The way neurosurgery has evolved has led to increased emphasis on anaesthetic techniques aimed at improving patient well-being. In the United States alone, the number of neurosurgeries has increased significantly, with growth reflected in approximately 12,000 spine procedures per year and another 2700 different neurosurgical procedures per year. For anaesthetists, this means that they are faced more frequently with the need to select the most adequate neuroanaesthesia technique for each patient.
ObjectivesThe purpose of this review is to analyze the role of inhaled and intravenous anaesthetics in neurosurgical procedures.
MethodologyA search was conducted in PubMed using the terms TIVA, inhaled anaesthetics, neurosurgery and spine surgery.
ResultsThe articles included in the review show that the adequate anaesthetic technique, besides ensuring a rapid onset of action, contributes to ease of titration with minimum effect on systemic and cerebral haemodynamics; it must enable intraoperative neurophysiological monitoring and rapid emergence, in order to allow early assessment of the patient's neurological function and improved outcome.
ConclusionsIn recent years, the question regarding the use of inhaled vs. intravenous anaesthetics in neurosurgery has given rise to several research studies. Although TIVA is the technique used most frequently, inhaled anaesthetics have also been shown to be safe, titratable, and to provide for adequate intraoperative monitoring and cerebral haemodynamic stability. In patients with normal intracranial compliance, inhaled agents (IA) are a good alternative to TIVA, especially in places where hospital resources are limited.
La evolución en neurocirugía ha fomentado las técnicas anestésicas en pro del bienestar del paciente. Solo en Estados Unidos el volumen de neurocirugías ha aumentado de forma significativa, mostrando un crecimiento aproximado de 12.000 procedimientos de columna al año, y de otros procedimientos neuroquirúrgicos de 2.700/año. Esto enfrenta con mayor frecuencia a los anestesiólogos a la elección de la técnica neuroanestésica adecuada para cada paciente.
ObjetivosEsta revisión pretende realizar un análisis del rol de los anestésicos inhalados e intravenosos en procedimientos neuroquirúrgicos.
MetodologíaSe realizó una búsqueda en PubMed utilizando TIVA, anestésicos inhalados, neurocirugía y cirugía de columna como términos de búsqueda.
ResultadosLos artículos revisados muestran que, la técnica anestésica adecuada, además de tener un rápido inicio de acción, ser fácilmente titulable, con mínimo efecto en la hemodinámia sistémica y cerebral; debe permitir monitorización neurofisiológica intraoperatoria, y un rápido despertar, con el fin de permitir una evaluación temprana de la función neurológica del paciente y mejorar su desenlace.
ConclusionesDurante los últimos años la disyuntiva del uso de anestésicos inhalados versus intravenosos en neurocirugía ha producido el desarrollo de diversas investigaciones. Aunque TIVA es la técnica usada con mayor frecuencia, los anestésicos inhalados, también han mostrado ser seguros, titulables, proveer una adecuada monitorización intraoperatoria, y estabilidad hemodinámica cerebral. En pacientes con complacía intracraneal normal los agentes inhalados, son una buena alternativa a la anestesia con TIVA, especialmente en lugares con recursos hospitalarios limitados.
Trends in anaesthetic practice have evolved over the past 20 years. In 2007, the most frequent types of neurosurgical procedures were spinal fusion, endovascular spinal procedures, craniotomies for tumour pathology, craniotomies not associated with tumour pathology, and intracranial endovascular procedures (54%, 20%, 11%, 9% and 1%, respectively).1 Just like other areas of medicine, neurosurgery is also moving towards minimally invasive procedures, and there is current evidence of a 32% growth in intracranial endovascular procedures in 2013.1
In daily clinical practice, anaesthetists are increasingly faced with the need to provide anaesthesia to neurosurgical patients because, in order to preserve neurological functions, it is critical to assess the effect of inhaled or intravenous anaesthetics during the procedure, as well as the time and quality of the recovery.
