Patients with traumatic injuries of the cervical spine who undergo a surgical intervention are a great challenge to the anesthesiologist. The airway management inherently involves movements of the cervical spine that may aggravate pre-existing injury. Currently there is not a consensus for the technique of intubation of these patients.
We present three patients with traumatic injuries associated neurological symptoms and cervical spine. All intubations were assisted with fiber bronchoscope, without removing the cervical collar and patients remained awake. All patients were examined again after intubation with no evidence of worsening of their neurological symptoms. We can conclude that the fiberoptic assisted intubation has several advantages in the care of these patients.
Los pacientes con lesiones traumáticas de la columna cervical que se someten a un control quirúrgico de las mismas suponen un gran reto para el anestesiólogo. El manejo de la vía aérea conlleva de forma inherente movimientos de la columna cervical que podrían agravar la lesión preexistente. Actualmente no existe un claro consenso en la técnica de intubación de estos pacientes.
Presentamos tres pacientes con lesiones traumáticas de columna cervical y clínica neurológica asociada en los que se indicó cirugía. En todos ellos se realizó una intubación asistida con fibrobroncoscopio con el paciente despierto y sin retirar el collarín cervical. Todos los pacientes fueron nuevamente explorados tras la intubación sin evidenciarse en ninguno de ellos agravamiento de sus síntomas neurológicos. Podemos concluir que la intubación asistida con fibrobroncoscopio presenta varias ventajas en el cuidado de estos pacientes.
Traumatic injuries of the cervical spine constitute an important health problem due to their potential consequences for patients and society. Some 5–10% of emergency room patients, unconscious after their traumas, exhibit a complex cervical spine injury.1
Patients with traumatic injuries to the cervical spine who undergo a surgical intervention are a great challenge to an anesthesiologist. The use of the airway inherently involves movements of the cervical spine that could aggravate the preexisting injury.
