Submental intubation is a simple, fast and safe alternative associated with low morbidity rates as compared against tracheostomy. It is suitable for patients with nose obstruction due to craniomaxillofacial malformation.
Case report (clinical findings and therapeutic intervention)The goal of this study is to do a literature review of the procedure and a clinical case presentation of a patient with severe midface hypoplasia that as a consequence of the characteristics of the patient's malformation required submental intubation for surgical treatment.
ConclusionThe submental intubation technique is an excellent choice for orthognathic surgery in patients with facial malformations and airway problems.
La intubación submentoniana es una alternativa simple, rápida y segura, asociada a bajas tasas de morbilidad en comparación a la traqueostomía, que la faculta para utilizarse en pacientes que presentan obstrucción de la nariz debido a la malformación cráneo-maxilofacial.
Informe de caso (hallazgos clínicos e intervención terapéutica)El propósito de este estudio es la revisión de la literatura de este procedimiento y la presentación de un caso clínico de una paciente, con hipoplasia de tercio medio facial severa, quien por las características de su malformación requirió intubación submentoniana para realizar el tratamiento quirúrgico.
ConclusiónLa técnica de intubación submentoniana es una muy buen alternativa para realizar la cirugía ortognática en pacientes con malformaciones faciales y problemas de vía aérea.
Background: Maxillofacial surgery is challenging to both surgeons and anesthesiologists since they have to work over the same area and hence securing the airway is critical for the patient.1,2
Usually the endotracheal intubation technique uses a nasal or oral approach, but there are different pathologies of the craniomaxillofacial region involving the work area due to existing anatomy secondary to a tumor, a craniofacial malformation or complex face fractures,1–11 compromising the ability to secure the airway for an adequate surgical intervention and challenging a functional and esthetic tissue reconstruction.1,3 In the past, tracheostomy or cricothyroidotomy were the primary options1,5–7,9 in these cases for preserving a patent airway; difficult intubation due to the local conditions entails risks – such as airway trauma, laryngeal edema and bleeding, inter alia, all leading to difficult ventilation.6 The difficult airway is an important contributing factor to morbidity and mortality; hence, good airway management is an essential tool for the anesthesiologist during a maxillofacial procedure and to protect the working area when it is shared with other practitioners.
