Ensuring Safe Surgery is a problem of great interest in public health. Bleeding is one of the most significant predictors of intraoperative outcomes. Visual estimation is the most frequently practiced method, although it is imprecise and may over or underestimate blood loss.
ObjectivesTo determine the correlation between visual estimation and the actual volume of blood soaked in surgical absorbent material, by a group of anaesthetists in the city of Cartagena. Also, to establish the determinants of the correlation between estimated and actual volumes in the perioperative period.
MethodsObservational study designed to estimate the correlation between visual estimation of blood loss, using photographs of gauze pads and sponges impregnated with different volumes of blood, and the actual extent of perioperative bleeding. The study sample was drawn from members of the Bolivar Anaesthesia Society, including subjects with different levels of training and experience (41 anaesthetists, 15 residents). Each participant was requested to estimate the volume of blood content (ml) in gauze pads and surgical sponges impregnated with blood, based on high-resolution photographic images. To estimate the agreement coefficient the intraclass correlation was used, and to identify factors associated with the accuracy of the estimate, a logistic regression analysis was performed. The visual estimate was considered adequate when it differed less than 10% compared to the actual known volume.
ResultsThe visual estimate was the method of choice used by 100% of the participants to determine the extent of perioperative bleeding. However, its correlation with the actual volume of blood is suboptimal and visual estimates of the same volume of blood by different subjects were very heterogeneous (ICC: 0.582, 95% CI 0.28–0.74). A tendency to overestimate bleeding among participants using visual estimation (65.2%) was observed. The logistic regression analysis identified the level of training (OR 1.76, 95% CI 1.04–2.969, P=0.033) and volumes greater than 75ml of whole fresh blood in the absorbent material (OR 1.55, 95% CI 1.04–2.32, P=0.029) as independent determinants of agreement.
ConclusionsVisual estimation is suboptimal as a method for determining perioperative bleeding. The objective measurement must be the method of choice in this clinical setting.
Garantizar prácticas quirúrgicas seguras es un problema de gran interés en salud pública. La hemorragia es uno de los predictores más significativos de desenlaces intraoperatorios. El método más usado para determinarlo es la estimación visual, pese a que es impreciso y puede sobre o subestimar las pérdidas sanguíneas.
ObjetivosDeterminar la concordancia entre la estimación visual y el volumen de sangre real impregnada en material absorbente quirúrgico, por un grupo de anestesiólogos de la ciudad de Cartagena. Establecer los factores determinantes de la concordancia entre los volúmenes estimados y reales en el periodo perioperatorio.
MétodosEstudio observacional analítico diseñado para determinar la concordancia entre la estimación visual de la hemorragia, utilizando fotografías de compresas y gasas impregnadas con diferentes volúmenes de sangre, y la magnitud real de la hemorragia perioperatoria. La muestra de estudio fue extraída de los miembros de la Sociedad Bolivarense de Anestesiología, incluyendo a sujetos de diferente grado de formación y experiencia (41 anestesiólogos, 15 residentes). Se solicitó a cada participante que estimara el volumen de sangre contenido (ml) en gasas y compresas quirúrgicas impregnadas con sangre, basándose en imágenes fotográficas de alta resolución. Para la estimación de la concordancia se utilizó el coeficiente de correlación intraclase y para identificar los factores asociados a la precisión de la estimación se realizó un análisis por regresión logística. La estimación visual se consideró adecuada cuando difería menos de ± 10 ml con respecto al volumen real conocido.
ResultadosLa estimación visual fue el método de elección utilizado por el 100% de los participantes para determinar la magnitud de la hemorragia perioperatoria. Sin embargo, su concordancia con los volúmenes reales de sangre es subóptima y las estimaciones visuales de los sujetos para un mismo volumen de sangre muy heterogéneas. (CCI: 0,582; IC: 95%:0,28-0,74), se observó una tendencia a la sobrestimación de la hemorragia entre los participantes al utilizar la estimación visual (65,2%). El análisis de regresión logística identificó como determinantes independientes de la concordancia el nivel de formación (OR 1,76; IC95%: 1,04-2,969; p = 0,033) y volúmenes superiores a 75 ml de sangre fresca total en el material de absorción (OR 1,55; IC 95%: 1,04-2,32; p = 0,029).