We present three patients with traumatic injuries to the cervical spine and the associated neurological symptoms. We describe the management of their anesthesia, focusing on the use of the airway, and then we provide a discussion, citing the recent scholarship.
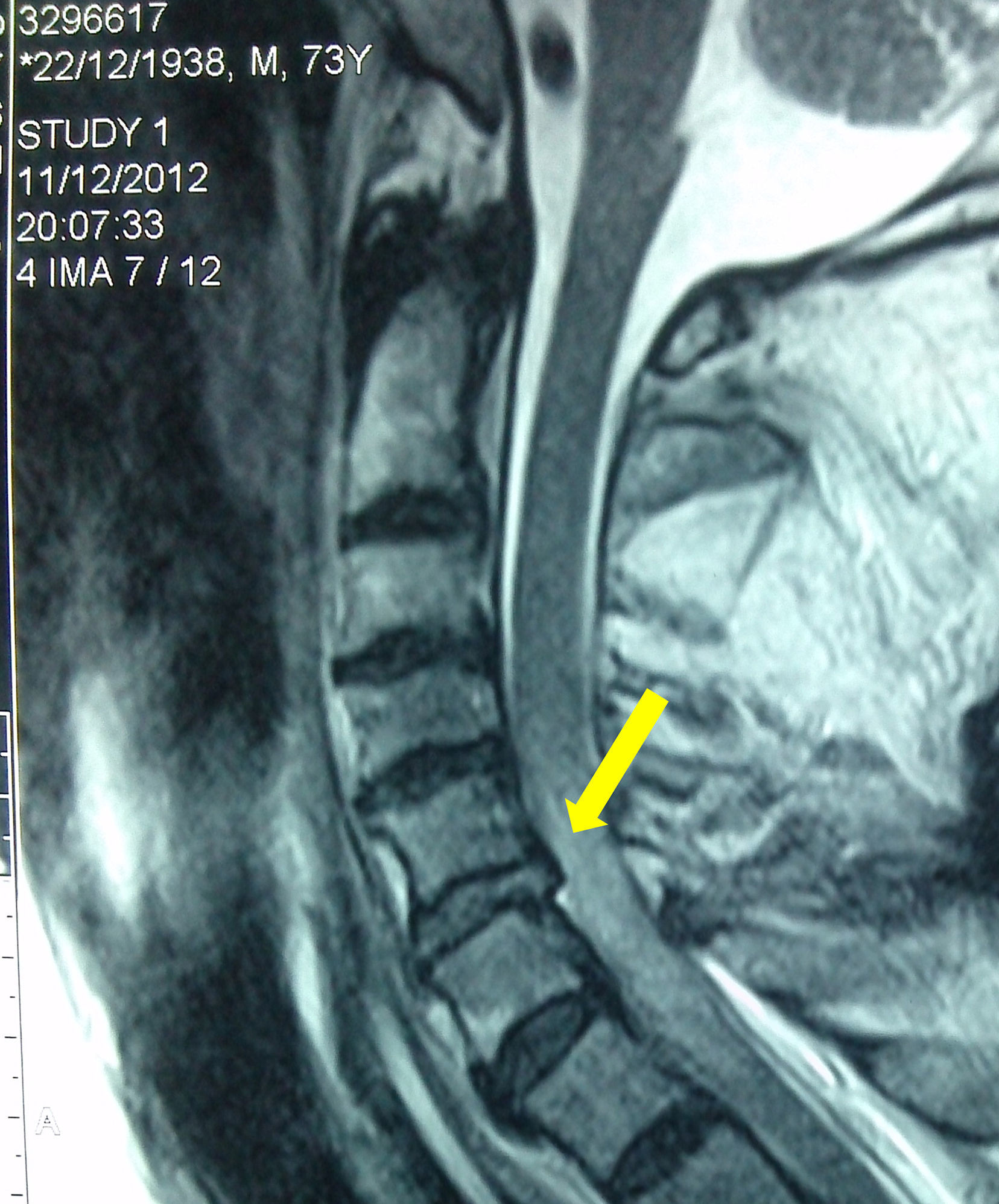
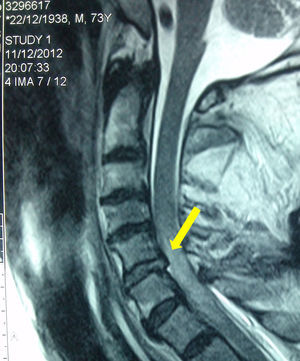
Case 1A 44-year-old Caucasian woman, with no previous history of injuries, suffered a fall and was immobilized with a semirigid neck brace. Upon further exploration it proved to be a tetraparesis without other apparent injuries. The computerized tomography (CT) of the cervical spine showed a dislocation of C5 over C6 (Fig. 1). A surgical fix was chosen, so we explained it to the patient and obtained her consent for the anesthetic technique. Three hours after her admittance, in the operating room, after basic monitoring, we initiated a perfusion of remifentanil at 0.05μgkg−1min−1. We kept the neck brace on and initiated oxygen therapy through nasal prongs with capnography. We administered topical anesthesia to the patient with lidocaine aerosol at 10% into the oral cavity and the pharynx, encouraging the patient to gargle with the solution, ventilating her intermittently with a flexible tube. After 15min we confirmed the anesthesia of the area, progressively introducing an oral catheter specifically for intubation with fiberoptic bronchoscopy. Through the catheter, we introduced a flexible fiberoptic bronchoscope, with a cuffed orotracheal tube (OTT) with an internal diameter of 7.5mm, previously inserted. Once we could see the glottis we administered 3mL of lidocaine at 2% through a flexible, single-tubed catheter introduced into the working channel of the fiberoptic bronchoscope. Next we advanced the catheter to the trachea and administered another 3mL of lidocaine. The patient responded with a small, involuntary self-limited cough and we introduced the fibrescope until we reached the carina. Afterwards we advanced the OTT, rotating it 90°, which coincided with a deep spontaneous inhalation from the patient. The maneuver was performed without difficulty. After confirming the positioning of the OTT with capnography, we performed a new neurological examination that ruled out an aggravation of the patient's symptoms and we administered anesthesia with propofol and rocuronium. We carried out an anterior arthrodesis without incident and the patient recovered without further injury.