A topic that has created quite a lot of debate is which is the best anaesthetic method for these types of patients with cerebral and spinal pathologies as well as head injury. Anaesthetic management is a critical issue during those procedures. Ensuring haemodynamic stability is fundamental in order to preserve cerebral autoregulation2. One of the factors affecting cerebrovascular autoregulation is partial CO2 pressure (PaCo2), where a 1mmHg change may result in changes of up to 3–4% in cerebral blood flow (CBF).1
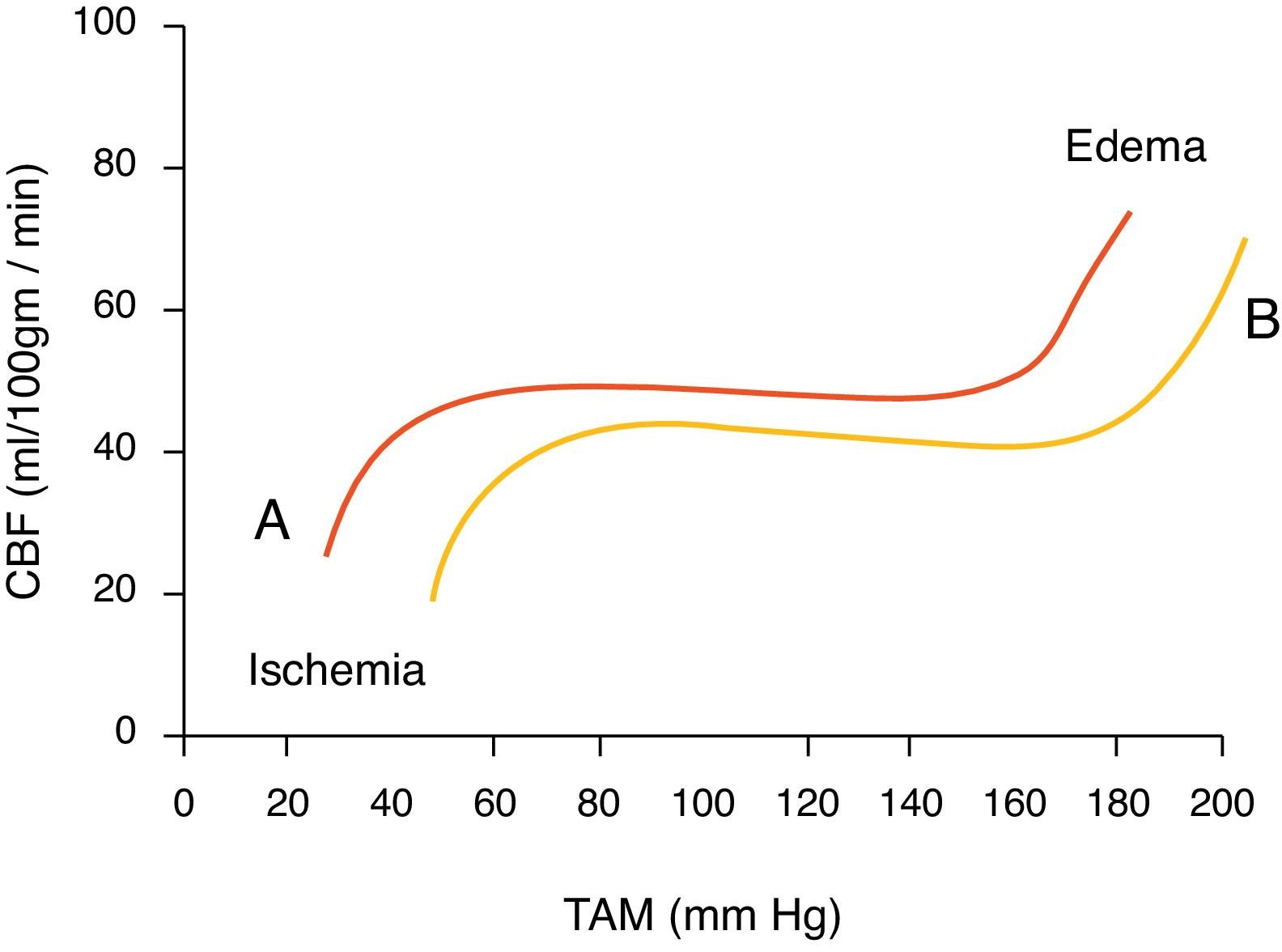
Together with PaCo2, mean arterial pressure (MAP) plays a very important role as well, and must remain in the range of 60–150mmHg (Fig. 1).2 When fluctuations occur in these ranges, different counter-regulation mechanisms are activated, including the renin-angiotensin-aldosterone system and the sympathetic nervous system in order to bring blood pressure (BP) back to normal.3
This autoregulation is lost as a result of different circumstances: severe brain injury, tumours, haematomas, space occupying lesions in the cranial vault, infections, increased systemic arterial pressure, etc.2
The ideal anaesthesia for neurosurgical procedures must have the following characteristics: reduction of cerebral metabolism, neuroprotection, haemodynamic stability, preservation of cerebral autoregulation, only mild effect on intracranial pressure (ICP), and fast patient recovery.4 The effects of anaesthetic drugs on each of these characteristics have been studied at length.
Two modalities are in use at the present time: total intravenous anaesthesia (TIVA) and inhaled anaesthetics (IA). They both have advantages and drawbacks, as will be explained below.
