Pain continues to be one of the most frequent complaints in clinical centers. Consequently, understanding gender differences in relation to pain is important and critical for the clinical management of patients by the different healthcare services. Pain in patients of different gender is usually treated in the same way; however, there are several gender-associated factors involved in the management of pain, which sometimes are not taken into consideration in clinical practice.
ObjectiveTo describe the differences between men and women as far as pain is concerned, taking into consideration anatomical, physiological, neural, hormonal, psychological, social and cultural factors in the practice of anesthesia.
MethodologyA non-systematic review was undertaken using the key words in the Pubmed/Medline, Science Direct, OVID, SciElo databases.
Results and conclusionsDifferences between men and women when it comes to pain involve anatomical, physiological, neural, hormonal, psychological, social and cultural factors. When examining those factors, it is found that women report pain more frequently, and have a lower threshold for pain than men. They usually complain more of muscle–skeletal, neuropathic, electrical shock and temperature-related pain, but respond better to opioids, in particular κ receptor-binding opioids.
El dolor en la clínica sigue siendo una de las mayores causas de consulta en centros clínicos, por lo tanto comprender las diferencias de sexo en cuanto al dolor se refiere es importante y trascendental para el manejo clínico del paciente en los diferentes servicios. La presentación del dolor en pacientes de diferente sexo suele tratarse de la misma manera, aunque son varios los factores involucrados en el manejo del dolor en relación al sexo que algunas veces no son tenidos en cuenta en la práctica clínica.
ObjetivoDescribir las diferencias entre hombre y mujer en relación al dolor, desde distintos aspectos tales como factores anatómicos, fisiológicos, neurales, hormonales, psicológicos y socioculturales en la práctica anestésica.
MetodologiaCon las palabras clave se realizó una revisión no sistemática en bases de datos (Pubmed/Medline, Science Direct, OVID, SciElo).
Resultados y conclusionesLas diferencias entre hombre y mujer respecto al dolor involucran factores anatómicos, fisiológicos, neurales, hormonales, psicológicos y socioculturales. Al evaluar estos factores se concluye que la mujer reporta con mayor frecuencia dolor y presenta un umbral más bajo de dolor que los hombres, refiriendo más dolor musculoesquelético, neuropático, por electricidad y por presiones de temperatura. Aun así, responde mejor a los opioides, en especial el receptor κ.
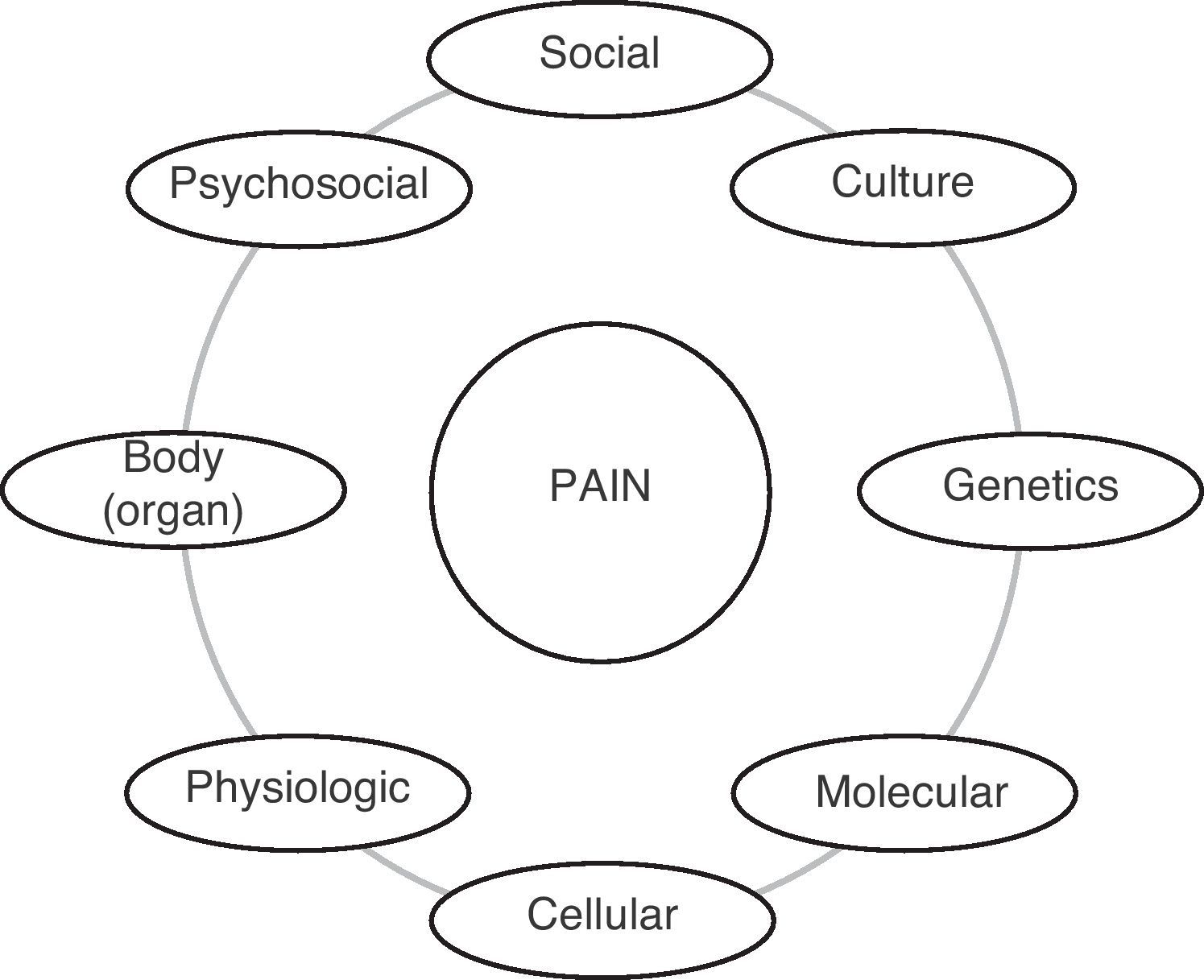
In clinical practice, pain continues to be one of the most frequent complaints in clinical centers.1 Consequently, understanding gender differences in relation to pain is important and critical for the clinical management of patients by the different services. Pain is the most uncomfortable physical sensation that an individual may experience. According to the International Association for the Study of Pain (IASP), pain is considered as an “unpleasant sensory and emotional sensation resulting from