Valved conduits for surgically reconstructing the outflow tract of the right ventricle have improved the prognosis for certain congenital heart diseases. When they become dysfunctional, transcatheter pulmonary valve replacement is safe and effective.
Clinical findings, diagnostic evaluation and interventionsWe report the case of a 21 years old female patient diagnosed with transposition of great vessels corrected in childhood. After several surgeries, she presents a dysfunction of the right ventricle. In response, a “Melody®” pulmonary valve was implanted percutaneously under deep sedation.
ConclusionThe ideal anesthetic technique for transcatheter pulmonary valve replacement is controversial. There is a debate over the merits of general anesthesia and deep sedation. Each case must be decided on after a careful preoperative evaluation, considering the risk/benefit and patient cooperation. The experience at our center using deep sedation is promising, but we have an alternative plan to convert to general anesthesia if necessary.
Los conductos valvulados para reconstruir quirúrgicamente el tracto de salida del ventrículo derecho han mejorado el pronóstico de ciertas cardiopatía congénitas. Cuando éstos se vuelven disfuncionantes, el remplazo valvular pulmonar transcatéter es eficaz y seguro.
Hallazgos clínicos, evaluación diagnóstica e intervencionesPresentamos una paciente de 21 años, diagnosticada de transposición de grandes vasos corregida en la infancia, que tras varias intervenciones quirúrgicas presenta una disfunción del conducto del ventrículo derecho, por lo que se implanta percutáneamente una válvula pulmonar “Melody®” bajo sedación profunda.
ConclusiónLa técnica anestésica ideal para el recambio valvular transcatéter pulmonar es controvertida, discutiéndose entre la anestesia general y la sedación profunda. Cada caso debe decidirse tras una evaluación preoperatoria cuidadosa, considerando el riesgo/beneficio y la colaboración del paciente. La experiencia en nuestro centro empleando la sedación profunda es prometedora, aunque debemos contar con un plan alternativo para reconvertir a anestesia general de ser necesario.
Valved conduits (VC) are used for the surgical reconstruction of the right ventricle outflow tract1 (RVOT), providing improved prognoses for patients with complex congenital cardiopathies1 such as the transposition of great vessels (TGV). Nevertheless, they tend to calcify and develop stenosis,1 making intervention necessary. In these cases, transcatheter pulmonary valve replacement techniques (tPVR) represents an advance.2 It is an alternative for delaying or avoiding open heart surgery valve replacement (OHSVR) and the technical complexity and morbidity that it implies.3
Clinical caseWe present the case of a 21-year-old female patient who underwent the percutaneous implantation of a “Melody®” pulmonary valve.
Case informationIn the patient's clinical history, we highlight TGV with ventricular septal defect (VSD) and pulmonary stenosis at birth. She underwent an intervention at 5 months of age for a Blalock-Taussig pulmonary-systemic shunt and three year later underwent a Rastelli procedure. She was operated on again for a subaortic obstruction and dysfunction of the VC of the RVOT, corrected previously. She has an automated implantable cardioverter defibrillator (AICD).
Clinical findings, diagnostic evaluation, and interventionsThe preoperative study revealed a class 3 on the New York Heart Association scale. In the right catheterization, multiple residual stenoses were described along the RVOT, together with a VSD of 4.5mm, high pressure in the RV (85% of systemic), and a significant gradient at the level of the pulmonary homograft (63mmHg).
Before surgery, the habitual dose of bisoprolol was administered along with prophylaxis of bacterial endocarditis, and the AICD was deactivated. After habitual monitoring with pulse oximetry and noninvasive arterial pressure, the right femoral artery was cannulated without incident. This was used for both invasive monitoring and catheterization. Cerebral oximetry (rSO2) and the bispectral index (BIS) were also used, and adhesive patches were applied for the defibrillator. For sedation, propofol and remifentanil were administered via target controlled infusion (TCI) with a target BIS between 60 and 80, maintaining spontaneous respiration with nasal cannula at 31pm and monitoring with capnography, avoiding etCO2>50mmHg. The base values of rSO2 in both hemispheres were 67 and 69, respectively.
