The upper limb compartment syndrome is considered an emergency. It may cause necrosis and loss of functionality of the hand. The principal treatment is fasciotomies. However, there are therapeutic possibilities that may help or avoid surgery, provided there is always the option to do a fasciotomy when conservative treatment fails.
ObjectiveTo assess the clinical response and treatment safety with stellate ganglion block and cervical epidural anesthesia in a patient with compartment syndrome of both upper limbs.
Methods and materialsDescriptive longitudinal prospective study in a case report format, of a patient with compartment syndrome of both upper extremities that underwent a stellate ganglion block and cervical epidural anesthesia for treating her condition. The patient was followed for 7 days. The recovery of sensitivity and the mobility were assessed on both hands, in addition to pain intensity and bilateral distal cyanosis improvement.
ResultsThe patient evolved satisfactorily with evidence of recovery of sensitivity and mobility in both hands, adequate pain control and immediate and bilateral improved distal cyanosis.
ConclusionsSympathetic block and epidural cervical analgesia are a treatment option for the comprehensive approach of the compartment syndrome, as long as the patient receives constant monitoring of any alarm signs and a surgeon is immediately available to do fasciotomies if the intervention therapy fails.
el síndrome compartimental en la extremidad superior es considerado una urgencia. Puede generar necrosis y pérdida de la funcionalidad de la mano. El principal tratamiento es con fasciotomías. Sin embargo, existen posibilidades terapéuticas que pueden ayudar o evitar la cirugía, siempre y cuando exista la posibilidad rápida de realizar una fasciotomía si la terapia conservadora fracasa.
Objetivoevaluar la respuesta clínica y la seguridad al tratamiento con bloqueo del ganglio estrellado y analgesia epidural cervical en una paciente con síndrome compartimental de ambos miembros superiores.
Métodos y materialesestudio descriptivo longitudinal prospectivo tipo reporte de caso en una paciente con síndrome compartimental de ambos miembros superiores en la que se realizó un bloqueo del ganglio estrellado y analgesia epidural cervical como medida en el tratamiento de su enfermedad. Se realizó un seguimiento durante 7 días. Se evaluaron la recuperación de la sensibilidad y de la movilidad en ambas manos, la intensidad del dolor y la mejoría de la cianosis distal bilateral.
Resultadosla paciente evoluciona satisfactoriamente, se evidencia recuperación de la sensibilidad y movilidad en ambas manos, con adecuado control del dolor y mejoría de la cianosis distal de manera inmediata y bilateral.
Conclusionesel bloqueo simpático y la analgesia epidural cervical son una alternativa terapéutica en el tratamiento integral del síndrome compartimental siempre y cuando el paciente reciba una monitorización continua de los signos de alarma y tenga la disponibilidad inmediata de un cirujano de mano para realizar fasciotomías en caso de que el tratamiento intervencionista falle.
The compartment syndrome is an entity secondary to an increase in pressure within one or several compartments. The diagnosis is mainly clinical. The disproportionate early onset of pain is the key warning sign.1
