Shoulder fracture is one of the most frequently treated injuries in trauma centers, with an overall incidence that appears to have increased in recent years, ranging from 219 to 419 cases per 100 000 person-years.
In clinical terms, shoulder girdle injury is difficult to diagnose due to the close relationship between the shoulder and the chest, and imaging identification of the different types of injuries can be challenging.
In this context, X-rays are the most appropriate method and the cornerstone of the initial approach to shoulder trauma, and at least 3 views are recommended: true anteroposterior view (AP), axial or axillary projection or modified axial projection (Velpeau view), and lateral scapula shoulder or Y view. However, patient positioning is often problematic due to the additional pain associated with limb mobilization in order to achieve the proper position for radiographic projection.
The following is the description of a technique for performing an axial shoulder projection that is free of these complications, easy to standardize, and applicable to any traumatic or degenerative disease of the proximal humerus or glenohumeral joint, which, to the best of the authors’ knowledge, has not been previously published.
El trauma de hombro es una de las patologías más frecuentemente vista en los centros de trauma con una incidencia global que aparentemente ha aumentado en los últimos años y que se ha reportado entre 219 a 419 casos por 100000 personas-año.
El diagnóstico del trauma de la cintura escapular no es fácil clínicamente por la íntima relación entre el hombro y el tórax, y la identificación imagenológica de las distintas lesiones puede ser desafiante.
Las radiografías son el método más apropiado y piedra angular del estudio inicial en el trauma de hombro, el set de trauma tiene al menos 3 planos: la vista Anteroposterior (AP) verdadera, una proyección axial o axilar o su modificación descrita por Velpeau. Y una proyección Y de escápula. Sin embargo, el posicionamiento del paciente muchas veces no es fácil por el dolor adicional que puede generar la movilización de la extremidad para lograr la posición adecuada para la proyección radiográfica.
Describimos una técnica para realizar una proyección axial de hombro sin estas dificultades, fácilmente estandarizable para cualquier patología traumática o degenerativa del húmero proximal o de la articulación gleno-humeral y que creemos no ha sido publicada previamente.
Shoulder fracture is one of the most frequently treated injuries in trauma centers.1 Its incidence is difficult to determine since patients with low-grade rotator cuff tears and acromioclavicular joint sprains do not always seek medical attention immediately.2
Epidemiologically, shoulder girdle trauma has a bimodal distribution, with a higher prevalence in young men and older women. Around half of the injuries occur in soft tissues, while 35% are fractures and 17% are dislocations, with an overall incidence that appears to have increased in recent years, ranging from 219 to 419 cases per 100,000 person-years,1,3,4. It is possible to find cases with involvement of bone tissue such as the clavicle, scapula, or proximal humerus, as well as soft tissue such as the rotator cuff, ligaments, or labrum-ligament complex.
In clinical terms, shoulder girdle injury is difficult to diagnose due to the close relationship between the shoulder and chest, and imaging identification of the different types of injuries can be challenging 1,5. Consequently, imaging assessment should start with a plain x-rays that may progress to a scan or magnetic resonance imaging if diagnostic suspicion exists. In this context, ultrasonography has limited utility, particularly in the case of deep tissue injury. CT angiography or traditional arteriogram may also be indicated in some cases. 2,6
Treatment options may range from conservative orthopedic management to emergency surgery1,2, which is determined based on an adequate clinical history and a thorough radiological and imaging evaluation. Therefore, an effective X-ray acquisition technique is required for the comprehensive assessment of these patients,2,7 as it allow performing a complete evaluation of the bone anatomy and identifying fractures and joint relationships2,5,7.
Since X-rays are the most appropriate method and the cornerstone of the initial approach to shoulder trauma, at least 3 views are recommended: standard anteroposterior view (AP), axial or axillary projection or modified axial projection (Velpeau view)2,5,7–12. In cases of acromioclavicular joint damage, the Zanca projection with a 10-15 cephalad angle should also be used5,13. Glenohumeral and acromioclavicular luxation may be difficult to recognize with an AP view alone; thus, axial or axillary projections, as well as lateral scapula or Y projections, are required in these instances.2,9
Regarding technical considerations, X-rays should be taken in erect posture, as supine positioning may result in an under-representation of malalignment 2,5,7. However, patient positioning is often problematic due to the additional pain associated with limb mobilization in order to achieve the proper position for radiographic projection.
