Patients suffering from a neuromuscular disease have a greater likelihood of postoperative respiratory failure. Sometimes, this complication does not respond to non-invasive mechanical ventilation.
Case reportPerioperative management of a patient with Werdnig–Hoffmann disease who underwent bilateral coronoidectomy due to trismus. The postoperative period was hampered by the patient's poor respiratory mechanics, inducing the appearance of atelectasis. Despite the application of preventive non-invasive mechanical ventilation, the patient suffered respiratory failure and required endotracheal intubation. Finally, the respiratory weaning was achieved after the application of insufflation–exsufflation devices associated with non-invasive mechanical ventilation.
ConclusionThe application of insufflations–exsufflation devices in the immediate post-operative period of patients with neuromuscular diseases promotes the proper respiratory evolution of a patient considered impossible to extubate.
El padecimiento de una enfermedad neuromuscular es un factor predictor independiente de insuficiencia respiratoria postoperatoria. Esta complicación en ocasiones no responde al tratamiento con ventilación mecánica no invasiva.
Presentación del casoManejo perioperatorio de un paciente con enfermedad de Werdnig-Hoffmann que fue intervenido de coronoidectomía bilateral por trismus. Su evolución postoperatoria se vio dificultada por la mala mecánica respiratoria del paciente que favoreció la aparición de atelectasias. A pesar de la aplicación de ventilación mecánica no invasiva de forma preventiva, el paciente terminó sufriendo insuficiencia respiratoria y requiriendo intubación orotraqueal. Finalmente se logra el destete respiratorio tras la aplicación de dispositivos de insuflación-exsuflación asociados a la ventilación mecánica no invasiva.
ConclusiónLa aplicación de los dispositivos de insuflación-exsuflación en el postoperatorio inmediato de pacientes con enfermedades neuromusculares favorece la adecuada evolución respiratoria de un paciente considerado inicialmente como imposible de extubar.