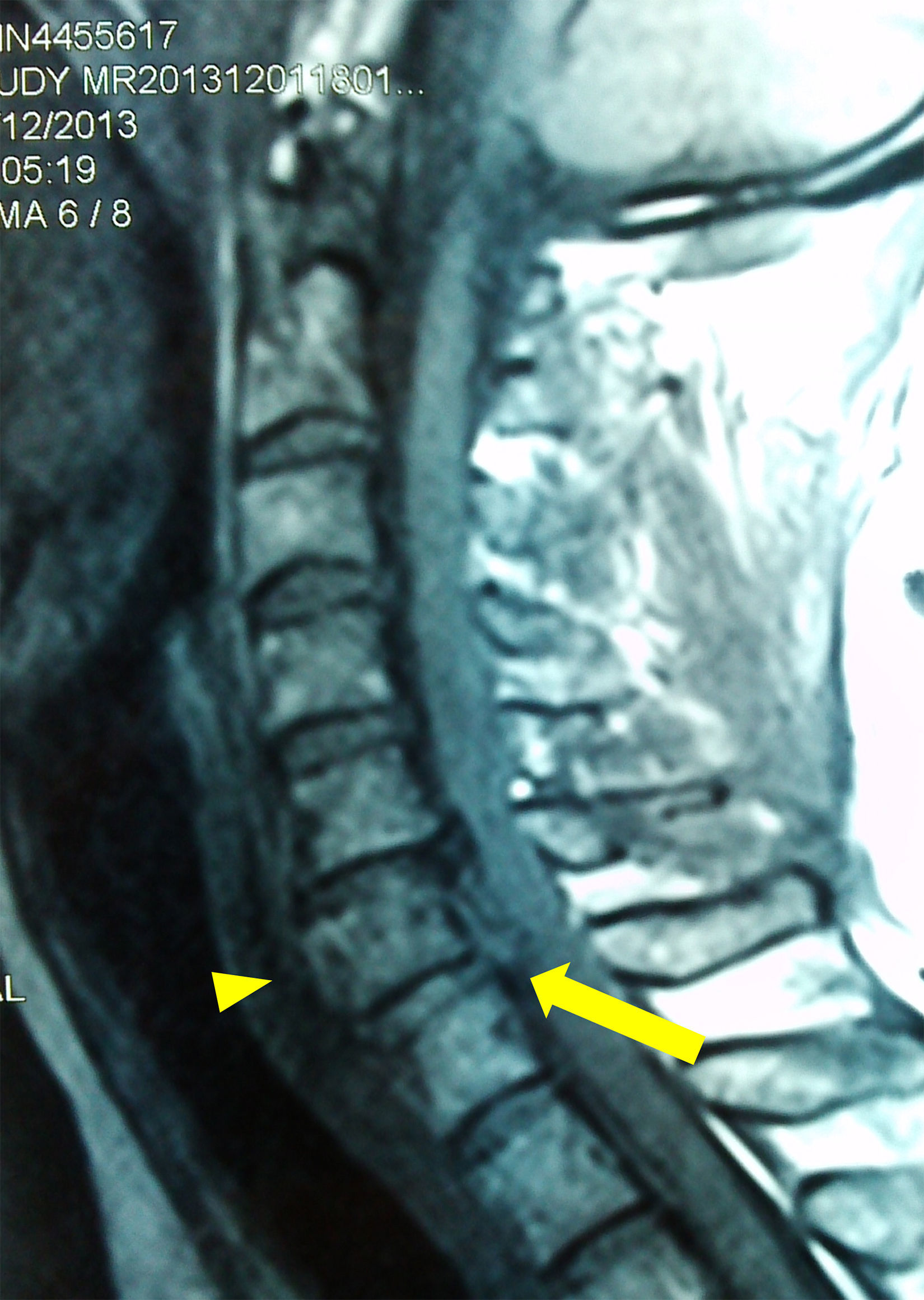
Case 273-year-old Caucasian male with a history of hypertension treated with enalapril and multiple falls due to repeated syncope. He was brought to hospital due to a new fall without any neurological clinical signs but was diagnosed via CT with a non-displaced fracture in the posterior arch of C6. He was discharged after conservative treatment. Three days later, he fell yet again and was brought back to the hospital. This time he presented with quadriplegia with a T4 neurological level. Emergency nuclear magnetic resonance (NMR) was performed, revealing a traumatic disk herniation of C5–6 with an associated medullary contusion (Fig. 2). He was admitted to the intensive care unit where mechanical ventilation with orotracheal intubation was initiated due to suboptimal ventilation capacity. After obtaining the patient's consent, we administered anesthesia in a manner identical to Case 1, with the peculiarity that this patient showed excellent tolerance to the intubation technique, probably due to a lack of coughing capacity associated with his injury. Neurological exploration posterior to intubation remained identical. Later, cervical fixation surgery was performed, but the patient's evolution was not favorable and he died five days later.
Case 350-year-old Caucasian woman with no history of interest. After a traffic incident, she was admitted with no apparent injuries and normal cranial and spinal TCs. After 24h, she gradually presented paraplegia and distal paresis of the upper limbs. Urgent NMR was performed, which showed traumatic disk herniation in C6–7, anterior displacement of the C6 body, and associated medullary contusion (Fig. 3). She apparently conserved her breathing capacity, though her basal oxygen saturation was at 89%. The patient understood and consented to our anesthetic plan and so the same technique as in previous cases was performed, with the exception that in this case larger doses of topical anesthesia were required due to initial intolerance of the oral cannula. In this case too, there were no changes in the neurological examination after extubation. A discectomy of the affected level was performed with surgical stabilization of C5–C7. The patient presented a minimal neurological improvement and was transferred to a specialized center for medullary injuries.
