Patients with valve disease are at a higher risk of perioperative complications in the context of non-cardiac surgery. The active involvement of the anaesthetist from the moment of the pre-anaesthesia assessment to determine the severity of the disease is crucial.
The purpose of this report on the management of a clinical case is to highlight the need for a multidisciplinary approach to the patient with heart disease.
We present the case of a patient in the eighth decade of life with severe aortic stenosis, and a 46mm infra-renal abdominal aortic aneurysm; chronic obstructive pulmonary disease, controlled arterial hypertension; and a lymphoproliferative process. Following the pre-anaesthesia assessment, valve repair surgery was indicated prior to a surgical procedure for colon cancer resection. Key to the successful management of this patient was pre-operative optimization with cardiac surgery and adjustment of the pharmacological treatment, plus haemodynamic monitoring as a basis for decision-making during the perioperative period using a minimally invasive device (Vigileo®). Spinal analgesia with intrathecal morphine was combined with general anaesthesia. The patient remained stable with CI 2.3–3l/min/m2, SVV 2–7% and ScvO2 74–67%.
As a result of the successful anaesthetic and surgical process, we concluded that it is our duty at the present time to know and apply the recommendations contained in the guidelines developed by the anaesthesia and cardiology societies and their regular updates, as they allow clinicians to make decisions in accordance with evidence-based protocols.
Los pacientes con enfermedad valvular presentan mayor riesgo de complicaciones perioperatorias en el contexto de cirugía no cardiaca. La importancia del anestesiólogo desde la consulta de preanestesia para valorar la severidad de la enfermedad y su intervención activa es determinante.
El manejo de este caso clínico se reporta para poner en valor la necesidad que tiene el paciente cardiópata de ser atendido de manera multidisciplinar.
Presentamos el caso de un paciente de 80 años con estenosis aórtica severa, aneurisma de aorta abdominal infrarrenal de 46mm; enfermedad pulmonar obstructiva crónica, hipertensión arterial controlada; proceso linfoproliferativo. Tras valoración preanestésica se indicó cirugía valvular reparadora previa a la cirugía por cáncer de colon. La optimización preoperatoria mediante la cirugía cardiaca y el ajuste del tratamiento farmacológico, así como el apoyo en la monitorización hemodinámica para la toma de decisiones durante el periodo perioperatorio, mediante un dispositivo mínimamente invasivo (Vigileo®), fueron las claves en el correcto manejo de este paciente; combinamos raquianalgesia con morfina intratecal y anestesia general. El paciente se mantuvo estable con IC 2.3 - 3 l/min/m2, VVS 2 - 7% y ScvO2 74 - 67%.
Tras el éxito del proceso anestésico-quirúrgico concluimos que hoy en día tenemos la obligación de conocer y aplicar las recomendaciones disponibles en las guías elaboradas por las sociedades de anestesiología y cardiología, de forma conjunta, que se actualizan continuamente y permiten al clínico protocolizar la toma de decisiones basándose en la evidencia científica.
Since the implementation of protocols for pre-anaesthesia assessment, anaesthetists play a crucial role in optimizing the outcomes of the process of anaesthesia and surgery. This goal is more critical still in patients with heart disease, and guidelines have been developed to provide recommendations on the care for these patients.1,2 These guidelines must be applied during the pre-operative, intra-operative and post-operative periods and range from the modification of an inadequate pharmacological treatment to prior cardiac surgery and careful intra-operative and post-operative haemodynamic monitoring. Guidelines are based on scientific evidence and are developed jointly by expert cardiologists and anaesthetists. The literature shows that in elderly patients with severe aortic stenosis, which was the case of our patient, survival improves significantly when interventions are used, as compared with non-intervention.3–5
At present, anaesthetists play a key role in optimizing the patient's condition and their intervention does not result in a significant delay.
Clinical caseAn 80 year-old male patient with rectal neoplasia in whom assessment revealed asymptomatic severe aortic stenosis (valve area 0.8cm2); a 46mm infra-renal abdominal aortic aneurysm; chronic obstructive pulmonary disease; arterial hypertension and a lymphoproliferative process. Following the cardiology consult, it was decided to take the patient to valve repair and placement of a no. 23 biological prosthesis through a ministernotomy approach.
The patient was referred 4 months later for a new assessment after the valve exchange procedure and neoadjuvant therapy to shrink the tumour, and re-assessment for the oncology surgery indication.
The new echocardiogram showed a slightly dilated, normally functioning left ventricle (FEV1 65%), with no contractility abnormalities; a dysfunctional biologic prosthesis with maximum and mean gradients of 45 and 23mmHg and impressive peri-prosthetic leaks; moderate-to-severe tricuspid regurgitation with an estimated PASP of 50mmHg; and bi-atrial dilatation (AI 47mm–31cm2).
During the period following valve exchange and chemotherapy, the patient had two episodes of left heart failure, which responded to pharmacological treatment. Cardiac catheterization showed normal coronary arteries.