ConclusionesLa estimación visual es un método subóptimo para la determinación de la hemorragia perioperatoria. La medición objetiva del sangrado debe ser el método de elección en este escenario clínico.
It is estimated that 234.2 million major surgical procedures (95% CI 187.2–281.2) are performed every year, which means that one out of every 25 people undergoes major surgery. This large volume of interventions is associated with a high rate of complications and deaths, which are preventable in half of the cases. Consequently, ensuring safe surgical practices is a matter of great concern in public health.1
Bleeding is one of the most significant predictors of intraoperative outcomes; in paediatric patients, it is one of the main causes of perioperative mortality2; in cancer patients, it is a predictor of disease progression as well as mortality; and in all surgical patients it predicts the need for red blood cell transfusion, which is in itself associated with higher mortality.3 Different methods have been used to estimate intraoperative bleeding, including, among others, blood volume measurement, blood collection for weighing; weighing of surgical drapes, absorbent materials and other utensils containing blood from the surgery; use of colorimetric reactions for blood detection; and haemorrhage estimation based on haemoglobin or oxygen saturation before and after surgery.3,4 However, the method most frequently used is visual estimation, despite its inaccuracy and the potential to under or overestimate blood losses.4
The primary objective of this study was to determine correlation between visual estimation by a group of anaesthetists in the city of Cartagena and actual blood volume impregnated in absorbent surgical material. The secondary objective was to establish determining factors of agreement between estimated and actual volumes in the perioperative period in this population.
MethodsEthical considerationsThis work was conducted pursuant to the ethical standards set forth under Resolution 008430 of 1993 issued by the Colombian Ministry of Health. This project falls under the No Risk Research category according to Article 10 (a) of the resolution mentioned above.
The names of the interviewees were not recorded in order to protect their identities.
The institutional Ethics Committees endorsed the project.
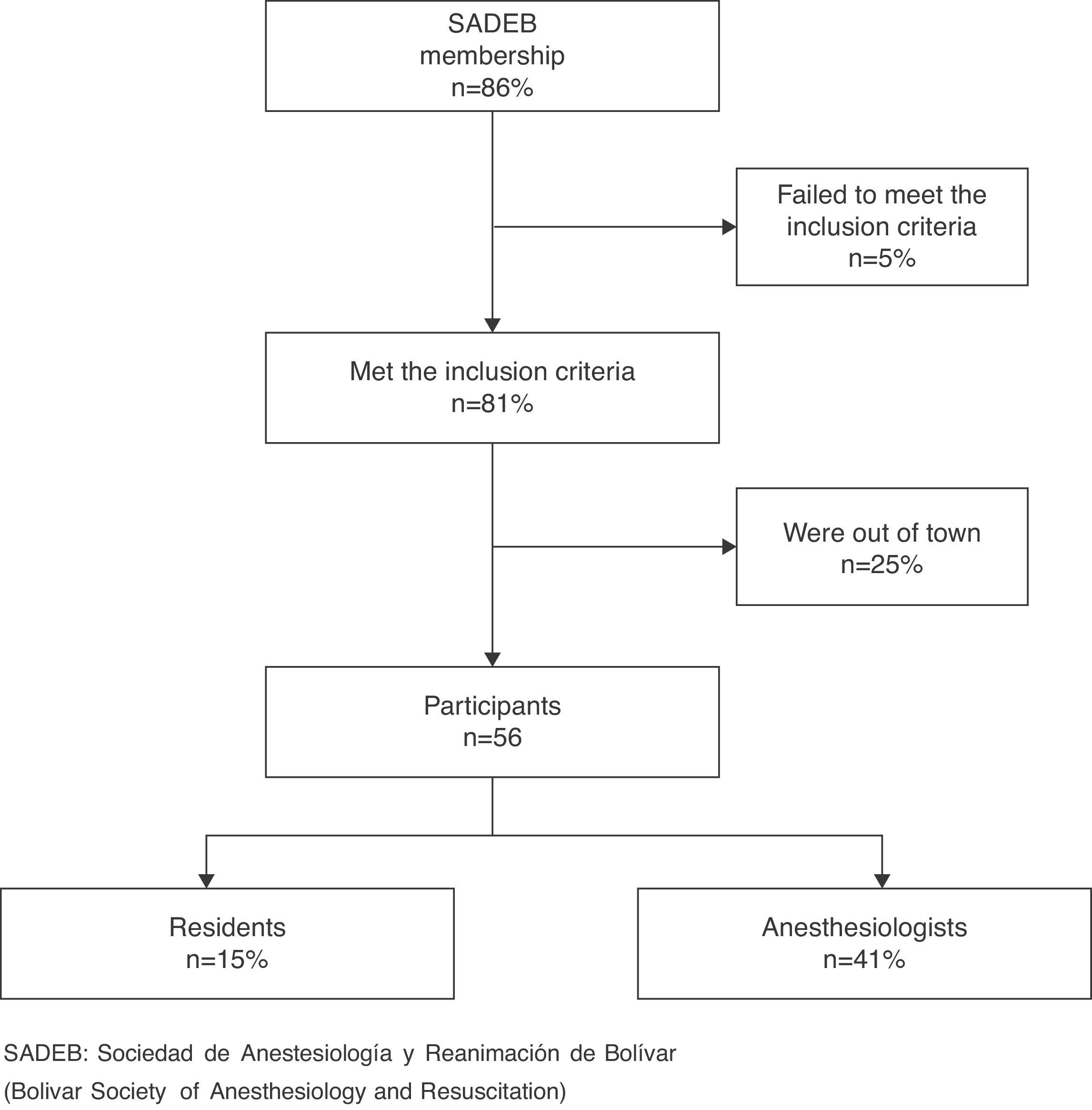
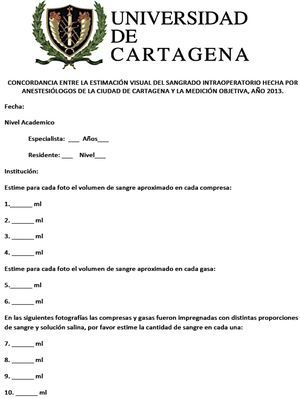
Study design and populationObservational correlational studyAll of the anaesthetists and anaesthesia residents, members of the Anaesthesia Society of Bolívar (SADEB) in July 2013, were asked to participate. Retired specialists with more than 2 years of absence from practice or specialists living outside the city were excluded (Fig. 1). They were each asked to give a visual estimate in millilitres (ml), using high definition photographs, of ten different blood volumes impregnated in surgical absorbent material. The assessment was conducted individually and anonymously by one single interviewer during a minimum time period of 10min; each interviewee was asked to observe each photograph for at least 1min. Data were collected from anaesthetists and anaesthesia residents practicing in the public and private intermediate and high complexity hospital network in the city of Cartagena.