Non-invasive mechanical ventilation (NIMV) is an effective tool to fight against post-operative respiratory insufficiency. It avoids, in many cases, the need to establish invasive mechanical ventilation (IMV).1
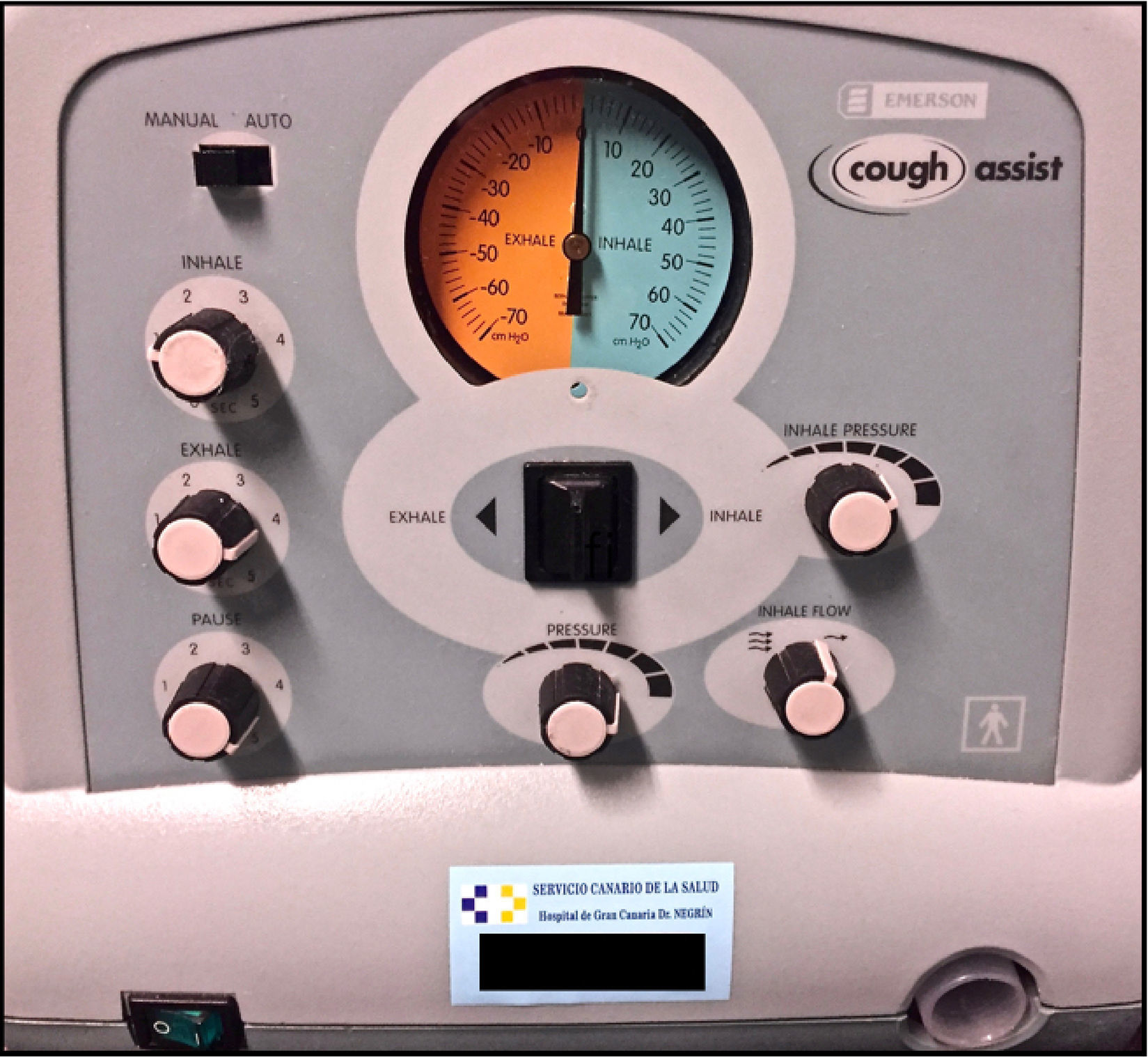
Suffering from a neuromuscular disease is an independent predictive factor of prolonged post-operative IMV.2 The weakness of the respiratory muscles, as well as the decrease in pulmonary volumes and inspiratory capacity, are associated with ineffective coughing. On the other hand, the poor respiratory mechanics of these patients means that their weaning from IMV is considered difficult or even, on some occasions, impossible.3 It has been demonstrated that the use of insufflation–exsufflation devices, like Cough Assist® (JH Emerson Co. Cambridge, MA, USA), increases the efficacy of the coughing, thereby reducing the incidence of post-operative respiratory complications in these patients,2 as well as the need of prolonged IMV.3
We present the case of a patient with Werdnig–Hoffmann disease, who suffered from post-operative respiratory insufficiency. It was solved with the combination of NIMV, an insufflation–exsufflation device, and cleaning bronchoscopy.
Clinical casePatient information25-year-old male, diagnosed with type 2 Werdnig–Hoffmann disease at fourteen months of age. He suffered difficulties eating orally due to the presence of trismus. As such, he was scheduled for a bilateral coronoidectomy and masseter muscle release.
In terms of antecedents, the patient had been operated when he was 15 years of age for D3-L4 arthrodesis due to paralytic scoliosis. After the intervention, he suffered from a deep femoral thrombosis in the lower right limb secondary to a deficit of factor V Leiden, requiring treatment with oral anticoagulants. Due to the restriction caused by the thoracic deformity, he suffered from symptoms of respiratory insufficiency, which evolved favorably with home-based physiotherapy, without needing NIMV. At 20 years of age, he underwent an atypical apical segmentectomy of the upper lobe of the right lung due to recurrent pneumothorax, without perioperative incidents. In addition, he was being studied by endocrinology due to severe malnutrition.