Total intravenous anaesthesiaThe term TIVA is applied whenever a hypnotic agent (propofol) is used in combination with an opioid for anaesthesia induction and maintenance. One of the most commonly used combinations is propofol with remifentanil because it has similar characteristics to the use of IA.5
Propofol potentiates GABAA receptor activity has a rapid onset of action and it is very short acting. It has a neuroprotective effect during cerebral ischaemia, lowering ICP, CBF, cerebral metabolism and oedema, and improving cerebral perfusion pressure (CPP) and MAP.6–8
Inhaled anaestheticsAIs have been shown to reduce excitotoxicity, increase physiological stability and have an association with good neurological outcomes. This effect is mediated by their GABA agonist and NMDA antagonist activity and is also related to glutamate reduction, activation of ATP-dependent potassium channels, reduction of cerebral metabolic rate (CMR), positive regulation of nitric oxide synthase and proapoptotic regulating factors (PI3K-AKT, MAPK/ERK, p38).4,9 AIs produce a dose- and agent-dependent cerebral autoregulation effect.10 With a MAP between 70 and 150mmHg, the effect of inhaled anaesthetics on CBF is acceptable, but at higher values there is an exponential increase in CBF, which could result in an increase in ICP.
At a dose of 1 minimum alveolar concentration (MAC) there is a balance between the drop in CMR and the increase in CBF. At >1 MAC doses, CBF increases and CMR values remain low. In ascending order, the vasodilation potential is sevoflurane<isoflurane=desflurane<enflurane ≪ halothane. Generally, in patients with normal intracranial compliance, the effect of IA on brain haemodynamics is negligible. TIVA is preferred in patients with an altered flow/metabolism ratio, unstable ICP, expansive or large lesions.7,11
Intracranial pressureTIVA has very important characteristics for intracranial procedures, but it has limitations that need to be borne in mind when considering its use.5
- (1)
It must be used by experienced anaesthetists. Propofol accumulation may delay emergence from anaesthesia; similarly, if plasma levels are not optimal, the patient may experience intraoperative awakening.
- (2)
Propofol infusions may lead to the development of rhabdomyolysis, lactic acidosis and renal failure.
- (3)
It may induce a substantial reduction of cerebral blood volume, leading to complications such as epidural bleeding.
- (4)
TIVA is substantially more costly than IA.
Different studies have compared the two anaesthetic methods in intracranial procedures. Todd et al.12 measured pressures in the epidural space, and found no significant difference in ICP between the two groups (isoflurane-nitric oxide versus propofol-fentanyl). However, they found rapid anaesthesia recovery and a higher incidence of post-operative nausea and vomiting (PONV) in the TIVA group. Petersen et al.13 assessed both anaesthetics in the subdural space during elective craniotomies for supratentorial tumours. ICP was much higher in the patients who received TIVA. Later, they showed that the use of hyperventilation lowered ICP significantly in patients treated with IA.14
There are also studies supporting the use of IA. In neurosurgical patients, desflurane has been shown to have shorter extubation and recovery time compared to sevoflurane and isoflurane.15–17 Another important factor to consider is the prevention of blood hypertension during surgical closure and emergence; in this regard, low doses of fentanyl have shown to be better than propofol and isoflurane.18 Other advantages of IA have also been shown: less coughing, which avoids considerable ICP increases19; better cardiovascular stability over TIVA, preserving left ventricular relaxation and, consequently, maintaining a stable CBF.
In a study in patients taken to intratentorial intracranial surgery, no significant difference was found in the incidence of PONV between TIVA and sevoflurane.20 In a systematic review conducted later in 821 patients, the results were similar, showing more PONV and greater use of anti-emetics in patients treated with sevoflurane.21 A meta-analysis with 1819 patients undergoing elective craniotomy showed a lower incidence of PONV in patients managed with propofol.22
Spinal surgeryIntraoperative electrophysiological monitoring (IEM) plays a key role in continuous monitoring of neuronal integrity and function of the neuronal structures at risk during the surgical procedure. In patients taken to spinal surgery, factors such as instrumentation, surgical manipulation, hypervascularity and hypercoagulability increase the risk of complications such as permanent neurological damage. IEM allows for early detection and correction of potentially reversible damage. It is indicated for the correction of congenital spinal abnormalities, correction of scoliosis with angles greater than 45°, intra- and extramedullary tumour resection, and spinal stenosis decompression.23–27
At the present time, somatosensory evoked potentials (SSEP) and motor evoked potentials (MEP) are part of the standard neurosurgical protocol.28 MEPs have shown a better correlation with motor function and also greater sensitivity to spinal cord perfusion abnormality, ischaemia and hypothermia.29–31
In order to obtain adequate SSEP and MEP it is important to use an anaesthetic technique which does not suppress or alter their amplitude or latency32. In general, the most sensitive neurological pathways to physiological and pharmacological changes are the longer ones and those with larger synapses. Frequently, signals from the lower limbs are more difficult to record than those coming from the upper limbs.8
In surgery for epidural spinal cord tumours, Avila et al.23 found that preserved IEM signals suggest good neurological outcome. Changes in the SSEP amplitude and latency signals may be indicative of neurological damage onset, and must prompt the surgical team to check the effect of anaesthesia, instrumentation, blood pressure and temperature.23
IAs have been shown to suppress MEP as well as to reduce the amplitude and prolong the latency of the SSEP in a dose- and agent-dependent fashion, the most potent agents being isoflurane and sevoflurane.33 In scoliosis surgery, an MAC of up to one has shown to be compatible with monitoring. Moreover, when comparing desflurane and TIVA,8,34 MEP amplitudes have shown to be significantly greater in patients anesthetized with desfluorane (p>0.0001). Recently, Sloan et al.35 compared the effect of TIVA and 3% desflurane on evoked potentials of patients undergoing spinal surgery. No significant difference was found in SSEP and transcranial electric MEP (TCe-MEP) or stimulation voltages of TCe-MEP between the two groups. In paediatric patients taken to vertebral arthrodesis, Clapcich et al.36 showed that propofol-based TIVA is better than isoflurane as monotherapy, or isoflurane plus nitrous oxide in preserving SSEP.