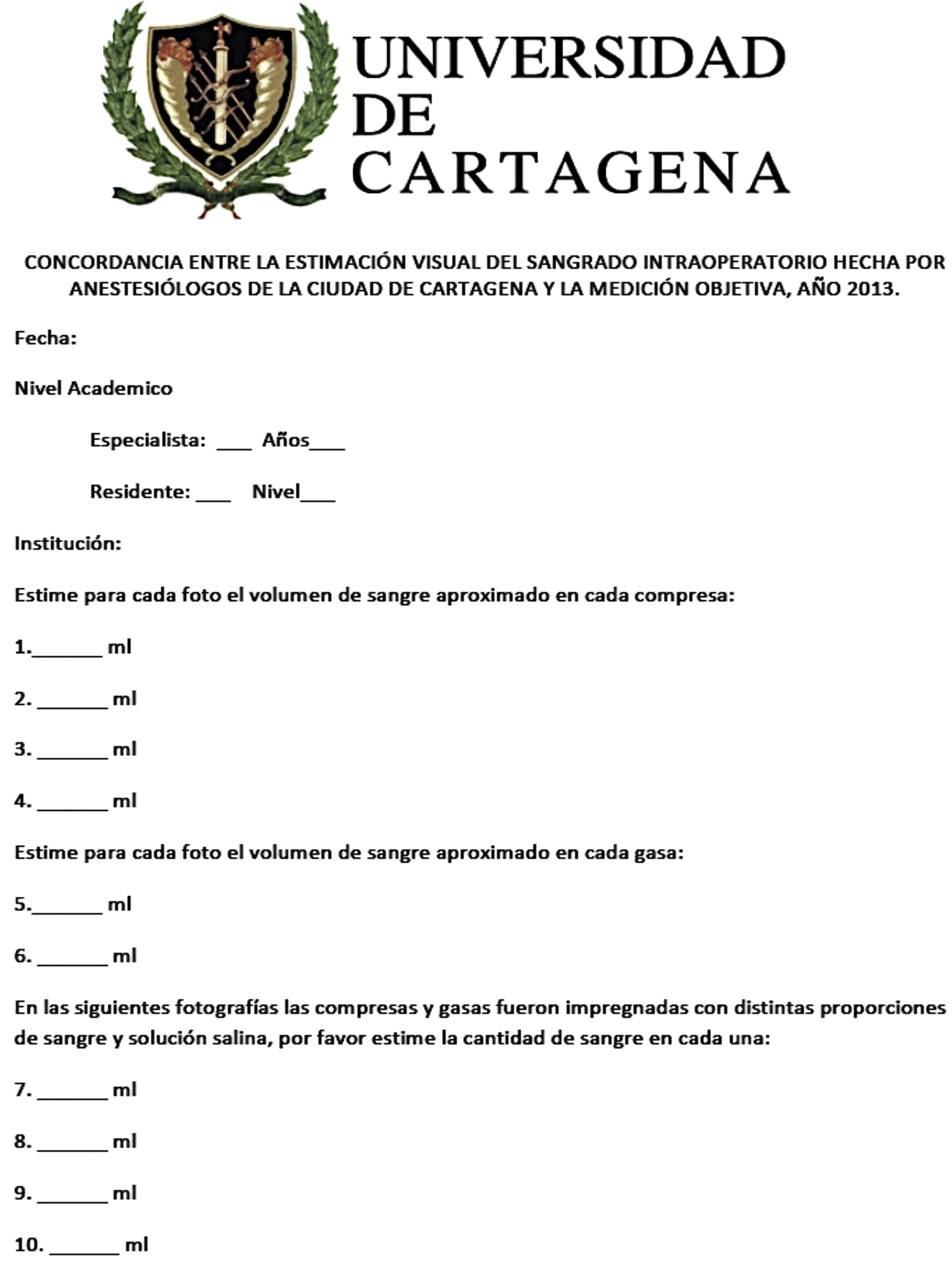
Assessment toolPhotographsThe surgical absorbent materials used were gauze pads (7.5cm×7.5cm) and sponges (8cm×18cm). Seven sponges were soaked, four of them in whole fresh blood (WFB) with 100ml, 75ml, 50ml and 25ml, and the remaining three were soaked in mixed blood and 0.9% saline solution (NSS), as follows: 75ml WFB+25ml NSS; 50ml WFB+50ml NSS and 25ml WFB+75ml NSS. Also, three gauze pads were used, two with WFB (10ml and 5ml, respectively) and one with an admixture of WFB and NSS (WFB 5ml+NSS 5ml). The photographs were taken with a high-resolution camera by the same operator, at the same capture distance (60cm), immediately after soaking the absorbent material. The photographs were printed in a digital format, using the same sizes of the gauze pads and sponges to enhance the simulation effect.