Clinical findingsIn the physical examination conducted in the anesthetic evaluation, he demonstrated pronounced muscular atrophy, as well as strong retromicrognathia, and mouth opening limitations. As a result, he was classified as having a difficult airway, and it was decided that nasotracheal intubation would be performed with a fibrobronchoscope while the patient was awake, maintaining the spontaneous respiration (Fig. 1). Intubation was difficult, due to the excessively anterior position of the glottis. Then, the patient underwent intravenous induction of anesthesia with 2mgkg−1 propofol, continuous infusion of remifentanil (0.05–0.1mcgkg−1min−1), and 0.5mgkg−1 of rocuronium. Intraoperative maintenance was carried out with propofol and remifentanil in continuous infusion, without needing additional doses of neuromuscular blocking agents.
After finalizing the surgery, the patient was admitted to the Resuscitation Unit to protect the airway during the post-operative period. 24h after admittance, sedation was withdrawn, and the patient was extubated without incident after the placement of an airway exchange catheter due to the difficulties associated with the airway management.
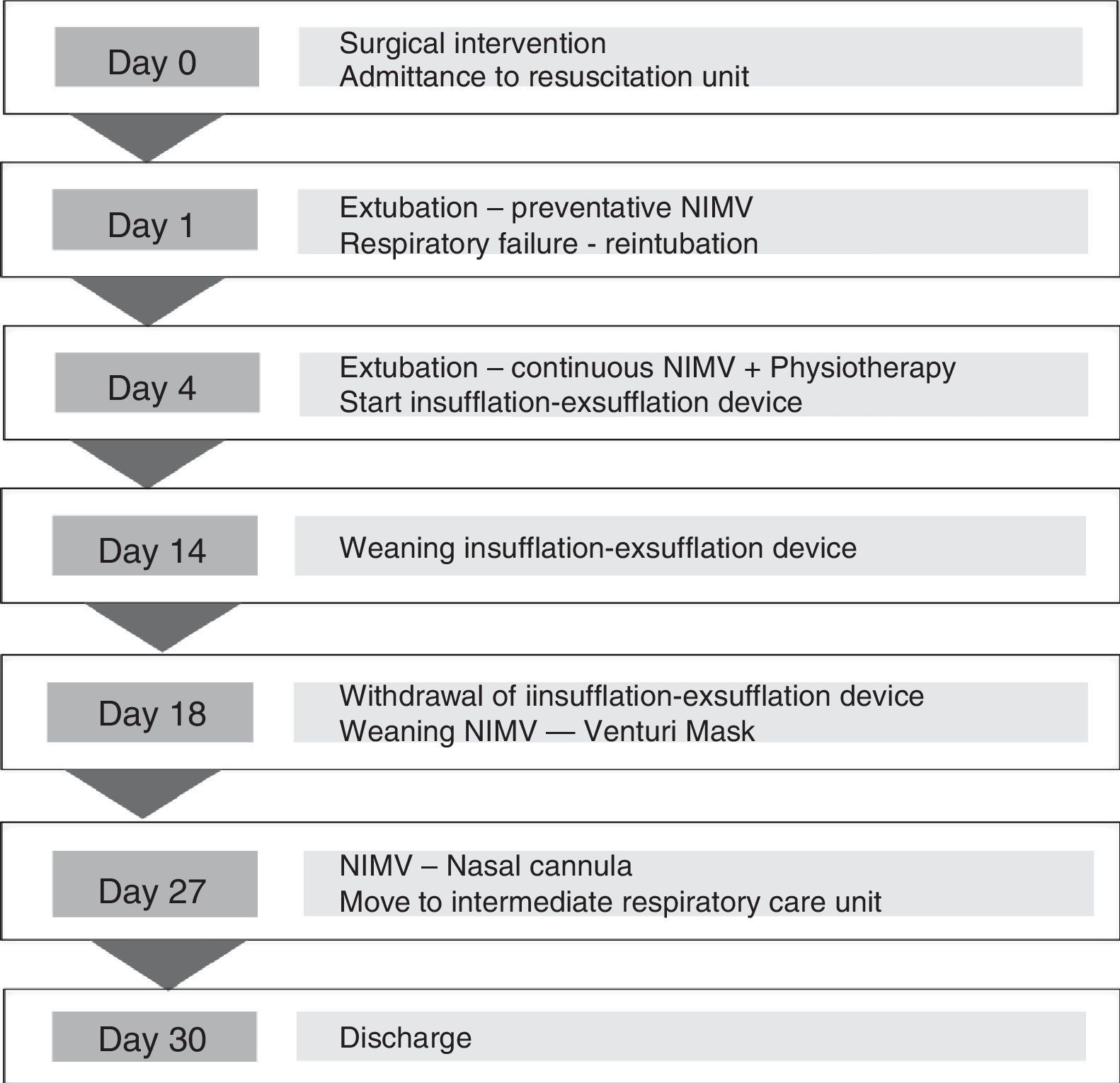
CalendarThe patient's evolution, detailed in the text, is summarized in Fig. 2.
