Clinical case discussion and non-systematic literature review on lactate and base deficit in trauma, its pathophysiology and prognostic value.
Materials and methodThe case of a polytraumatized patient that underwent major vascular and orthopedic surgery, ICU management and outcomes is discussed with the approval of the Ethics Committee of our Institution. The literature search included Pub Med, Scielo and Bireme.
ResultsLactate and base deficit are early follow-up clinical tools in trauma for identifying anaerobic metabolism, in addition to evaluating and changing the resuscitation strategy. This model is applicable to cardiovascular surgery.
ConclusionsBoth in trauma and cardiovascular surgery, lactate and base deficit are biomarkers that need to be quantified very early and in a serial manner. They are independent predictive factors for mortality in trauma patients in the first 48h.
Similarly, the base deficit allows for an early staging of patients in shock and for establishing with a high probability the need for blood by-products or mass transfusion.
Further studies are required for normotensive patients.
Presentación de un caso clínico y revisión no sistemática de la literatura sobrelactato y déficit de bases en trauma, su fisiopatología y su valor pronóstico.
Material y métodoCon autorización del comité de ética de nuestra institución, se presenta el caso de un paciente politraumatizado sometido a cirugía vascular mayor y ortopédica, su manejo en la UCI y su desenlace. La búsqueda bibliográfica se realizó en Pub Med, Scielo y Bireme.
ResultadosEl lactato y el déficit de bases son herramientas clínicas de seguimiento muy temprano en trauma para detectar metabolismo anaeróbico. Igualmente evaluar y modificarla estrategia de reanimación. Este modelo es aplicable a cirugía cardiovascular.
ConclusionesEn trauma y cirugía cardiovascular, el lactato y el déficit de bases constituyen biomarcadores que se deben cuantificar de manera muy temprana y seriada, constituyendo un factor predictivo independiente de mortalidad dentro de las primeras 48 h en los pacientes con trauma. Igualmente, el déficit de base permite una estratificación temprana de los pacientes que se presentan en estado de choque y determinar con alta probabilidad su necesidad de hemoderivados o transfusión masiva. Se requieren más estudios relacionados con los pacientes normotensos.
Inadequate or insufficient oxygen delivery results in anaerobic metabolism. The level of anearobiosis is proportional to the depth and severity of the hemorrhagic shock reflected by the base deficit and the level of lactate. In the presence of oxygen in the mitochondria, per every molecule of glucose, 36 ATP are produced during oxidative phosphorylation, in addition to water and carbon dioxide. In anaerobic conditions, pyruvate accumulates due to the failure of the pyruvate dehydrogenase enzyme to turn it into acetyl CoA. The excessive amount of pyruvate is converted into lactate through the action of lactic dehydrogenase. This system generates only 2 ATP molecules. Lactate is then used as metabolic fuel through Cori cycle or lactic acid. Lactate is an indicator sensitive to the presence and the severity of anaerobic metabolism. Its normal serum concentration is <2mmol/L. Actually, two categories of lactic acidosis have been described: Type A where lactic acidosis occurs with tissue hypoxia and Type B, where lactic acidosis occurs without tissue hypoxia (Tables 1 and 2 and Fig. 1).1–3
Causes of lactic acidosis type B (no clinical evidence of tissue hypoxia).
| Medical causes | Diabetes mellitus, pheochromocytoma, thiamine deficiency |
| Toxic agents | Ethanol, methanol, salicylates, sorbitol |
| Inborn metabolic errors | Pyruvate dehydrogenase deficiency, oxidative phosphorylation defects, glucose 6-phosphate deficit |
| Miscellaneous | Hypoglycemia |
The Ethics Committee of our organization authorized this case discussion of a 30-year old male patient who was the driver in a car crash but did not loose consciousness. The physical examination revealed chest trauma with dissection of the descending aorta, left femur fracture, fracture of the left distal radius and of the fifth left hand digit, in addition to pneumothorax and pulmonary contusion of the left lung. The patient was managed with closed thoracotomy (see Fig. 2).
The transesophageal ultrasound evidenced a normal biventricular systolic function.
Surgical management: descending aortic graft, bleeding packing.
The patient was admitted to the ICU with a left-sided double lumen endotracheal tube and continuous cardiac output monitoring. The surgery lasted for 10h; clamp time of 320min and extracorporeal circulation of 349min with a beating heart. Complications: bleeding and coagulopathy. 15units of platelets, 8units of plasma, and 6units of red blood cells were transfused. The orthopedist placed an external tutor in the left femur.
