Wheezing and stridor are a frequent reason for consultation, as well as the diagnosis of asthma. Any cases of asthma with failed clinical response to treatment should undergo additional testing leading to differential diagnoses. The case herein presented emphasizes the importance of having a knowledgeable surgical team that interprets lung function tests correctly.
This is a case of a 13-year-old girl who underwent corrective surgery of a right tympanic perforation, with a history of difficult to control exercise-induced asthma. At the time of intubation, Cotton's grade III laryngeal stenosis was identified that required intervention prior to the scheduled procedure. Emphasis shall be placed on the importance of interdisciplinary work when evaluating these patients.
Las sibilancias y el estridor son un motivo de consulta frecuente, así como el diagnóstico de asma. Aquellos casos de asma sin respuesta clínica al tratamiento deben ser estudiados con pruebas adicionales para realizar diagnósticos diferenciales. Presentamos un caso clínico que resalta la importancia de que todo el equipo quirúrgico conozca e interprete correctamente las pruebas de función pulmonar.
Presentamos el caso de una adolescente de 13 años, llevada a cirugía para corrección de una perforación timpánica derecha, con antecedente de asma inducida por ejercicio de difícil control. Al momento de la intubación se encontró una estenosis laríngea grado III de Cotton que fue necesario intervenir antes de realizar la cirugía programada. Resaltamos la importancia del trabajo interdisciplinario en la evaluación de estos pacientes.
Wheezing is described as a constant noise lasting more than 0.25s that is caused by the oscillation of the opposing airway walls. It may occur during inspiration or expiration and may be caused by narrowing of the airway. Stridor is a high-frequency sound caused by air turbulence inside the upper airway. Though wheezing and stridor are clinically different, they are often mistaken.
One of the causes of stridor is laryngotracheal stenosis resulting from an abnormal narrowing along the glottis and the carina. Before 1960 the condition was a congenital etiology, but with the wide use of orotracheal intubation, its incidence rose from 0.9%1 to 24.5%.2 The most frequent benign cause is tracheal intubation and the most frequent malignant cause is squamous cell carcinoma. The most widely accepted stenosis-associated factor following endotracheal intubation is the duration of the intubation. Not withstanding the existing evidence about its relevance, the occurrence of cases after short endotracheal intubations suggests that laryngeal lesions are multifactorial, involving patient as well as intubation-associated factors.3
Furthermore, wheezing secondary to exercise-induced bronchoconstriction is the primary indicator of asthma exacerbations and the last to be resolved.4 In case of an asthmatic patient, a differential diagnosis shall be done between inspiratory symptoms during exercise, typically occurring at the end of the exercise session, and exercise-induced asthma, with onset of symptoms between 3 and 15min after exercise. Finally, the possibility of exercise-induced laryngeal obstruction, associated to adduction of the vocal folds as a secondary phenomenon shall also be kept in mind.5
When studying asthma, the flow-volume curve evidences highly suggestive changes, although it is a rare cause of dyspnea and wheezing during exertion. However, without a clinical suspicion, the symptoms may be confused for asthma. Delays in making the diagnosis may result in increased morbidity.6