The purpose of this study is to discuss a clinical case of a patient with severe midface hypoplasia who, as a result of the characteristics of the patient's malformation, required submental intubation for surgical treatment.
Case reportDemographic information: The case of a female patient, 18 years and 11 months old, body weight 39.5kg is discussed.
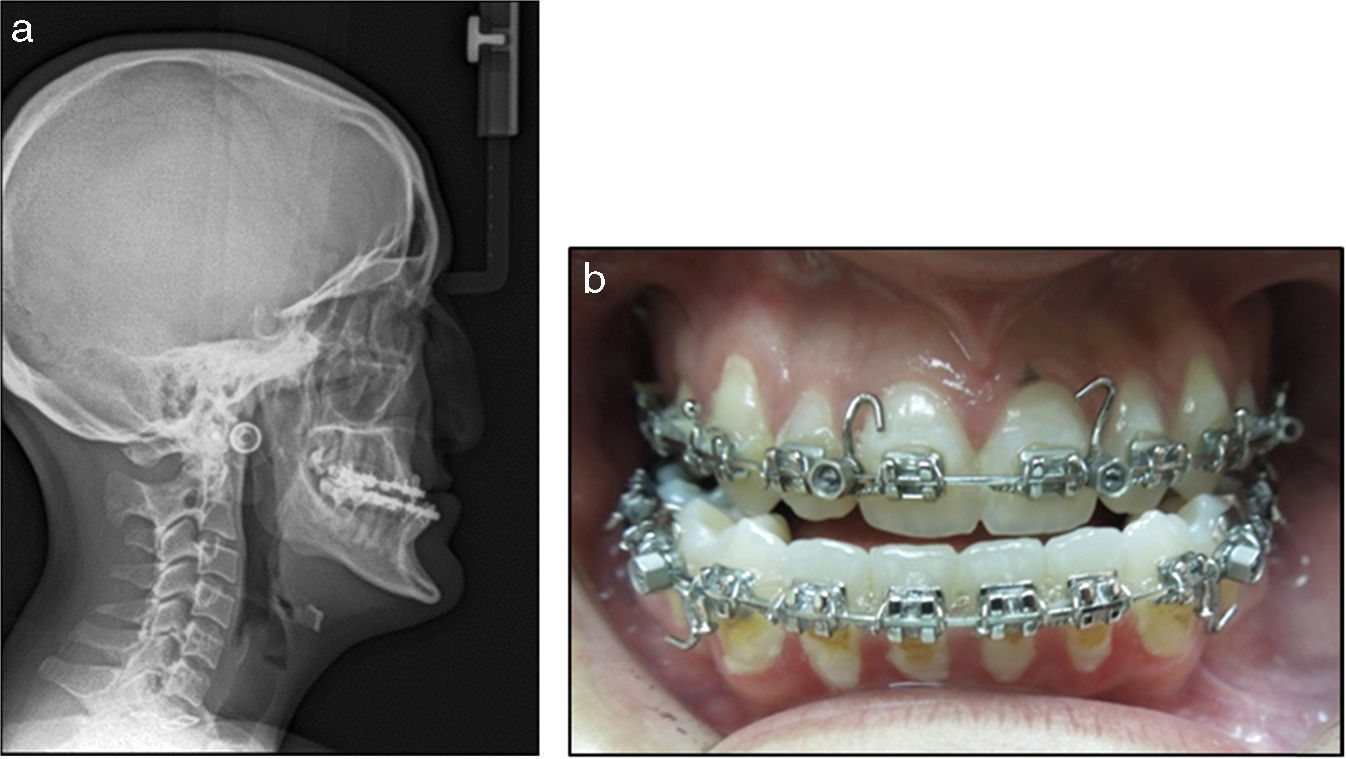
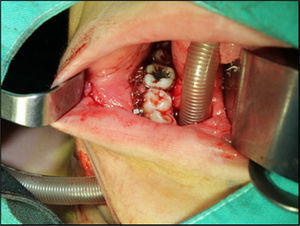
Among her clinical findings, severe midface hypoplasia was observed (Fig. 1), requiring orthognathic surgery for maxillary advancement and local iliac crest bone graft. The patient was previously evaluated by the Anesthesiology Service at the Hospital Nacional de Niños, with the following findings, in addition to the severe maxillary hypoplasia: significant stenosis of both nasal fossae, good mouth opening (28.5mm) and Cormack evaluation 1–2 (this scale evaluates the difficulty for visualizing the glottis during laryngoscopy). Plaster models were made for diagnostic evaluation and analysis of the case, as well as radiographs (cephalometric and orthopantomography). The blood tests and other exams were normal, so the patient classification was ASA I.
Following the case analysis, the decision was made to perform orthognathic surgery as a therapeutic intervention. The patient was pre-medicated with Midazolam during the anesthetic procedure with standard monitoring, receiving 0.50% air, 0.50% preoxygenation and 2% Sevorane. The protocol for the induction of anesthesia prior to intubation included Propofol 100mg, Fentanyl 100mcg, Atracurium 25mg, Dexamethasone 8mg, and Metamizol 1.2g. Nasal intubation was attempted afterwards as required by the surgical procedure for intraoperative management of dental occlusion. The right nasal cavity was totally obstructed and the stricture of the left fossa only allowed for the passage of a leaking 5.0 endotracheal tube with balloon that hindered the patient's ventilation, despite the absence of a balloon rupture or supraglottic intubation. This led the anesthesiologist to change the intervention as a result of this unexpected event, notwithstanding the previous evaluation. The decision was made to discontinue the surgical procedure and offer the parents the alternative of submental intubation with their prior consent. The patient was stable throughout the procedure.