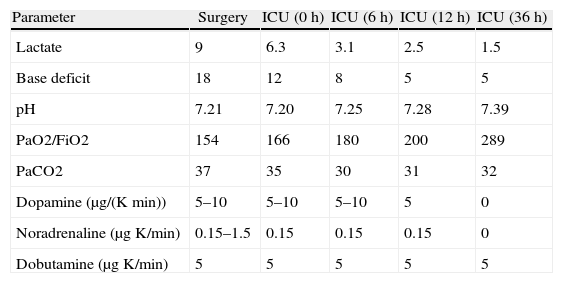
The resuscitation in the ICU was accomplished using isotonic crystals, hypertonic agents (3% hypertonic saline solution) and colloids (20% albumin). Sedation with fentanyl for RASS-2. Table 3 depicts the lactate behavior, base deficit, vasopressor support, inotropes, invasive ventilation and gasimetry during surgery and in the ICU.
Lactate trends, base deficit, vasopressor support, inotropes, invasive ventilation and gasimetry.
| Parameter | Surgery | ICU (0h) | ICU (6h) | ICU (12h) | ICU (36h) |
| Lactate | 9 | 6.3 | 3.1 | 2.5 | 1.5 |
| Base deficit | 18 | 12 | 8 | 5 | 5 |
| pH | 7.21 | 7.20 | 7.25 | 7.28 | 7.39 |
| PaO2/FiO2 | 154 | 166 | 180 | 200 | 289 |
| PaCO2 | 37 | 35 | 30 | 31 | 32 |
| Dopamine (μg/(Kmin)) | 5–10 | 5–10 | 5–10 | 5 | 0 |
| Noradrenaline (μgK/min) | 0.15–1.5 | 0.15 | 0.15 | 0.15 | 0 |
| Dobutamine (μgK/min) | 5 | 5 | 5 | 5 | 5 |
Table 4 shows the glycemic control and urinary output during surgery and in the ICU. Impaired normal values.
The protective ventilator strategy is illustrated in Table 5. Neurologically the patient is alert, is responsive to orders and is able to move his four limbs. Antibiotic prophylaxis with oxaciline infusion associated with aminoglycoside up to 24h after final closure. The kidney was protected with n-acetyl cysteine for 48h.
Ventilation strategy.
| Ventilation parameter | Surgery | ICU (0h) | ICU (24h) | ICU (36h) |
| Ventilation mode | A/C | A/C | A/C | APRV |
| Tidal volumen (ml/kg) | 7 | 7 | 7 | - |
| PEEP | 10 | 10 | 10 | - |
| Peak pressure | 25 | 22 | 25 | - |
| MIP | 25 | 28 | 28 | - |
A/C: Assisted controlled, APRV: Air Pressure Realice Ventilation, MIP: Maximum Inspiratory Pressure.
Source: Authors’.
Thirty-six hours later the patient is transferred for surgical unpacking. Twelve hours after readmission, the patient is successfully extubated upon reaching satisfactory airway scores and adequate Cuff Leak Test and Tobin.4 The patient stayed in the ICU for four days and was discharged from hospital on the tenth day; 90-day telephone follow-up was done with satisfactory evolution.
Literature reviewLactate and base deficitBlood base deficit (BD) was introduced by Ole Siggard-Andersen in 1950 with the idea of quantifying the non-respiratory component in the acid–base imbalance.5 Lactate is a biomarker mainly used in trauma and sepsis. The first scenario is associated with a hypoxic tissue response to the accumulation of pyruvate – a lactate precursor. By contrast, in sepsis there is a dysfunction of the pyruvate dehydrogenase enzyme, responsible for converting pyruvate into AcetylCoA, resulting in increased lactate levels in the presence of oxygen.1,6 Alcohol and psychoactive substances (cocaine, meta-amphetamines or phenylcyclidines), quite common in multiple trauma patients, affect the precision of lactate and base deficit.7 In case of trauma, there are no differences in terms of the origin of arterial or venous lactate and requires a baseline analysis within the first two hours after the patient is admitted, with continued serial measurements to determine clearance.8 The baseline value and early clearance are independent factors for early mortality (less than 48h). Short quantification intervals are suggested – between 2 and 3h – until the sixth to the ninth hour, and a clearance rate of 20%/h or 60% in 6h.9,10 Additionally, lactate clearance enables the evaluation of the resuscitation process and the quantification of the scope of the primary lesion.9–11 Extremely high baseline values with poor early clearance are a reflection of hypoxic tissue damage and unfavorable outcomes.