DiscussionIn the 1970s, the incidence of secondary neurological injury varied between 10% and 25%. After the introduction of out-of-hospital care systems and the generalization of the principles of immobilization, this incidence dropped drastically to 2–10.2
Since then, immobilization of the cervical spine during the treatment of these patients has been established as a standard practice, despite the non-existence of clear evidence of its benefit.3
There is a great sensitivity among the involved professionals due to the fear of causing greater neurological damage during the intubation of these patients. As such, protocols have been established that include manual in-line immobilization of the cervical spine during the manipulation of the airway.4 In recent years, the safety of this technique with respect to the integrity of the injured spine has been questioned.5,6 Furthermore, we have known for years that this practice makes intubation more difficult since it worsens the view from the direct laryngoscope.7
Multiple devices have arisen in recent years that, via indirect laryngoscopy, facilitate intubation with minimal cervical movement.8 Nevertheless, a considerable percentage of failed intubations present when compared to direct laryngoscopy, especially in the out-of-hospital context.9
If we analyze the movement of the cervical spine, all the devices evaluated mobilize it, thought the majority of these studies present favorable results for videolaryngoscopes when compared to direct laryngoscopy.8
When flexible fiberoptic bronchoscopes are compared, this technique is shown to mobilize to a lesser degree the affected spinal area.10,11 Undoubtedly, the use of the fiberoptic bronchoscope requires overcoming a learning curve, and so its use is limited to experienced professionals, and its recommendation cannot be generalized.
We consider it important to not remove the cervical collar for the treatment of these patients, whenever possible. We are conscious of the limitation of the mouth opening that this implies,12 but in the cases described, the anesthetic plan consists of maintaining the collar only during intubation with the fiberoptic bronchoscope since it bare requires a mouth opening. Were it necessary to change techniques, the collar would have been removed and a manual in-line immobilization would have been applied.
The decision to perform intubation with the fiberoptic bronchoscope on the waking patient was based on the following criteria: all were collaborative patients, had “full stomachs” (except case 3, who had been fasting for 24h), and we wished to perform a new neurological examination after intubation. In addition, ventilation with the facial mask and the manual opening of the airway are also strongly associated with movement of the cervical spine.10,13 When this intubation technique is performed on unconscious patients, it is usually necessary to ventilate the patient and perform the jaw thrust maneuver to improve the fiberscopic view.14
With the conscious patient, we are exposed to the risk that voluntary or involuntary movements in the patient, such as coughing, may mobilize the cervical spine. Therefore, it is essential to have their complete collaboration. Topical anesthesia is considered to be vitally important, and we never introduce the fiberoptic bronchoscope without previously ensuring an absolute tolerance to the deep insertion of the oral catheter.
If the intubation were not successful, our alternative would be to remove the cervical collar, apply manual in-line immobilization under sedation or general anesthesia, and to introduce a laryngeal mask with the possibility of intubation. We would ensure correct ventilation with the mask and would introduce the cuffed OTT through it.15 In the case of difficulty with the ‘blind’ intubation, we would use the fiberscope with the OTT inserted through the mask.16 This way, cervical mobilization would be minimal since, with a direct view of the glottis, we would not have to manipulate the mask to achieve intubation. A third option would be the use of a videolaryngoscope with a channel, which has also been used in these patients.17
The use of the fiberoptic bronchoscope to intubate patient with suspected cervical injury is widely accepted in the anesthesiology community. An analysis of American anesthesiologist showed that 78% use the fiberoptic bronchoscope for intubating these patients.18 Unfortunately, we were unable to ask the patients about their satisfaction with the anesthetic technique used.
If any of these patients were to require urgent control of the airway, we would reject this option due to the necessary preparation of materials and of the patient, unacceptably in an emergency context. We consider that the internationally recognized recommendations of the American College of Surgeons for the care of polytraumatized patients should be followed.4 In them, the use of direct laryngoscopy with manual cervical immobilization is recommended, with the possibility of videolaryngoscopes if one has experience with them.
Despite the fact that no clear evidence exists in favor of any device for the management of the airway of these patients, intubation assisted with fiberoptic bronchoscopes is the technique that causes the least mobilization of the cervical spine. Performing this technique with the patient awake avoids the necessity of manual ventilation and airway opening techniques. Furthermore, it allows for an immediate neurological re-examination after intubation. Nevertheless, for success, previous experience from the anesthesiologist is required, along with the patient's collaboration and excellent topical anesthesia of the involved anatomy.
Ethical disclosuresProtection of people and animalsThe authors state that for this investigation have not been performed experiments on humans or animals.
Confidentiality of dataThe authors declare that this article does not appear patient data.
Right to privacy and informed consentAll the patients gave express written informed consent, with the exception of Case 2 for whom a first degree relative provided it. All informed consent authorized the publication of the case description as well as images from their diagnostic tests. This document is held by the corresponding author.
FundingThe authors did not receive sponsorship to carry out this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Bilbao Ares A, Castañeda Pascual M, Merino Sierra B, Jimeno García JP, Martín Vizcaíno MP, Salvador Bravo M. Control de la vía aérea en pacientes con traumatismo sobre columna cervical y clínica neurológica. Informe de casos. Rev Colomb Anestesiol. 2017;45:45–49.