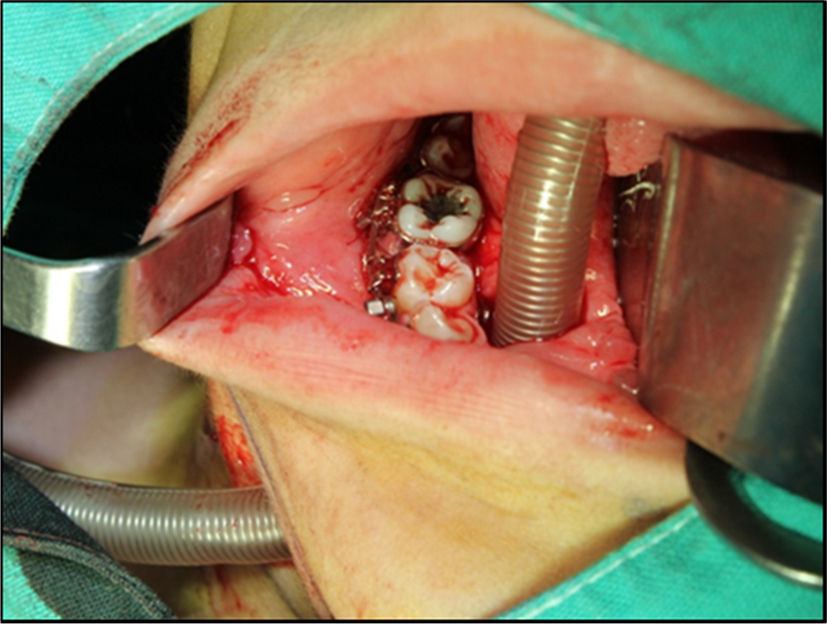
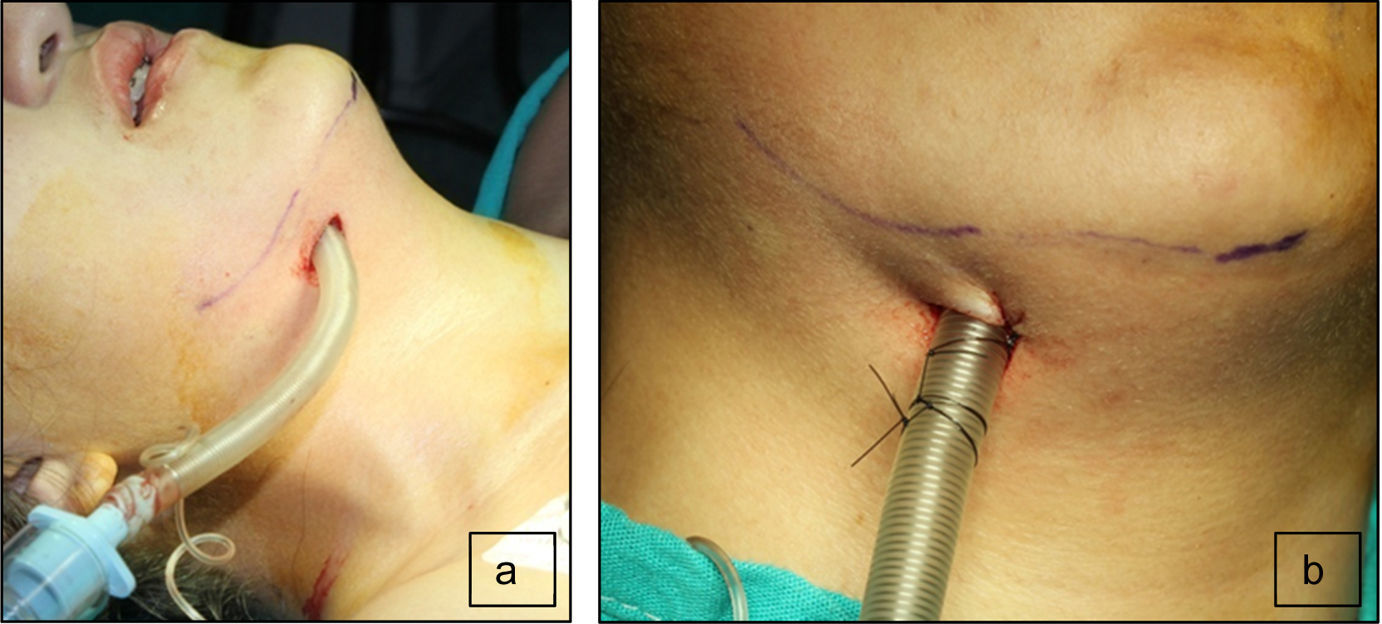
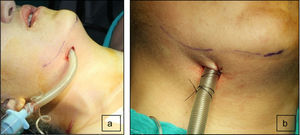
The second maxillofacial surgery scheduled for one week later followed the anesthetic procedure as previously described. The oral intubation was uneventful with a 6.5 catheter with balloon, so that upon the aseptic procedure and local anesthesia, the surgeon performed a 2cm skin incision to the right of the midline of the chin, parallel to the basal margin of the mandible. The incision was submental lateral instead of medial to avoid trauma to the Wharton ducts and interfere with the attachment of the genioglossus and geniohyoid muscles, and to avoid injury to the lingual vessels that in 98% of the cases are along the midline and lead to bleeding and sublingual hematoma.8 The muscles were carefully dissected, always in contact with the lingual surface of the mandible, behind the caruncles of the salivary duct to penetrate the mucosa of the floor of the mouth for creating a tunnel where the endotracheal tube was inserted outwards, for immediate placement of the connector and the circuit, completing the submental intubation (Fig. 2). The tube was then sutured to the skin (Fig. 3) to proceed with the surgical procedure as planned. It should be mentioned that the skin incision must be properly sized and the tissue dissection has to be long enough to externally slide the endotracheal tube with no difficulty. It is important to first insert the balloon through the tunnel and then the tube, since the tube blocks the passage. It is advisable to fix the tube to the skin of the submental region to avoid any intraoperative displacement. At the end of surgery, the tube sutures were removed and the tube was reinserted inside the oral cavity turning it into an orotracheal intubation again and proceed with extubation with no complications. The submental wound was sutured in planes and the intraoral wound was allowed to heal by secondary intention. The patient remained hemodynamically stable during surgery and the vital signs were within the normal parameters for a successful surgical outcome. During this second intervention, the patient did not experience any anesthesia or surgery-related adverse events.