Diagnostic evaluationAfter extubation, NIMV was applied preventatively with BiPAP (iPAP 15, ePAP 8). Despite this, the patient showed poor respiratory mechanics, and a complete right atelectasis could be seen in the X-ray. Arterial blood gas showed hypercapnic respiratory insufficiency (pH 7.21, pO2 69mmHg, pCO2 76mmHg, bicarbonate 23mmol/L). As such, it was necessary to intubate the patient. Three days later, and after detecting clinical improvement and an improvement in the complementary tests, it was decided that the patient would be weaned off IMV gradually, ending sedation and making extubation possible.
Therapeutic interventionAfter the second extubation, continuous NIMV was implemented (iPAP 15, ePAP 10) with good patient's tolerance. However, thoracic X-rays showed again the right atelectasis. Cleaning fibrobronchoscopy was performed, and intense respiratory physiotherapy was initiated in order to stimulate coughing and the expulsion of respiratory secretions. Since the patient continued with ineffective coughing, the device Cough Assist® was employed (Fig. 3). It was used alternated with NIMV three times per day, with an insufflation pressure of 40cmH2O, followed by an abrupt exsufflation of −40cmH2O.
Monitoring and results10 days after the second extubation, after observing an improvement in the patient's respiratory mechanics and in his capacity to expectorate, the frequency of the application of the insufflation–exsufflation device was reduced to once per day.
Four days later, after clinical improvement, and after ensuring the absence of atelectasis by X-ray, the use of this device could be discontinued completely. Furthermore, NIMV weaning procedures were started, alternating NIMV with longer periods of spontaneous ventilation through a Venturi mask, showing the patient a good tolerance. The patient was discharged from the Resuscitation Unit 27 days after his admittance, with good respiratory mechanics, alternating nasal cannula with BiPAP without incident. He was transferred to the Intermediate Respiratory Care Unit for continuing care. It was possible to discharge him from the hospital 72h later, with the recommendation of using BiPAP at home.
DiscussionThe perioperative management of patients with neuromuscular diseases implies a challenge to anesthesiologists. Successful post-operative evolution requires the utilization of measures to prevent the appearance of respiratory complications.
Werdnig–Hoffmann disease is a neuro-degenerative illness that affects the first motor neuron. This disease is included in spinal atrophies, with a recessive autosomal genetic transmission pattern. Its incidence is estimated at 1/5000–10,000 live new borns,4 with wide phenotype variability in its clinical expression. Patients affected by this disease suffer from hypotonia, weakness, and proximal muscular atrophy, without any effect on cognitive capacity. The presence of retrognathia and micrognathia, tongue twitching, and abundant secretions is frequent. 55% of patients with type 2 Werdnig–Hoffmann disease present significant scoliosis, which worsens the respiratory prognosis and frequently requires surgical treatment. This leads to a poor respiratory mechanics and secretion retention favoring the appearance of recurring respiratory tract infections.
The prognosis of these patients is determined mainly by the age of appearance of symptoms and their evolution. It also depends on how early an appropriate nutritional, orthopedic, physiotherapeutic, respiratory, and neurological treatment is implemented.5 Death is generally a consequence of respiratory failure. In recent years, because of the improvements in clinical care, their survival has been increasing.6 As a result, these patients will be found more and more often in the operating room.