InterviewThe interview included level of training and years of experience. The photographs were numbered and allowed room for the interviewees to record their visual estimation (See Annex 1).
Statistical analysisThe data were analysed using the SPSS statistical software package version 15.0 (IBM© software).
The mean (SD) and the median (range) were used for quantitative variable description and box diagrams were used for their graphic representation, when appropriate. Categorical variables were expressed as absolute numbers and percentages. The Student's t test was used for comparing the means of independent samples between the groups. The Kolmogorov–Smirnov test was used for evaluating the normal distribution of the quantitative variables.
The correlation analysis was conducted using the intraclass correlation coefficient (ICC), comparing actual values with interviewee estimations. The correlation level was considered adequate at ICC>0.75.5
Additional correlation analyses were made by subgroups as a function of training level (anaesthetist–resident), years of experience (>5 years), and the WFB/NSS admixture.
A multivariate logistic regression (ENTER METHOD) was used for identifying predictors of agreement between visual estimations and actual values, including level of training, WFB/NSS admixtures, actual volumes (>75ml) and years of experience of the interviewees as independent variables. Agreement was defined as occurring when the differences between estimated and actual values were not greater than ±10ml in the sponges and ±2ml in the gauze pads.
ResultsParticipant characteristicsUltimately, 56 individuals participated voluntarily in the study (Fig. 1). Years of experience of anaesthesia specialist physicians ranged between 1 and 35, with a mean of 10 years; and the experience of the residents ranged between 3 months and 3 years, with a mean of 2 years and 2 months. The correlation analysis was performed with a total of 560 estimates.
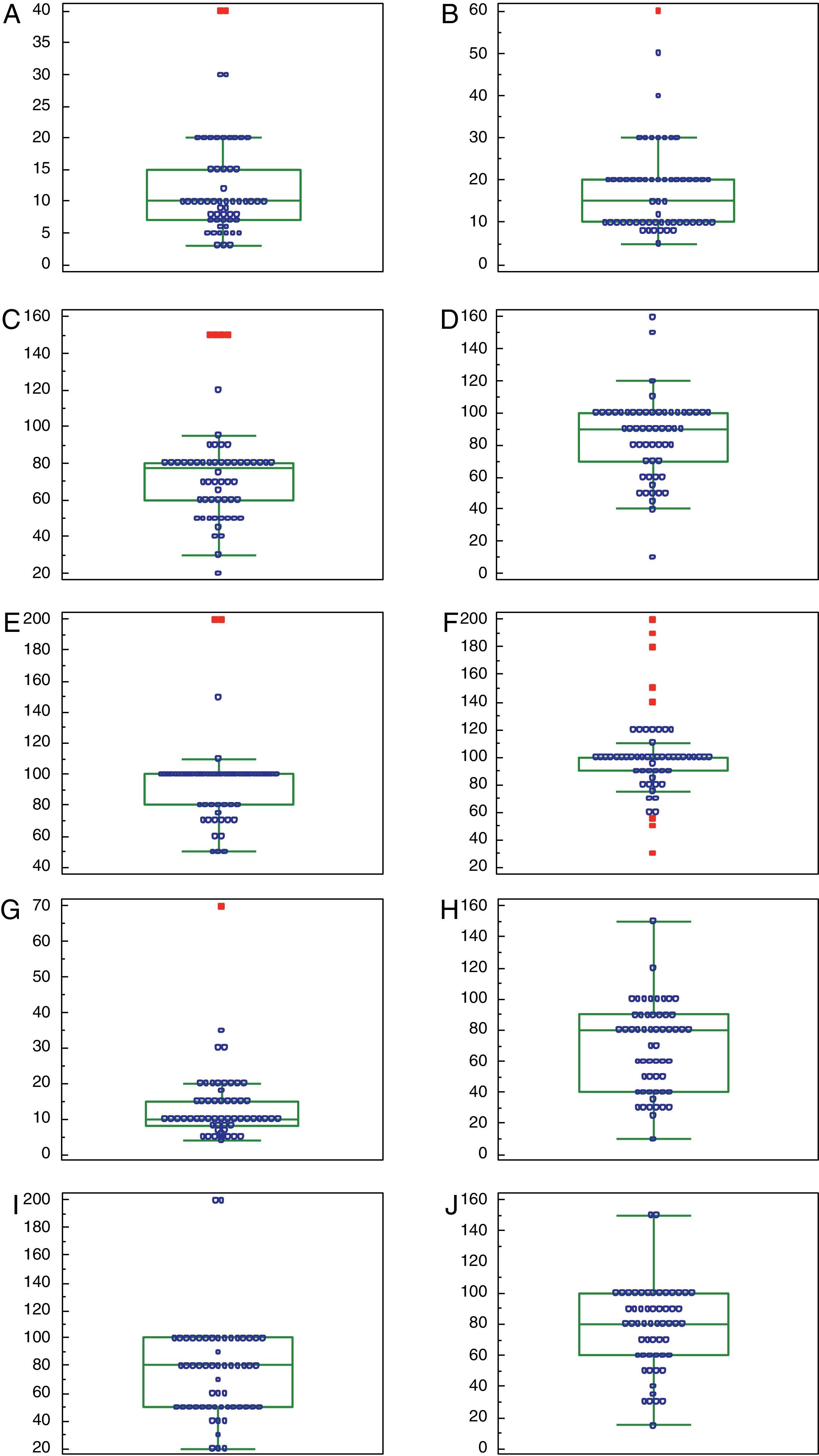
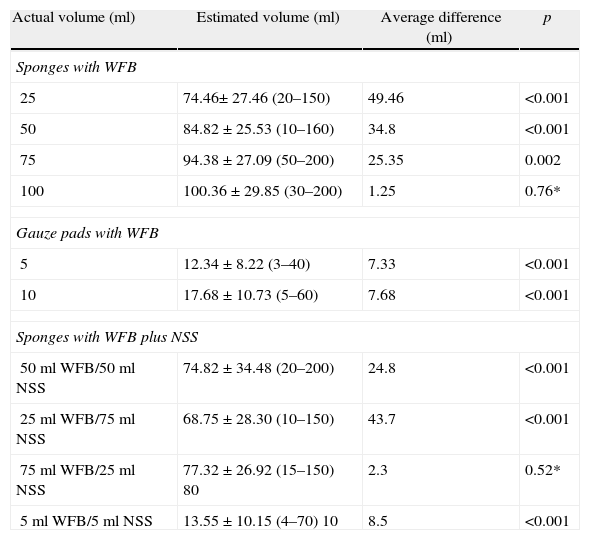
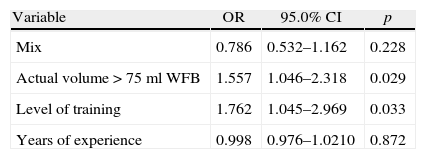
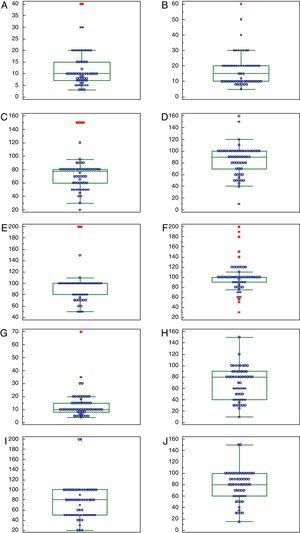
Visual estimation accuracyAgreement was observed in 153 estimates (27.3%), underestimation in 42 cases (7.5%) and overestimation in 365 opportunities (65.2%). A tendency to overestimate was also observed when comparing the mean of the estimated values with the actual amount of blood in the sponges and gauze pads; however, these mean differences between estimated and actual values were smaller when the actual volume was greater than 75ml (Table 1). The considerable heterogeneity of the estimated values in each of the 10 determinations suggests little accuracy of the visual method (Fig. 2). The logistic regression analysis identified the level of training of the anaesthetist (OR 1.76, 95% CI 1.04–2.969; p=0.033) and amounts greater than 75ml of WFB in the soaked material (OR 1.55, 95% CI 1.04–2.32; p=0.029) as the only independent predictors of agreement between the estimated and actual values, above the years of professional experience or the absence of NSS in the absorbent material (Table 2).