physical damage”. In 1842, Dr. Crawford Williamson Long, in Danielsville, Georgia, was the first to control pain when he used what today is known as anesthesia (ether) during the removal of neck cyst in a boy.2 Two years later, Horace Wells, a dentist, began to use nitrous oxide as anesthetic,3 after witnessing its use in performance shows. He was struck by the state of euphoria, violence or disinhibition caused by the gas. At one point, one of the volunteers was injured while under the effect of the gas, and Dr. Wells observed that there was no pain response. Based on this observation, he performed a successful tooth extraction in a friend under the effect of the gas. Ever since that time, man has had an interest in developing substances and methods to alleviate pain. In understanding the differences between men and women, it is important to understand the multiple factors involved in pain, including anatomical, physiological, neural, hormonal, psychological, social and cultural factors (Fig. 1).
Epidemiological studies have shown that women and men respond differently to pain. However, it is important to remember that the terms sex and gender are distinct and critical when it comes to assessing a patient. According to the Institute of Medicine (IOM), sex is “the classification of humans as man or woman in accordance to their reproductive organs and the function assigned by the chromosomal complement”, while gender refers to the “individual's own representation as man or woman, or the way in which the individual responds to social institutions based on the gender presentation.”4
Pain studies conducted in humans regarding the relationship between pain and several aspects such as brain function, psychological and physical factors, variation of the menstrual cycle and the influence of hormones in men, have shown several gender differences.
Anatomical, neural and physiological factorsAs far as the brain is concerned, there are structural differences of the various components of the cerebral cortex between the male and the female brain. Neuronal density is greater in the male brain, but the cortical thickness is the same.5 In spite of this, there are more neuronal processes taking place in the female brain when compared with the male brain, which enhanced the ability to perform multiple tasks.
Other studies conducted in men and women, who were subjected to some form of thermal stimulus, determined that some of the brain areas lighted up in both male and female brains,6 but there were others that only lighted up in the male brains.7 In women, there was greater activation of the contralateral frontal cortex, the contralateral insula and the thalamus, suggesting dimorphism in response to pain.8–10 When another type of test was used – a psychophysical test of rectal examination to demonstrate discomfort after applying noxious stimulation of the sigmoid colon in healthy men and women compared to patients with irritable bowel syndrome,11 women showed greater discomfort to the rectal examination than men. Additionally, it was observed that repetitive stimulation triggered generalized tenderness in women, suggesting that women are more vulnerable to the development of certain coexisting pain conditions.