The acute compartment syndrome is more often seen in patients under 35 years of age2; although it is usual for this phenomenon to occur in the upper extremity secondary to fractures or trauma, less frequent, non-trauma causes should also be considered: infections, blood dyscracias, renal syndrome, spider bites, snake bites, extravasation of infusions or contrast media, injection of illicit drugs and extended compression of the extremity.3–5 There is also the risk of masking the syndrome and making a late diagnosis when the patient is under the effects of regional anaesthesia, since the patient would not experience any pain.6
The treatment is aimed at achieving an early recovery of the microcirculation into the compartment through decompression.7 It is considered a surgical emergency; however, intervention management may be considered in some selected cases through the sympathetic block of the extremity, improving distal perfusion and reducing the interstitial pressure, provided there is an interdisciplinary team that ensures surveillance of any alarm signs and provides emergency surgical decompression.8
Case descriptionA 51-year-old female patient is admitted to the CES clinic (Medellín, Colombia), with a diagnosis of compartment syndrome of the upper limbs triggered by bee stings induced at an alternative medicine center for treating a chronic hand pain. The alarm signs included intense pain, areas of hypoesthesia and dysesthesia, finger pulp cyanosis and functional limitation. The patient receives initial treatment with intravenous steroid and antihistaminic. A surgeon and anesthesiologist evaluation is required for fasciotomies of both upper extremities. Both specialists carry out a joint evaluation of the patient and the following plan was agreed:
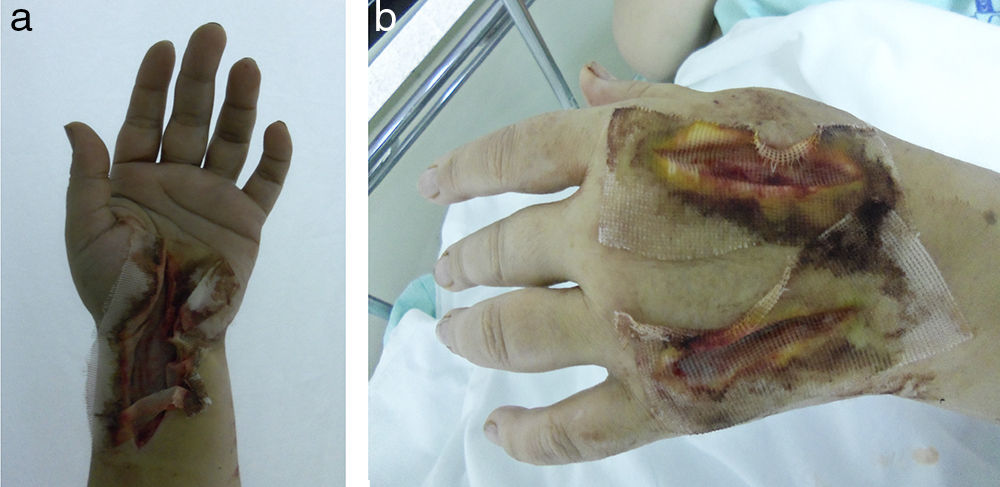
Fasciotomies of the upper left limb under general anesthesiaAfter asepsis and antiasepsis of the extremity, an incision is made on the volar aspect, from the distal third of the forearm along the midline between the flexor carpi radialis and palmaris longus up to Kaplan's line (Fig. 1). Another incision is immediately made of the complete transverse ligament and the skin wound is left opened. Then, on the dorsal side of the hand, two incisions are made: one between the second and third metacarpal and the second one between the fourth and fifth metacarpal. The wounds are left opened and covered with sterile bandages. Surgery is programmed every 48h for wound cleansing and the decision to close the wound is based on the extent of the edema. The wounds were closed on day seven.
Fluoroscopically guided interventional therapy of the upper right limb:- •
Stellate ganglion block: using a 22 spinal needle and paratracheal technique, the C6 transverse apophysis is identified and confirmed with water soluble contrast media followed by the administration of 6mL of 0.75% levobupivacaine (Fig. 2).
- •
Cervical epidural catheter: the epidural space is localized at C3 C4 with epidural needle and loss of resistance technique with saline solution, confirmed by 1mL of contrast media; the epidural catheter is then introduced, leaving three centimeters inside the space and a 3mL of 1% lidocaine test is done with 15μg of epinephrine that came out negative. Following tunnelization of the catheter the continuous infusion is initiated at a rate of 6mL/h with a mixture of 0.9% saline solution with levopuvicaine at a 0.125% concentration to treat the pain in both extremities and extend the sympathetic block (Fig. 3).
A continuous evaluation of the alarm signs is maintained for the first 12h and daily follow-up for 7 days until the left side wounds are closed. The patient evolves satisfactorily with evidence of recovery of sensitivity and mobility of both hands, with adequate pain control and immediate and bilateral improvement of the distal cyanosis.
