrade flow maintenance significantly reduced the rate of occlusion of the radial artery by 59 and 75% 24 hours after and 30 days after the procedure, respectively.5
Evidence shows that the maintenance of radial artery patency during hemostasis is the most important parameter for reducing the risk of arterial occlusion. In a randomized trial involving 400 coronary diagnostic procedures, the incidence of early (7%) and late (5%) radial occlusion in patients with antegrade flow during the process of hemostasis were independent from the use of unfractionated heparin at the start of the examination.14 Thus, in selected cases, heparinization could be omitted in diagnostic procedures through radial access, as long as hemostasis was attained with maintenance of arterial patency.
In the present study, involving a population of patients with ACS of predominantly medium to high risk, despite the routine use of 6F sheaths, ad hoc percutaneous coronary intervention in 83% of cases, the greater manipulation and the changing of catheters, and the mean duration of the procedure of 32 minutes, the authors obtained rates of arterial occlusion at discharge and at 30 days of 6.8% and 3.4%, respectively. The findings of the pre-procedure evaluation of palmar arch permeability through Allen’s test or oximetry do not represent contraindication to the procedure by radial approach, and cases with persistent arterial occlusion at 30 days did not exhibit an altered Allen’s test or plethysmographic curve type D in the initial screening.
The main limitation of this analysis, in addition to the small sample size, was the non-routine performance of radial artery Doppler ultrasound prior to hospital discharge, which could underestimate the true incidence of complications,11 although the close correlation between Barbeau’s test, applied to all patients, and the findings of Doppler ultrasound has been described. In addition, this was a single-center, non-randomized study, performed in a service with high volume of procedures using the transradial approach.
CONCLUSIONSThe TR Band® selective compression device is safe and effective for attaining reduced rates of radial occlusion after performing invasive coronary procedures, adding to the validated strategies to prevent this complication.
CONFLICTS OF INTERESTThe authors declare no conflicts of interest.
FUNDING SOURCENone.