Hormonal aspectsIn women, the menstrual cycle and its variations during the 28-day period (in average) are associated with the degree of pain.12 It is important to remember that there are differences among women in terms of regular or irregular menstrual cycles, depending on the level of estrogen which protects against pain during the first 7 days, and the level of progesterone during the remaining days, with the respective levels of follicle-stimulating hormone (FSH) and luteinizing hormone (LH). In a study conducted in healthy subjects under 60, the researchers found that women reported more pain at lower thresholds and less tolerance to any noxious stimulus, when compared to men.13 Some forms of pain are more common in women, including the joints, in particular temporomandibular joint disorders.14 In women, the pain threshold is lower during menstruation,15 but when progesterone levels are low and estradiol levels are high, women are not very different from men in terms of the threshold of pain.16 In fact, there is a directly proportional relationship between the pain threshold and estradiol levels in women, mainly because high estrogen levels increase the number of opioid receptors, activating a state of analgesia, unlike what happens when estrogen levels are low and there is a reduction in the number of opioid receptors in areas of the brain associated with analgesia such as the thalamus, the nucleus accumbens and the amygdala – which was associated with hyperalgesic responses.17
In men, the effects of estradiol are several, including its significant role in pain, its great anti-inflammatory action, which is evidenced in the form of protection in particular in acute coronary syndrome, as well as in other disorders. However, the most important benefit is observed in high-performance athletes.18 As far as muscle–skeletal pain is concerned, it is an economic and medical problem in epidemiological terms in the whole world. It is more frequent, more severe and longer lasting in women than in men,14 and this could be related to the incidence of autoimmune diseases in women19 like rheumatoid arthritis, systemic lupus erythematosus, ankylosing spondylitis, and even joint pain and fibromyalgia.20,21 Muscle inflammation is induced by exercise, and men have a higher anti-inflammatory response than women, and this may explain better adaptability to sports, considering that men participate more in sports activities such as football, basketball, volleyball, cycling, jogging, etc. The evidence suggests that the prevalence of pain in women increases during puberty and multiple problems of pain are common in girls during that time22; moreover, women experience higher levels of pain in catastrophic situations.23
Psychological, social and cultural aspectsHormonal variations, puberty, reproduction and the menstrual cycle have an effect on the threshold and the perception of pain. In general, women have a lower threshold and are less tolerant to noxious stimuli.13 Men report greater tolerance associated with a higher threshold in the presence of a female examiner – either a physician or a nurse24; the opposite is true in women, whose pain thresholds drop when they are examined by attractive men, and hence their reports of higher pain levels.25 There have been more examination testing done in animal models than in man, but many of the data are consistent. Women tend to seek medical help because of pain more often than men, among other things because they report higher levels of pain when seen by a male physician.
There is a direct relationship between aging and a lowering of the pain threshold,26,27 which becomes more easily activated. Likewise, with aging, the difference between men and women in terms of their threshold of pain is reduced.28 In situations of social catastrophe, adaptation to clinical pain has been shown to worsen, with increased sensitivity to experimental pain.29–31 Based on the hygiene hypothesis, the threshold of pain would drop for the individuals who do not feel affected by a threatening situation. For this reason, people who fight frequently (e.g. boxers) usually feel less pain than others.
Molecular aspectsEpidemiologically, there are certain differences in opioid-mediated analgesia between men and women32–34 because of the type and number of receptors present in the central nervous system. Animal studies have shown differences in opioid-mediated analgesia, and this was an important starting point for studies in humans. In a study with 4300 subjects who were prescribed morphine for post-operative pain, higher levels of pain were found in women despite the use of high amounts of morphine.33
In terms of non-drug-induced analgesia, there are two possibilities: stress-induced analgesia through the action of cortisol, the most important stress hormone, that might increase the pain threshold and tolerance; however, no significant difference has been found between the two sexes.35,36 The other possibility is exercise-induced analgesia where pain thresholds and tolerance increase in women when going from a pre-exercise to a post-exercise state; however, in men, the threshold does not change between one state and the other. Pain assessment in both sexes improves after exercising.37 In terms of neuropathic pain, there are different etiologies, including surgical interventions such as mastectomy, C-section, amputation, heart surgery, hernia repair, cholecystectomy and thoracotomy, some of which are more frequently performed in women (mastectomy and C-section).38 One study showed a prevalence of 52% in women, with no clear predominance of this type of pain by gender.39,40 Understanding neuropathic pain, its diagnosis and treatment, requires knowledge of the pathophysiology, and it is important to provide a rational prescription based on a review of the drugs that may be used for this form of pain included in the mandatory health plan: tramadol, morphine, gabapentin, carbamazepine, amitriptyline, pregabalin, valproic acid, duloxetine, venlafaxine.38
The other side of the coin is drug-induced analgesia, better studied in animals than in humans. The medical anesthesiology references focuses on the receiver μ-opioid similar to morphine and its derivatives, although some studies have also focused on the there are the others focused on the agonist κ-opioid receptor. Some initial studies showed differences in morphine metabolism, but later studies concluded that there are no gender differences in terms of morphine metabolism to morphine-6-glucoronide.41 The response of both men and women to analgesics is quite complex, given their multiple interactions. Of different studies, some report that both sexes consume equal amounts of opioids, while others reveal that women consume considerably less amount of opioids than men.42 These results are important for clinical application in surgery as well as in outpatient settings. Women are more closely related to opioids since they act on the agonist κ-opioid receptor, with greater analgesic activity in women.43 Women show a higher response to morphine in pain caused by electric shock or cold pressure.44 In terms of the pharmacological response to non-opioids, including NSAIDS (cyclooxygenase inhibitors) like ibuprofen, there is no evidence of significant gender differences.45 Regarding anesthesia and its influence on the control of post-operative pain, it has been found that after using inhaled anesthetics such as sevoflurane and desflurane, or intravenous anesthetics like propofol, there are no variations in pain scores 24h after surgery.46 However, women do report more post-operative effects such as nausea, vomiting and headache, together with longer recovery time.