IAs have shown to be a confounding factor in the interpretation of TCe-MEP, considering that they increase false positives in spinal surgery patients. This leads to changes in the approach and surgical time, and to the administration of unnecessary medications.37
En general, TIVA makes it easier to perform IEM. In surgeries like vertebral arthrodesis, dexmedetomidine has not shown to alter TCe-MEP significantly when given at a dose of 0.4ng/ml; however, at higher doses, it has been shown to interfere with TCe-MEP, because it attenuates its amplitude.38,39 Opioids produce a slight increase in latency and a slight reduction in MEP and SSEP amplitude.7,33,36,40–42
Important also in the anaesthetic management during spinal surgery is to use an agent that provides for adequate haemodynamic stability, adequate recovery, low PONV incidence, and adequate pain management. For this procedure, propofol and desflurane have shown to maintain better haemodynamic stability when compared to isoflurane.43,44 Moreover, propofol has shown to increase blood flow in paravertebral muscles without an increase in blood loss or bleeding perceived by the surgeon.45
In cervical spine surgery, the incidence and severity of coughing are lower in patients managed with propofol when compared to sevoflurane.46 However, in patients undergoing spondylolisthesis, a lower incidence of coughing and lower scores in the visual analogue scale (VAS) has been documented in the group receiving sevoflurane anaesthesia.47 The probability of coughing has been shown to depend on the residual concentration of the anaesthetic at the time of extubation, and is significantly higher in elderly patients. This has led some authors to recommend the use of TIVA in patients with a high risk of post-operative coughing, in order to prevent potential complications.47
Traumatic brain injuryTraumatic brain injury (TBI) is highly prevalent in the world. In the United States, it affects 1.4 million patients every year; in Colombia, mortality due to TBI is 14% and occurs in 51.2% of patients involved in traffic accidents.48,49 TBI often produces permanent neurological damage.11
Grathwohl et al.11 compared TIVA with IA in the surgical management of TBI in the combat setting. Mortality was found to be lower (5% vs. 16% p=0.02) in patients managed with TIVA, but no relationship was found between TIVA and better neurological outcomes.
ConclusionNeuroprotection is the cornerstone of anaesthetic management in neurosurgery. The review of the literature shows that both anaesthetic modalities have neuroprotective properties. TIVA is currently used more frequently in neurosurgery because of the fast onset of action and the ability to monitor neuronal structures continuously using intraoperative neurophysiological monitoring techniques. It is important to highlight that in patients with adequate intracranial compliance, the use of an IA dose equal or less than 1 MAC has not only shown minimal interference with autoregulation of cerebral blood flow, cerebral blood volume and ICP but also compatibility with intraoperative physiological monitoring in the usual neurosurgical setting. The selection of the appropriate anaesthetic agent in neurosurgery depends on the risk factors inherent to the patient and the procedure. It is essential to maintain a balance between CBF and metabolic demand, blood pressure and cerebral haemodynamics during the procedure, avoiding sudden changes of these parameters that might influence the patient's neurological outcome. It seems common sense to think that a combined technique with TIVA and inhaled agents may be easy to titrate, may allow to combine the neuroprotective effect of both agents, and reduce the anaesthetic dose used. Studies focused on finding the ideal anaesthetic technique for neurosurgery are still required.
Conflict of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Zuleta-Alarcon A, Castellon-Larios K, Mejía MCN-d, Bergese SD. Anestesia total intravenosa versus anestésicos inhalados en neurocirugía. Rev Colomb Anestesiol. 2015;43:9–14.