Distribution of estimated vs. actual blood loss.
| Actual volume (ml) | Estimated volume (ml) | Average difference (ml) | p |
| Sponges with WFB | |||
| 25 | 74.46±27.46 (20–150) | 49.46 | <0.001 |
| 50 | 84.82±25.53 (10–160) | 34.8 | <0.001 |
| 75 | 94.38±27.09 (50–200) | 25.35 | 0.002 |
| 100 | 100.36±29.85 (30–200) | 1.25 | 0.76* |
| Gauze pads with WFB | |||
| 5 | 12.34±8.22 (3–40) | 7.33 | <0.001 |
| 10 | 17.68±10.73 (5–60) | 7.68 | <0.001 |
| Sponges with WFB plus NSS | |||
| 50ml WFB/50ml NSS | 74.82±34.48 (20–200) | 24.8 | <0.001 |
| 25ml WFB/75ml NSS | 68.75±28.30 (10–150) | 43.7 | <0.001 |
| 75ml WFB/25ml NSS | 77.32±26.92 (15–150) 80 | 2.3 | 0.52* |
| 5ml WFB/5ml NSS | 13.55±10.15 (4–70) 10 | 8.5 | <0.001 |
Quantitative variables: mean plus/minus its standard deviation (range). Average difference: estimated haemorrhage – actual volume. ml, millilitres; WFB, whole fresh blood; NSSN, normal saline solution.
Box diagrams of visual estimations for each case.
(A) Visual estimations of gauze pads with 5cc of blood. (B) Visual estimations of gauze pads with 10cc of blood. (C) Visual estimations of sponge with 25cc of blood. (D) Visual estimations of sponge with 50cc of blood. (E) Visual estimations of sponge with 75cc of blood. (F) Visual estimations of sponge with 100cc of blood. (G) Visual estimations of sponge with 5cc of blood and 5cc of saline solution. (H) Visual estimations of sponge with 25cc of blood and 75cc of saline solution. (I) Visual estimations of sponge with 50cc of blood and 50cc of saline solution. Visual estimations of sponge with 75cc of blood and 25cc of saline solution.
Logistic regression analysis of determining factors of agreement.
| Variable | OR | 95.0% CI | p |
| Mix | 0.786 | 0.532–1.162 | 0.228 |
| Actual volume>75ml WFB | 1.557 | 1.046–2.318 | 0.029 |
| Level of training | 1.762 | 1.045–2.969 | 0.033 |
| Years of experience | 0.998 | 0.976–1.0210 | 0.872 |
Mix, whole fresh blood mixed or not with normal saline solution; Level of training: anaesthetist – resident. Years of experience >5 years. WFB, whole fresh blood.
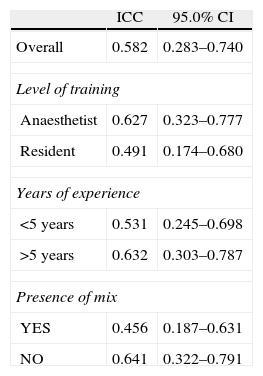
The analysis showed, overall, moderate correlation between estimated and actual values (ICC 0.582, 95% CI 0.28–0.74). The correlation did not improve when the results were analysed as a function of level of training, years of experience (>5 years) or absence of NSS in the soaked material (Table 3).