The patient was on treatment with bisoprolol, terazosine, budesonide, ipratropium bromide, atorvastatin, irbesartan, ferrous sulphate, potassium supplementation, and ranitidine.
Following reassessment, the patient was diagnosed with severe postoperative aortic regurgitation due to biological prosthesis dysfunction, with good systolic function; functional class II; COPD and moderate pulmonary hypertension. Pharmacological treatment was optimized with discontinuation of bisoprolol and atorvastatin and addition of enalapril and furosemide. The patient was informed of the anaesthesia and surgical risk, and the informed consent was obtained.
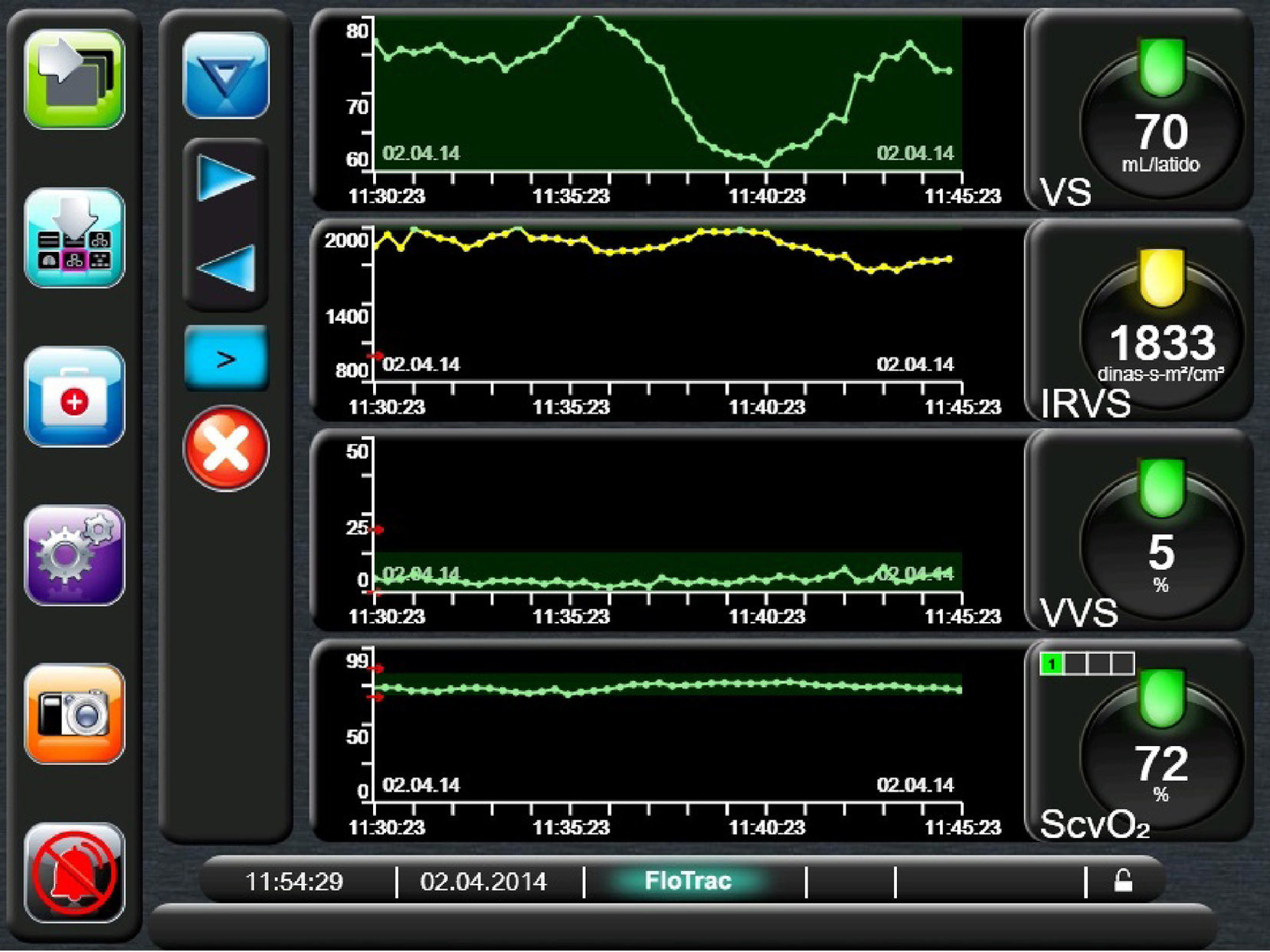
The patient was premedicated with oral lorazepam, budesonide and salbutamol inhalations, and Actocortina i.v. In the operating room, the patient was monitored with 5-lead electrocardiography (II and V5) and continuous recording of the depth of anaesthesia. Midazolam was administered and a left radial artery access was established for invasive blood pressure and cardiac output monitoring. Spinal analgesia was provided using a 25G Whitacre needle at L2–L3 with intrathecal administration of morphine 200μg and lidocaine 18mg. Anaesthesia induction was then started with etomidate 12mg, midazolam 2mg, ketamine 40mg, fentanyl 100μg and rocuronium 50mg. Anaesthesia was maintained with sevofluorane, fentanyl and rocuronium; hourly diuresis was recorded and a PreSep® catheter was used for haemodynamic monitoring of cardiac output (CO), systolic volume (SV), systolic volume variation (SVV), central venous saturation of oxygen (CvsO2), systemic vascular resistance (SVR) be means of a Flo Trac/Vigileo (Edwards Lifesciences®) system (Fig. 1).