Most of the cases found in the bibliography referring to the anesthetic management of patients with Werdnig–Hoffmann disease used regional anesthesia, avoiding airway management and the need of mechanical ventilation.6,7 In the cases in which general anesthesia was required, the use of neuromuscular blocking agents was avoided.8,9 There are few cases in which they were used, due to the hypersensitivity of these patients to neuromuscular blocking (just as has been demonstrated in different studies) associated with respiratory complications and post-operative residual curarization.10 In the present case, due to the characteristics of the intervention, it was necessary to use general anesthesia with a neuromuscular block. The applicability of sugammadex as an effective agent for reverting the neuromuscular block secondary to rocuronium in these patients has been demonstrated.11
Furthermore, patients with neuromuscular diseases present difficulties in IMV weaning. The prolonged use of IMV may lead to the need of tracheotomy to reduce potential complications and sedation requirements, to improve patient comfort, and to facilitate their weaning.1
NIMV has been used in the prevention and treatment of post-operative respiratory insufficiency, averting the high morbidity and mortality associated with IMV.1,12 Therefore, its use should be considered in the respiratory management of these patients. The use of NIMV preventatively reduces the appearance of nosocomial infection, the length of hospital stay, and mortality.1 In addition, it increases the survival, the quality of life, and the cognitive function of patients with chronic hypoventilation.13,14 It should be pointed out that NIMV weaning should also be carried out gradually to be successful. It should also be taken into account that patients with neuromuscular diseases may require continuing the use of NIMV after their hospital discharge.5
Patients with neuromuscular diseases suffer from altered respiratory mechanics, which favors the retention of secretions. This predisposes them to the appearance of respiratory complications15 such as atelectasis. Bronchoscopy continues being the technique of choice for the resolution of atelectasis. However, in these patients, insufflation–exsufflation devices have demonstrated their preventative and curative utility. These devices simulate the physiological coughing mechanism, allowing the removing of the secretions via positive pressure (insufflation) followed by an abrupt change to negative pressure (exsufflation). It should be applied several times per day through oro-nasal interfaces, with a recommended duration of each of the parts of the respiratory cycle of 2–4s, and reaching pressures of 40–70cmH2O, in both insufflation and exsufflation. Its use improves pulse oximetry and dyspnea with good tolerance and safety,15 prevents the appearance of atelectasis,16 and reduces the need of tracheotomy due to respiratory insufficiency.17
ConclusionThe perioperative management of patients with neuromuscular diseases is a challenge for anesthesiologists. The increased incidence of respiratory complications predisposes them to a prolonged post-operative IMV. As their respiratory weaning is difficult, they require the early application of NIMV. Nevertheless, the preventative use of NIMV is not sufficient for preventing the appearance of complications, making it necessary to apply other means of respiratory support, such as insufflation–exsufflation devices. We consider that the application of these devices is useful in the immediate post-operative period and may reduce the need of IMV.
Patients with neuromuscular diseases that present post-operative respiratory insufficiency and require intubation may be extubated with a combination of NIMV and insufflation–exsufflation devices.
Patient outlookCurrently, the patient is asymptomatic and tolerates oral feeding without incident. NIMV assistance was required for two months after hospital discharge, and he is now eupneic and without any respiratory support.
Ethical disclosureProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors obtained the informed consent of all patients and/or subjects herein mentioned. No patient's data are shown in this article.
FinancingThe authors declare that they did not receive financing for the completion of this article.
Conflicts of interestThe authors declare that no conflicts of interest exist.
Please cite this article as: Becerra-Bolaños Á, Ojeda-Betancor N, Valencia L, Rodríguez-Pérez A. Dispositivos de insuflación-exsuflación en el fracaso respiratorio postoperatorio: informe de caso. Rev Colomb Anestesiol. 2017;45:40–44.