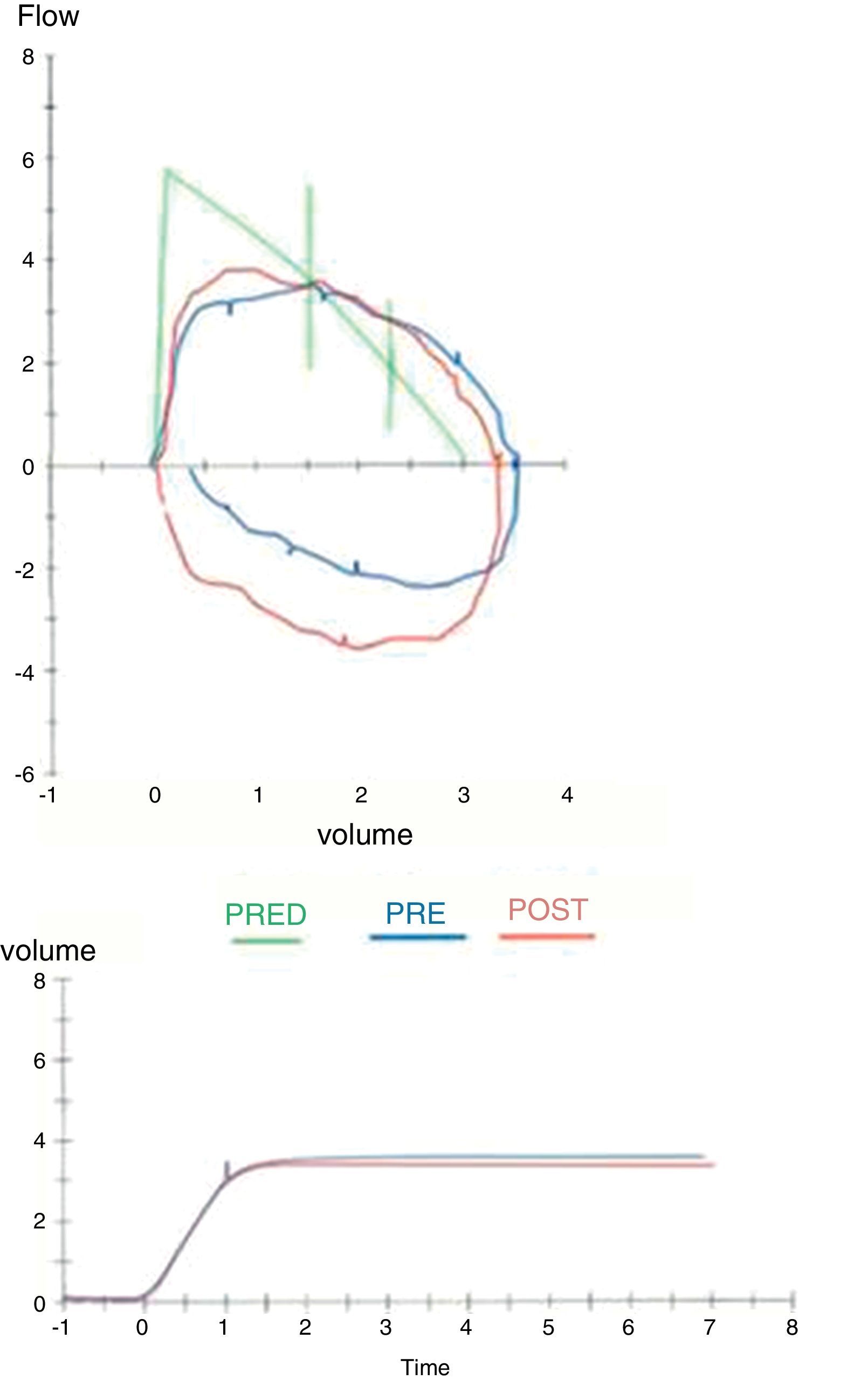
Lung function tests are useful for diagnosing unexplained respiratory symptoms and for monitoring patients with known respiratory disease. Generally speaking, patients over 5 years of age are considered able to cooperate with the proper performance of the procedure. A FVC ratio <70% in adults and <80% in children suggests obstructive pathology and the bronchodilator response must be evaluated. If the FVC is more than 12% between 5 and 18 years of age, or more than 12% and >200ml in adults, a reversible obstruction suggestive of asthma may be considered. However, if these premises are nor met, an irreversible obstruction should be suspected and differential diagnoses must be evaluated.7 When the flow – volume curve is flat, the most frequent cause is submaximal effort, but then a central or upper airway obstruction must be considered.8,9
The Empey10 index has been classically used to assess airway obstruction using spirometry. It measures the ratio between VEF1 (ml) and PEFR (l/min); if the ratio is over 10, this is considered evidence of laryngotracheal stenosis.
Properly diagnosing upper or lower respiratory disease is vitally important in the pre-surgical setting, to prevent unexpected difficult airway cases and getting the surgical team ready to optimize patient outcomes.
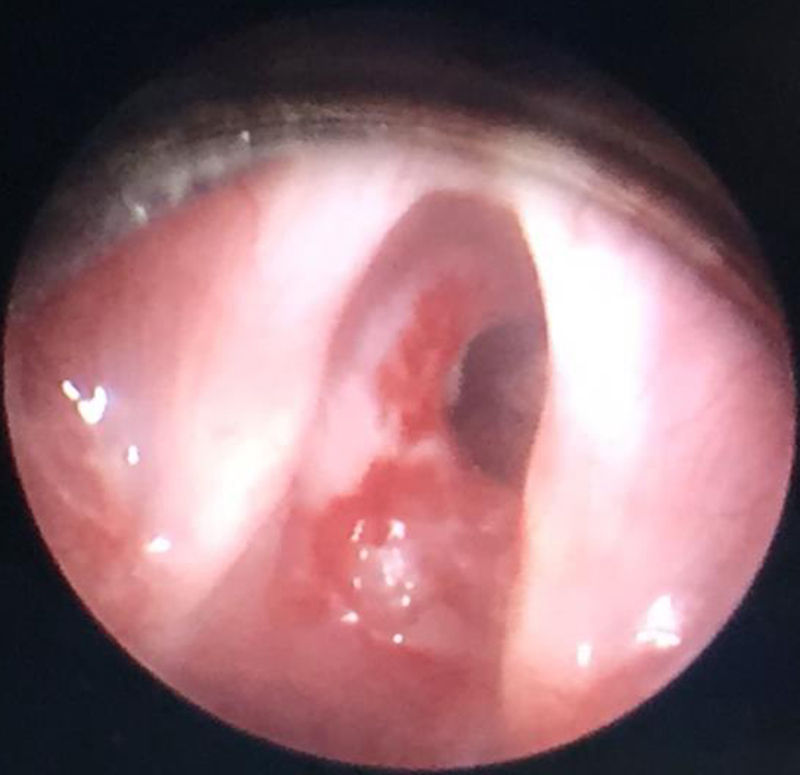
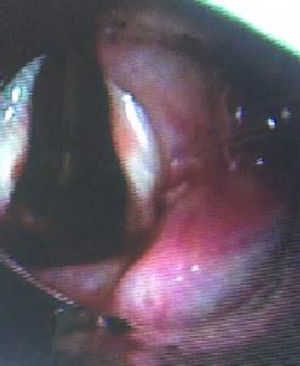
Clinical caseThis case is a 13-year old female patient with a history of patent ductus arteriosus surgically corrected 7 days after birth. The patient did not require orotracheal intubation following the procedure. Additionally, the patient has a history of asthma and is managed with inhaled steroids, with persistent symptoms when she exercises and follow-up by pulmonology. She came to the ENT department of the Fundación Hospital de la Misericordia because of hearing loss and repeated episodes of otitis media during her childhood. A sub-total right tympanic perforation was identified, and the patient was scheduled for type 1 tympanoplasty as an ambulatory procedure. During the pre-anesthesia evaluation, the patient was classified as ASA II because of her history of asthma and continued management was recommended. Following the anesthetic induction, difficulty for intubation with a #6.0 cuffed endotracheal tube was reported, with evidence of subglottic concentric stenosis during laryngoscopy; the anesthetist then switched to a #4.0 cuffed tube. Since the patient was admitted to a high-complexity hospital, she simultaneously underwent laryngeal microendoscopy and bronchoscopy, evidencing a Cotton-Myer III11 concentric subglottic stenosis affecting 70% of the subglottic lumen (Fig. 1), that required laryngeal dilatation and mitomycin and triamcinolone infiltration as per the institutional protocol (Fig. 2). The pre-surgical spirometry was studied, evidencing a curve with discrete flattening of the expiratory peak, reporting all parameters within the normal limits, except for a 60% PEF, with poor response to beta2-agonists (Fig. 3).
DiscussionThe British Thoracic Society12 recommends that unless an alternate diagnosis is more likely, patients with symptoms suggestive of asthma shall be initiated on medical management and further testing is advised if the response is poor.