Haemodynamic monitoring through the use of a Flo-Trac/Vigileo (Edwards Lifesciences®) system.
Operating room monitor view of haemodynamic recordings: systolic volume (SV mL/beat), systemic vascular resistance (dynes-s-m2/cm2), systolic volume variation (%SVV) and central venous oxygen saturation (CvsO2%).
The patient remained stable with CI 2.3–3l/min/m2, SVV 2–7% and CvsO2 74–67%. The procedure was performed through a midline laparotomy and lasted 160min. During specimen removal there was an estimated blood loss of 600ml, resulting in a drop in SV (down to 62ml/beat) and a 10% increase in the SVR index, with no significant reduction in mean arterial pressure (MAP). This was solved with an increase in fluid therapy and transfusion of concentrated red blood cells (Fig. 1). CvsO2 was maintained between 76 and 72%. Following the procedure, the patient was transferred to the critical care unit under mechanical ventilation in order to continue haemodynamic monitoring with the Vigileo®. In the first 24h, 1000cc were recovered from the surgical drain and the patient developed thrombopeni with a platelet count of 60,000 requiring a new transfusion of two units of red blood cell and platelet concentrate. The patient was maintained under controlled ventilation during the first few hours in order to be able to use the information from the Flo Trac® system and initiate dobutamine perfusion (decreasing doses starting at 12μg/kg/min) for four days to maintain MAP without significant increases in SVR, which would be detrimental for aortic regurgitation. The patient was discharged from the critical care unit on the ninth postoperative day and had a favourable course in the ward.
DiscussionThe literature shows that in elderly patients with severe aortic stenosis, survival after valve replacement improves significantly when compared to patients who are not intervened.3–5 However, based on preoperative recommendations from the European Society of Cardiology,2 valve repair surgery would not be warranted in patients with severe asymptomatic aortic stenosis before they are taken to cancer surgery if the latter is classified as a low-medium risk procedure. In our patient, the surgery was classified as “moderate-to-high” risk given the possibility of bleeding; the decision was further supported by the patient's age and comorbidity. However, a high degree of regurgitation of the replaced valve was found postoperatively, with clinical repercussions in the form of two episodes of heart failure. A good ejection fraction (FEV1: 67%) was evidenced before the oncologic surgery (67%) despite moderate-to-severe TR leading to the decision of not delaying the tumour resection surgery. In compliance with the guidelines, the cardiology service reassessed the treatment (introducing enalapril and discontinuing beta-blockers). The labile haemodynamic condition inherent to valve disease6 and the potential clotting abnormalities were taken into consideration for the anaesthetic management, leading to the combination of intrathecal morphine for spinal analgesia with general anaesthesia, as proposed by some authors,7,8 because we considered this approach as an adequate alternative to epidural analgesia (with no need to use a postoperative catheter), with very good haemodynamic stability.
We used a minimally invasive continuous haemodynamic monitoring device (Vigileo®), maintaining VsO2 values above 70. This was of great help for decision-making. A physiologically normal heart cannot fail in the event of high oxygen demand (hyperdynamic status: sepsis, thyrotoxicosis, surgery, etc.) and with the specific assumption of a non-functional valve, exquisite haemodynamic control is mandatory.2,6 Since its introduction, the pulmonary artery Swan-Ganz catheter has been the gold standard for monitoring. However, the cost/benefit ratio, the fact that it is not risk-free and the difficulty of interpreting the data by staff that does not use it routinely means that it is not usually available non-cardiac surgery operating. The new minimally invasive, easy-to-use monitoring devices are of great clinical use and a critical resource; consequently, their availability in all hospitals is desirable. The impact of the use of these systems on morbidity and mortality is the subject of on-going study.9,10
We conclude that the multidisciplinary approach to the correct assessment, treatment and haemodynamic control of the patient with heart disease during the perioperative period is critical for prognosis. Decision-making must be based on the recommendations contained in the guidelines developed by the relevant scientific societies, and haemodynamic management must be supported by an algorithm designed to ensure optimal oxygen delivery to the tissues. A four-month delay in performing the colectomy was a time used for active optimization as was explained to the patient: (a) cardiac surgery; (b) pharmacologic adjustment; and (c) chemotherapy.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FinancingThe authors did not receive sponsorship to carry out this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Rodríguez-Navarro MÁ, Rastrollo-Peña D, Iranzo-Reverter J, Sánchez-Ortega JL, García-Fernández R, Díaz-Alejo C. Hemicolectomía en un paciente con valvulopatía aórtica: reporte de caso. Rev Colomb Anestesiol. 2017;45:36–39.