Submental intubation was initially described as an alternate technique in complex cases and mainly as an option when the surgeon needs to control the dental occlusion,2,5,6,11 and when the facial fracture involves the nasal pyramid or extends into the base of the skull.5,7,10,11
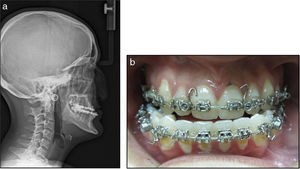
The advantages of this technique include simplicity,3–11 promptness,3,5–7,9,11 and low morbidity.3–5,8,9,11 It is a safe technique for managing the airway1–3,6,7,9–11 and does not interfere with any intraoral work during surgery or the intraoperative intermaxillary fixation.5–9,12 Likewise, submental intubation is a procedure that avoids tracheostomy and its complications,2–11 further care, equipment and extended hospital stay.4,6,9 The submental scar is cosmetic and practically invisible as compared with a tracheostomy scar,5–7,9–11 as shown in Fig. 4 depicting the patient with an almost undetectable scar. This approach may be used in a patient requiring orthognathic surgery with nasal obstruction.2,5,6,10,11 This was the reason for adopting this approach in this particular case. Similarly, this type of surgery reduces nasolabial tissue distortion when moving the maxilla12 or when a rhinoplasty is performed.2,9,12 It is also a way to approach frontonasal fractures7 and the submental incision is helpful for submental liposuction and platysmal plication.12
Some complications have been reported in the literature; for instance, salivary fistula in cases of prolonged ventilation,5,6,8,10 risk of submental tissue sepsis related to the possibility of a contaminated balloon during extubation,2,3,6,8–12 submental abscess,8,10,11 hypertrophic scar,2,3,8–10,12 high pressure resulting from endotracheal tube compression as a result of the acute angle of this inside the oropharynx,2,6,7,10 accidental extubation,2,3,9,10,12 accidental advancement of the endotracheal tube into the bronchi, endotracheal tube obstruction,2,3,9,12 tube damage when performing maxillary or mandibular osteotomy,2,8,9 bleeding,2,10 mucocele development,2,3,8,9,12 submandibular and sublingual glands and ducts trauma,2,3,9,11,12 vessel or nerve injury – for instance the lingual nerve2,3,9,12 – and orocutaneous fistulae.2,3,5,9,11
Some contraindications include patients requiring prolonged assisted ventilation,1–11 multiple trauma patients with neurological impairment,1–7,9,11 patients with chest trauma that need multiple surgeries where tracheostomy is the option of choice,2,3,5–7,11 as well as patients with wounds on the floor of the mouth,5,11 tumors in the maxillomandibular region, or unstable cervical trauma.1
In conclusion, the literature describes the submental intubation technique mainly in cases of complex facial trauma; however, this procedure shall be considered for orthognathic surgery, particularly in patients with severe facial malformations. This is a simple, safe, and rapid technique that allows an adequate airway management and requires professional skills and coordination, and avoids the need for a tracheostomy. As shown in this case, nasotracheal intubation could not be used due to the patient's anatomical conditions and orotracheal intubation was not indicated because the patient's occlusion had to be controlled during surgery.
Ethical approvalProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
FundingThe authors did not receive sponsorship to carry out this article.
Conflicts of interestThe authors have no conflicts of interest to disclose.
Please cite this article as: Navas-Aparicio MC, Díaz y Faz R. Intubación submentoniana: una alternativa útil para cirugía ortognática en pacientes con malformaciones craneofaciales. Informe de caso. Rev Colomb Anestesiol. 2017;45:50–54.