DiscussionThe muscle groups of the extremities are divided into compartments made up of strong muscle fasciae. The upper limb has 15 compartments and the most frequently affected is the forearm volar compartment.3
The use of bee venom as a therapeutic agent for the relief of pain dates back to Hippocrates times. This technique called apitherapy is widely used in Asia, Europe and South America.9 The therapeutic effect is achieved through the anti-inflammatory properties of bee venom, via a substance called Mellitin that is believed to be five times as potent as Cortisone; however, there are no current trials in humans, since the practice of this technique is potentially dangerous.10,11
The diagnosis of the compartment syndrome is clinical and the manifestations are known as the five “Ps”: pain, pallor, pulselessness, paresthesias and passive extension of pain to the affected muscle group. In the final stages skin manifestations such as epidermolysis may be observed, and bullae secondary to marked edema inside the compartment.12 Occasionally, objective diagnosis tests are needed: a pressure measurement inside the compartment above 30mmHg is diagnostic; and in hypotensive patients a difference of less than 20mmHg between the diastolic blood pressure and intracompartment pressure is suggestive of the syndrome.12
The initial management is aimed at an early recovery of the microcirculation to the affected compartment through surgical decompression with fasciotomies.13
There are other options such as interventional management with sympathetic blockade of the extremity under fluoroscopic or ultrasound visualization, aimed at improving the distal perfusion and reducing the interstitial pressure. Based on the pathophysiology of this condition and the important sympathetic component in the course of its evolution, the sympathetic block is suggested as a therapeutic approach during the initial stages of the compartment syndrome.
The stellate ganglion block has been used historically with different therapeutic, diagnostic and prognostic purposes.5 It is useful in reducing sympathetic nervous system mediated pain, achieving symptom relief from the vasodilation effect that optimizes blood perfusion and from enhanced collateral circulation, as well as from its impact on relaxing muscle spasms.4,14 The stellate ganglion block has also been described in situations such as extravasation of contrast media and vasoppressors in the upper limb,4,5,15 supporting the hypothesis of the potential role of the sympathetic nervous system in the pathogenesis of acute pain. The sympathetic nerve block disrupts the pain cycle and lowers the arteriolar basal tone in response to an acute inflammatory process, facilitating the recovery of the painful zone and the restoration of somatic sensation.5,16 Another advantage of the stellate ganglion block is that it facilitates early postoperative assessment of the neuromuscular function since it does not cause motor blockade.17
The most widely used technique for this block under fluoroscopic guidance is the anterior paratracheal approach, localizing the most prominent transverse cervical hypophysis (C6, known as Chaussignac's tubercle) and confirming with contrast media.17 The successful block is verified with the presence of ipsilateral Horner's syndrome, a temperature difference of 2°C between the two extremities (with a higher temperature in the blocked side), vasodilatation of the venous system in the arm and hand, as well as decreased or absent sweating in the affected extremity.4 As any other procedure, this block has some adverse effects and risk of complications, including: intra-arterial injection, epidural or spinal administration, hematomas, chest neuralgia, pneumothorax, recurrent phrenic or laryngeal nerve block, loss of the cardio-accelerating activity (with secondary bradycardia and hypotension), brachial plexus injury and dysphonia.
In recent years, the use of ultrasound has enabled this block under direct visualization of all the structures, improving safety.18
In the clinical practice, the commonly used technique to identify the epidural space is the blind technique with loss of resistance using air or saline; however, several reports have shown that this blind procedure at the cervical level may fail in 53% of the cases and hence the use of fluoroscopic guidance has been established for considerably improved localization and lower risk of complications.19 Likewise, the continuous cervical epidural infusion allows for pain control and extended sympathetic block of the upper extremities.
Some case reports have indicated that the compartment syndrome has been masked with regional block; this does not mean that there is a causal relationship, but what is important is that the patient receives information about warning signs other than pain and that the hospital team is more vigilant.
ConclusionsIn conclusion, we reported the successful management of a female patient with a diagnosis of compartment syndrome in the upper limbs, following bee stings, where the high rate of suspicion of the condition and early interdisciplinary treatment were fundamental. Sympathetic nerve block and cervical epidural anesthesia contribute to the recovery of the arteriolar basal tone in response to an acute inflammatory process, improving distal perfusion and achieving adequate pain control. This becomes then a therapeutic alternative in the comprehensive treatment of the compartment syndrome, provided that the patient is constantly monitored for any alarm signs and has a hand surgeon immediately available for fasciotomies in case the interventional therapy fails. Furthermore, the use of imaging guidelines such as fluoroscopy or ultrasonography should be emphasized in these procedures for improved efficacy and fewer complications.
FundingFunding for this article was with the authors’ own resources and the advice of CES University.
Conflicts of interestThe authors have no conflicts of interest to declare.