With regards to normotensive patients undergoing trauma, there are conflicting opinions about their usefulness and prognostic value.9,10 In a subgroup of patients over 65 years of age with penetrating trauma, lactate and excess base are associated with a significant rise in mortality.12
Lactate is currently a very important tool in cardiovascular anesthesia and intensive postoperative cardiac care. In patients undergoing myocardial revascularization, valve changes, with or without extracorporeal circulation, lactate is an independent predictor of early mortality and of any type of associated surgical re-intervention.13 Extracorporeal circulation and the use of the intra-aortic counterpulsation balloon rise lactate values and reduce clearance.14–16
Finally, the lactate value at admission to the ER in young patients with blunt and/or penetrating trauma, with systolic pressure ranging between 90 and 110mmHg, is more effective at predicting the risk of receiving over 6units of red blood cells during the first 24h post-injury and hospital mortality, versus the systolic pressure value.17
As a matter of fact, the key argument is: What is the best tool to individually analyze the metabolic and respiratory contribution to the acid–base status at a particular PaCO2 and pH?18
The theoretical importance lies on the fact that of the three approaches, the base deficit is the only one valid (Boston School, Stewart's physical-chemical approximation; Base Deficit, Copenhague's approach) that solves the stoichiometric problem. This means that an index should quantify the amount of strong acid or base to correct any acid–base disturbance.18,19
Base deficit and lactate are correlated with hemorrhagic shock but the former is a sound indicator of actual effective circulating volume.19 Likewise, these biomarkers are oxygen debt indicators.20 Among the normotensive patients with blunt abdominal trauma, the decrease in base deficit is associated with bleeding in around 65% of the cases and was the most important predictor of the need for laparotomy (odds ratio 5.1).21,22
Mutschler et al. used the BD to develop a new classification of hypovolemic shock, reassessing the proposals in the ATLS that shows deficiencies in the clinical correlation. This trial showed a good correlation between the level of shock, transfusion requirement, mortality and base deficit.23
BD is associated with mortality; when combined with lactate, it predicts the mortality with a sensitivity of 80% and a specificity of 58.7% (BE<−6mmol/L). In critically ill patients, BD and/or lactate are used to screen for ICU admission and mortality outcomes.24
Changes in base deficit that are not related to lactic acidosis do not imply mortality.25
Time is a key factor when analyzing BD as compared to lactate values. These biomarkers change early in a parallel and proportional manner to the extent of the primary injury – the hypovolemic shock.
DiscussionIn our case, an elevated lactate value was observed (6.3mg/dl) with adequate clearance (15%/h) resulting in a value of 2.5mg/dl after 12h, despite the prolonged extracorporeal circulation. Base deficit exhibits a similar behavior in terms of the literature reviewed. The requirement for vasopressor and inotropic support is consistent with the tendency of these biomarkers.
In trauma and cardiovascular surgery, various authors agree that the initial lactate value is a measurement of the extent of the trauma and its early clearance at 6 and up to 12h. Lactate levels allow for an evaluation of the resuscitation strategy, the patient's physiological response and an independent determination of the mortality during the first 48h.
With regards to the group of normotensive patients, the information is inconclusive and apparently its analysis is beneficial to detect occult hypoperfusion in the subgroup of patients over 65 years old. However, further studies are needed.
Cardiovascular surgery is an interesting model because it comprises two aspects: it involves non-septic patients and patients exposed to major surgery. The behavior is similar to trauma patients. Clearance is up to 12h and allows discrimination of the possibility for any type of surgical re-intervention. Studies agree that base deficit provides information about the effective circulating volume, oxygen debt and patient mortality.
ConclusionsIn trauma and cardiovascular surgery, lactate and base deficit are biomarkers that should be measured at a very early stage and serially. They represent an independent predictive factor for mortality of trauma patients in the first 48h.
Likewise, the base deficit allows for early staging of patients that present in a state of shock and for determining with a high degree of probability the potential need for blood products or mass transfusion.
Further studies are needed in normotensive patients.
FundingResources own authors.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Sabogal CEL, Riveraa AFC, Higuerab AJ. Lactato y deficit de bases en trauma: valor pronóstico. Rev Colomb Anestesiol. 2014;42:60–64.