When clinically evaluating the differential diagnoses, the upper airway obstruction usually involves stridor, contrary to asthma that presents with wheezing. However, there may be some cases that are impossible to differentiate and in the presence of dyspnea and exertion symptoms, may be mistaken for asthma. The upper airway obstruction may be due to altered mobility of the vocal folds (paralysis, paradoxical movement), congenital abnormalities such as laryngeal membranes or vascular compressions, subglottic stenosis for multiple reasons, masses or pressure at the subglottic or tracheal level. Keep in mind that gastroesophageal reflux is one of the conditions most frequently associated with a poor diagnosis of asthma.
Whilst the differential diagnosis may be relatively easy using the flow-volume curve, the Empey11 index and the expiratory disproportion index13 (FEV1[L]/PEFR[L-s]×100) are also helpful. The latter provides a high specificity and sensitivity of >50 for diagnosing laryngotracheal stenosis.
This is a case of asthma refractory to management, with absence of the typical loop curve in spirometry suggestive of subglottic stenosis. The spirometry values reported as normal are probably due to the enormous muscle effort the patient was able to produce as a result of her body size, reaching close to normal levels, affecting only the PEF and hence hindering an accurate diagnosis. The estimated expiratory disproportioned index was 50.4 in this case, indicating a high suspicion of laryngotracheal stenosis. Despite the difficulty in interpretation, the spirometry findings could have been suggestive of the diagnosis, leading to additional airway testing and hence preventing the potential complications of a difficult airway and the emergent surgical management. We believe it is critical that the surgical team as a whole makes an accurate interpretation of pulmonary functional tests during the pre-anesthesia and pre-surgical evaluation, in all patients with a diagnosis of asthma.
ConclusionsA delayed diagnosis of laryngotracheal stenosis may affect up to 10% of patients, increasing the respiratory morbidity and the risk of respiratory failure.14 Notwithstanding the fact that this is a low frequency disease among the general population, this case reminds us of the need to be suspicious in case of a diagnosis of asthma refractory to management and it is the duty of the surgical team as a whole, to be aware of the interpretation of the spirometry for early identification of any laryngotracheal stenosis cases and to prevent any anesthesia or surgery-associated complications. In accordance with the recommendations of the British Thoracic Society,12 the authors believe that any patient with a questionable diagnosis of asthma, particularly in the case of exercise-induced asthma, and with a history of previous intubations, requires an evaluation of vocal folds’ movement and subglottic patency. A judicious preoperative evaluation must comprise this aspect. In this particular case, both pathologies were simultaneously treated, since the patient was admitted to a high complexity pediatric hospital; however, in a different setting, probably the outcome would have been less favorable.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingNo external funding was involved in the development of this publication.
Conflicts of interestThe authors have no disclosures to make.
Please cite this article as: Marrugo-Pardo G, Villalobos-Aguirre MC. La confusión entre asma y estenosis subglótica puede causar un evento adverso en la intubación. Reporte de un caso. Rev Colomb Anestesiol. 2017;45:82–85.