CalendarNot specified due to the characteristics of the case.
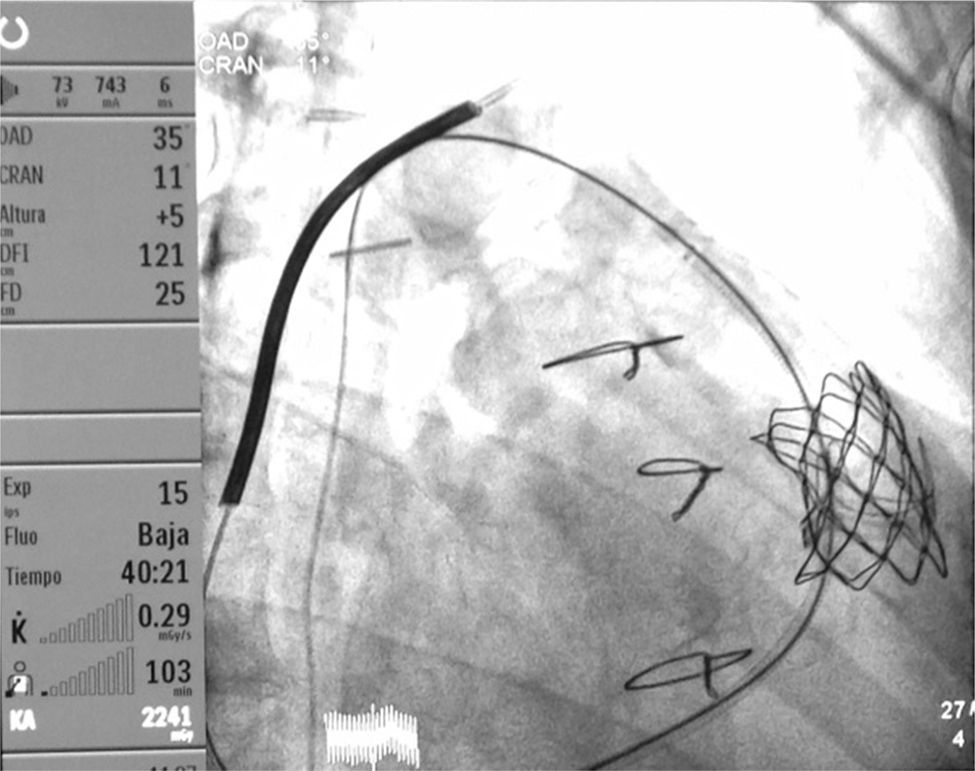
Monitoring and resultDuring the procedure, the patient was stable. The valve was implanted correctly, guided by radioscopy (Fig. 1) without incident, except for two self-limited incidents of desaturation that coincided with the valve dilation with good response to the transitory increase of FiO2. The rSO2 remained without significant changes (a reduction less than 10% bilateral rSO2). Later, she was transferred to the ICU for post-operative monitoring. Via transthoracic echocardiography, it was estimated that the pressure of the RV was around 70% of systemic and the gradient at the level of the pulmonary homograft was 40mmHg.