Intraclass correlation coefficient for the estimated and actual volumes soaked in the surgical absorbent material.
| ICC | 95.0% CI | |
| Overall | 0.582 | 0.283–0.740 |
| Level of training | ||
| Anaesthetist | 0.627 | 0.323–0.777 |
| Resident | 0.491 | 0.174–0.680 |
| Years of experience | ||
| <5 years | 0.531 | 0.245–0.698 |
| >5 years | 0.632 | 0.303–0.787 |
| Presence of mix | ||
| YES | 0.456 | 0.187–0.631 |
| NO | 0.641 | 0.322–0.791 |
ICCI, intraclass correlation coefficient; CI, confidence interval; Overall, refers to all estimations performed; Presence of mix, refers to whole fresh blood mixed or not with normal saline solution.
Visual estimation is the method most widely used for determining intraoperative haemorrhage, despite several studies that have found it to be lacking in accuracy, precision and reproducibility.4 The majority of the studies are conducted in the field of obstetrics and gynaecology, considering the huge impact of post-partum bleeding on morbidity and mortality. The different studies show that visual estimation either overestimates or underestimates haemorrhage.6
In this study, visual estimation was used by 100% of the participants and it was found to be moderately correlated with the actual measurement, with no evidence of improvement as a function of level of training, years of experience or absence of distractors such as saline solution.
Rubio et al. analysed the correlation between visual estimation and actual measurement of intrapartum blood volume collected in women with normal deliveries in Bogotá. There was great estimation variability, with acceptable correlation that worsened as blood volumes increased. In their results, the trend was towards underestimation, but it is important to consider that the values assessed in their study were much higher (541.4ml in average).7
In the distribution analysis and in the analysis of the mean difference between the estimate and the actual value, it was interesting to find a marked trend towards overestimation (65.2%), a discrepancy which diminished as volumes increased (>75ml), similar to what Larsson8 and Yoong9 found using volumes between 25 and 200ml. The quality of visual estimation was also determined by the level of training of the observer (anaesthetist), but not so by the years of experience. Casquero-León in Lima, Perú, found a weak correlation between blood loss estimated visually and calculated intrapartum haemorrhage in nulliparous patients undergoing Caesarean section, with overestimation when intrapartum haemorrhage was less than 500ml, and underestimation when it was greater than 1.000ml.10 Similar results were obtained by Cheerranichanunth and Poolnoi, in Thailand.11
The graphic analysis of estimation distributions shows the great heterogeneity of the results and the inaccuracy of visual estimation.
Considering the findings of this research, the great limitation and inaccuracy of visual estimation as a method for determining bleeding are confirmed. Also, considering the huge impact of haemorrhage on surgical outcomes, efforts to improve it must be a priority for the healthcare team,12 with a focus on improving visual estimation by means of training and education13,14 or introducing quantitative measurement tools to measure bleeding objectively and accurately.3
One of the limitations of this study was the sample size, which does not allow extrapolation of the data beyond the local setting. Second, the estimation was done using photographs and not in real circumstances when the anaesthetist may occasionally make a subjective determination of the weight of the material.
Despite the importance of this issue in the surgical field, it had not been approached locally, and this work shows evidence of the need to use more accurate methods for measuring intraoperative blood loss.
ConclusionsVisual estimation performed by a group of anaesthetists in the city of Cartagena was shown to have poor correlation with the actual measurement of blood impregnated in the surgical absorbent material. There is a need to use more accurate methods for the determination of intraoperative haemorrhage. Developing training and education programmes on the subject is an option, considering that there was a discreet improvement in correlation with the level of training, although it continued to be poor.
FundingNone.
Conflict of interestNone.
The authors acknowledge all the seconded members of the Sociedad de Anestesiología y Reanimación de Bolívar for their voluntary contribution in this research.
And to all those people who contributed to the development and success of the project.
Please cite this article as: De La Peña Silva AJ, Delgado RP, Barreto IY, De La Peña Martínez M. ¿E útil la estimación visual en la determinación de la magnitud de la hemorragia perioperatoria?: Un estudio de concordancia en anestesiólogos de hospitales de mediana y alta complejidad en Cartagena, Colombia. Rev Colomb Anestesiol. 2014;42:247–254.