DiscussionAll services need to assess several aspects relating to pain, and this is even more important in pre-anesthetic consultations and pain clinics. There is a long-standing belief that men and women respond equally to pain, and despite the knowledge gained regarding the human physiology, pain therapy provided to men and women is the same. Women activate exclusive areas of the CNS, perhaps as a result of evolution and social and cultural influences, considering that women are more sensitive to events involving them. As far as rectal pain is concerned, it may be associated with female sense of decency in the presence of men. However, it is important to consider the abundant innervation of the perianal area in women when it comes to the determination of that form of pain. In the case of muscle–skeletal pain, it is more frequent in women in research and in the clinical practice, as a result of autoimmune diseases, which are found to be more prevalent in women in pre-anesthetic consultations. Pain in women is associated with hormonal changes, which explains why in situations of severe pain, such as delivery, there is a relationship with hormonal changes, in particular with the release of enkephalins, endorphins and dynorphins. From the social and cultural perspective, women have been closely linked to the most sensitive side of mankind and, for this reason, tragic events may lower their threshold of pain and increase their vulnerability. Women experience more pain resulting from electric shock or thermal pressure, although this is debatable because it could be due to the social effects mentioned previously. It is important to note that although women report more pain, they respond better to opioid-mediated analgesic therapy, although these drugs may induce dizziness and vomiting episodes at times. As far as post-operative pain is concerned, a study showed that the combination of dipirone plus meperidine reduces by 50% the need for opioids, with less adverse events. The values reported in this study47 are much higher than those reported in a study conducted in Paris.48 This is true for pain control in both men and women. This study of two groups, the group with the intervention (meperidine 0.5mg/kg) and the control group (meperidine 1mg/kg) showed values of 24% and 21.05%, respectively, in male patients, out of a total of 50 and 57 patients in the two groups, suggesting better results with a lower concentration of opioids. In another study49 comparing morphine–bupivacaine vs. hydromorphone–bupivacaine in order to assess tolerability to epidural analgesia and adverse effects resulting from the opioid used, no statistically significant differences were found in terms of the presence of nausea, vomiting, sedation, pruritus or urinary retention, described all together as tolerability.50 In spite of this, women tend to report greater discomfort with anesthesia and the use of opioids; for this reason, lowering the burden of opioids becomes a therapeutic option in the treatment of pain, according to the study mentioned above.
ConclusionsThis article shows the most relevant aspects of pain, but there is much more to be learned, and gaining new knowledge could be the goal of the sciences that study pain at clinical and molecular levels. The main findings are that, despite the higher neuronal density in men when compared to women, exclusive areas of the brain are activated in women, suggesting dimorphism in response to pain. Pain is closely associated with hormonal processes, explaining why in women the experience of pain depends in part on the variations of the hormonal cycle. There is a higher relationship between catastrophic situations and pain in women than in men. Women have lower thresholds when it comes to neuropathic pain, pressure pain, electric shock pain, but they respond better to opioids than men with κ-receptor mediation. It is important to assess pain from a multi-disciplinary perspective and not from a single vantage point, considering that medical and scientific experience is constantly adjusting in response to the changes brought about by human evolution.
FundingAuthors’ own resources.
Conflict of interestNone declared.
Please cite this article as: Gutiérrez Lombana W, Gutiérrez Vidal SE. Diferencias de sexo en el dolor. Una aproximación a la clínica. Rev Colomb Anestesiol. 2012;40:207–12.