DiscussionDiscussion of medical literatureArterial switch techniques have improved the morbimortality of patients with TGV,1 90% of whom reach adult age.2 The surgery described by Rastelli is complex, and the persistence of heart disease oscillates between 5 and 15%, thus requiring monitoring and subsequent interventions,3 either open surgery or percutaneous procedures.2
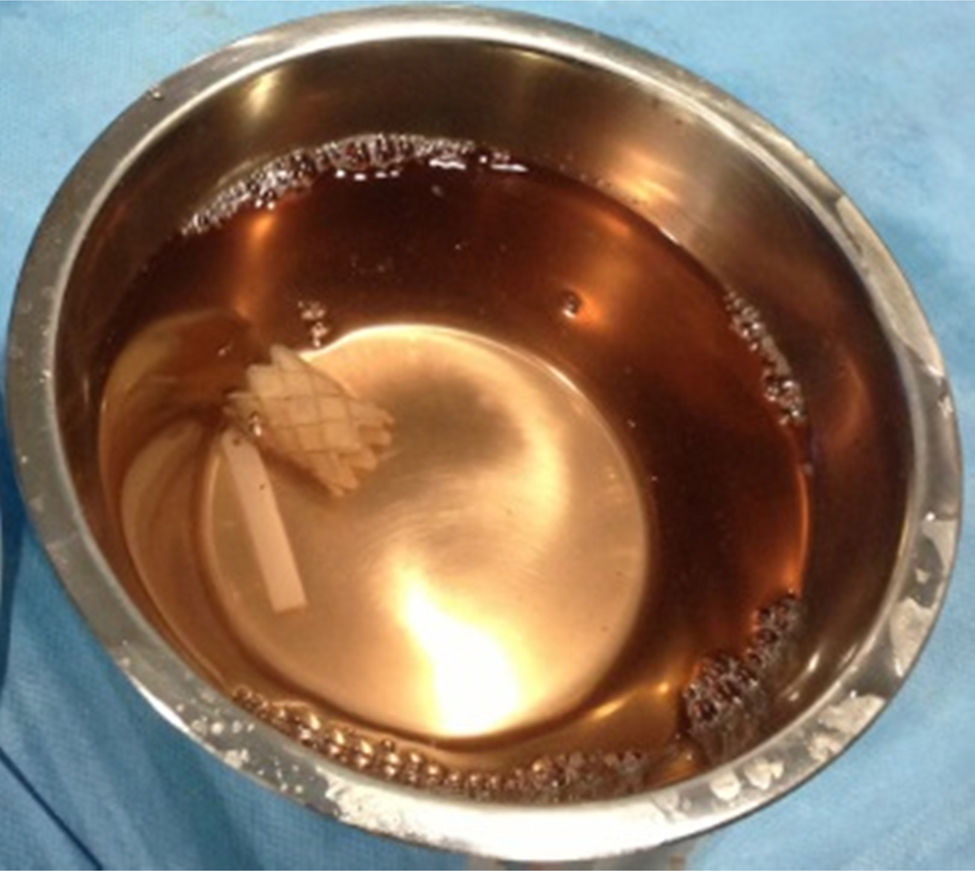
Melody® is the only device designed for percutaneous pulmonary valve replacement.3 It is a 35mm platinum-iridium stent coupled with a graft of bovine jugular vein (Fig. 2) for implantation through a central jugular or femoral venous access with a specific introducer–liberator. It is a palliative treatment for patients with a corrected and dysfunctional RVOT who develop a severe transpulmonary gradient, symptomatology, deterioration of functional class, and in patients in which the relative pressure of the right ventricle compared to the left ventricle is very high.3 Case series with tPVR with Melody® have shown good results.2 Reported mortality is <1%, and adverse effects described include: compression of coronary arteries, bleeding, hematoma, rupture of prosthetic conduit, arrhythmias, and embolization. These though, are infrequent.4
The ideal anesthetic technique for tPVR is controversial, with debate between general anesthesia and deep sedation.5 All publications found refer to aortic tVR. No bibliography was found regarding the anesthetic management of specifically pulmonary tPVR. Among the arguments in favor of general anesthesia are: better control of hemodynamic changes and possible complications, assuring the immobility of the patient, comfort in the use of the transesophageal echocardiogram (TEE), lower risk of aspiration and better adjustment of oxygenation and ventilation.5 As for sedation, it reduces morbimortality related to the induction of anesthesia, avoids endotracheal intubation and mechanical ventilation, provides better hemodynamic stability, requires fewer inotropic drugs and close neurological monitoring and, according to some authors, reduces the duration of the procedure favoring early recovery and reducing hospital stay.5 Although TEE during tPVR is a good support, it is not necessary in crucial steps such as valvuloplasty and valve implantation since they are guided by radioscopy. They can be complemented with a transthoracic echography during the procedure or in the post-operative period.5 General anesthesia would be the Gold Standard since it ensures better operative conditions in the critical steps of the procedure.6 Nevertheless, more and more there is a tendency toward minimal invasion,7 and sedation is considered a valid alternative in some health centers in tPVR procedures with femoral access. It is necessary to have material on hand for reverting to general anesthesia if necessary, for instance if a complication arises.
Certain consensus exists that tPVR should be performed in centers with a cardiovascular anesthesiologist, means for advanced cardiovascular support and mechanical circulation, availability of TEE, cardiopulmonary bypass and OHSVR.6
Management of our patientThe patient was operated on in a palliative manner with a pulmonary-systemic shunt, followed by definitive correction with the Rastelli technique. In terms of complications, she presented: residual VSD, an episode of ventricular tachycardia that required the implantation of an AICD, subaortic obstruction and stenosis of the VC of the RVOT. Given the significant gradient at the level of the pulmonary homograft (63mmHg) and the high pressures in the RV (85% of systemic), the patient was scheduled for tPVR, and both variables fell after the procedure (40mmHg and 70%, respectively). During the procedure, two self-limited episodes of desaturation occurred, coinciding with valve dilation (probably due to increasing the dead space). As such, a temporary increase in FiO2 would be prudent to improve the patient's functional reserve.
During tPVR, patient immobility is crucial. With the exception of arterial cannulation, it is not very painful. Some parameters should be defined to avoid oscillations in the level of sedation that can compromise the procedure. In our center, the pharmaceuticals generally used are propofol and remifentanil in TCI, for a target BIS between 60 and 80, paying special attention to the arterial cannulation and the valve dilation and implantation. The use of capnography allows for both an early intervention based on the early detection of hypoventilation (loss of the quality of the curve or an etCO2>50), thus improving the titration of the pharmaceuticals or the performance of maneuvers for opening the airways. In this way, it is possible to anticipate a desaturation that would require respiratory support and cause involuntary movement of the patient. This may include preventing excessive hypercapnia that would hinder the technique due to hypoxic pulmonary vasoconstriction.8 Sedation, together with rSO2 (to avoid reductions of more than 20% with respect to the patient's base values and an absolute value under 50%)9 allows for closer neurological monitoring, given the risk of cerebral (stroke) events.
A strict process for selecting patients as candidates for sedation should be carried out, taking into account the team's experience, the technical difficulty, the patient's cooperation, the cardiovascular tolerability to the procedure, and the difficulty of airway management.
LessonsEach case should be planned following a careful preoperative evaluation by a multidisciplinary team, considering risk/benefit. The experience in our center using deep sedation in tPVR procedures with femoral access is promising, though having an alternative plan to revert to general anesthesia is recommended. Randomized, prospective trials on a large scale are necessary to establish recommendations for our clinical practice.
Patient perspectiveThe patient saw the anesthetic management that we performed to be the one with most benefits given the nature of the surgical intervention and the associated risks.
Informed consentWritten informed consent was obtained for the publication of the case and associated images.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on human beings or animals for this study.
Confidentiality of dataThe authors point out that in this article, patient data does not appear.
Right to privacy and informed consentThe authors point out that in this article, patient data does not appear.
FinancingOur work was not financed.
Conflict of interestNo conflicts of interest exist.
Please cite this article as: Fernández-Castellano G, López-Herrera-Rodríguez D, Domínguez A, Sánchez-Carrillo F. Sedación para recambio valvular transcatéter de una válvula pulmonar melody®: informe de caso. Rev Colomb Anestesiol. 2017;45:55–58.