X-rays are preferred over CT scans during the initial assessment of the patient because the former is faster, less expensive, and capable of adequately diagnosing fractures and changes in joint relationships, which are of primary concern to the emergency service, and in many cases, even allows for classification of the injuries.2,11.
The axial projection of the series of radiographs recommended for the adequate evaluation of proximal humerus or glenohumeral joint trauma is usually not performed by X-ray technicians due to the difficulty in performing it in patients with post-trauma pain, so some alternatives to conventional X-rays have been described, including the Horsfield-Jones projection12, the axial wheelchair projection14, the Ciullo15 or Clements view16, the Garth17 view, among others.
Two techniques are frequently reported in the literature: 1. The Velpeau projection, described by Bloom and Obata in 1967,9 which involves positioning the patient in hyperextension of the lumbar spine on an X-ray table; however, this technique is extremely difficult to perform on small patients; and 2. abduction of the affected arm, which is not possible in patients with dislocation or fracture.
The following is the description of a technique for performing an axial shoulder projection that is free of these complications, easy to standardize, and applicable to any traumatic or degenerative disease of the proximal humerus or glenohumeral joint, which, to the best of the authors’ knowledge, has not been previously published.
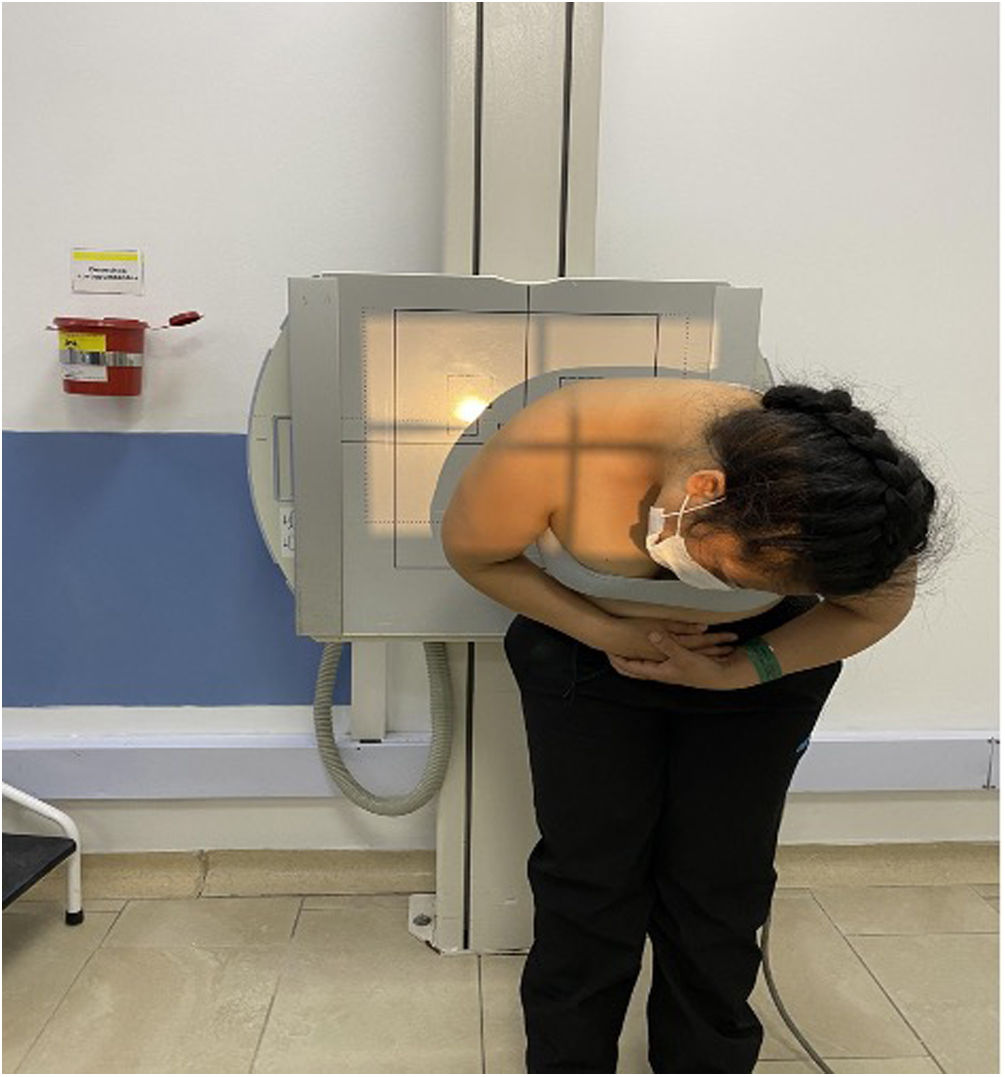
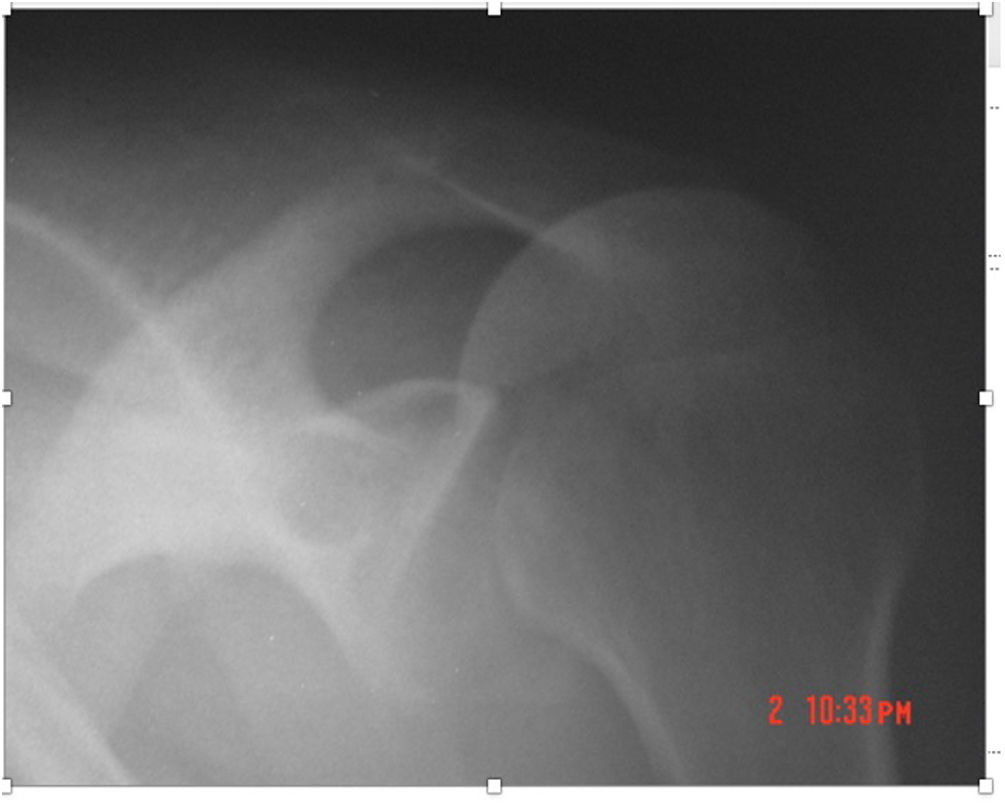
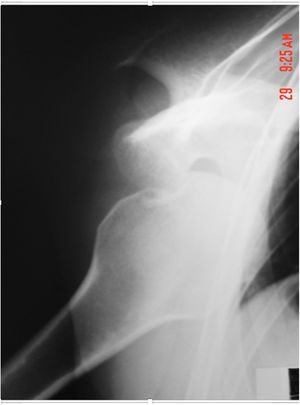
TechniqueThe X-ray cassette used in a conventional chest X-ray is placed; the trunk is flexed 60 degrees; the beam is focused on the shoulder (Figures 1-2); the head is tilted to the contralateral side, away from the affected shoulder, as shown Figure 2; and the RX emitter is placed approximately 150 centimeters away from the patient. In this manner, the patient keeps the limb close to the trunk and the shoulder sling is not removed. It should be noted that this projection produces a magnified image of the joint due to the distance between the shoulder and the cassette.
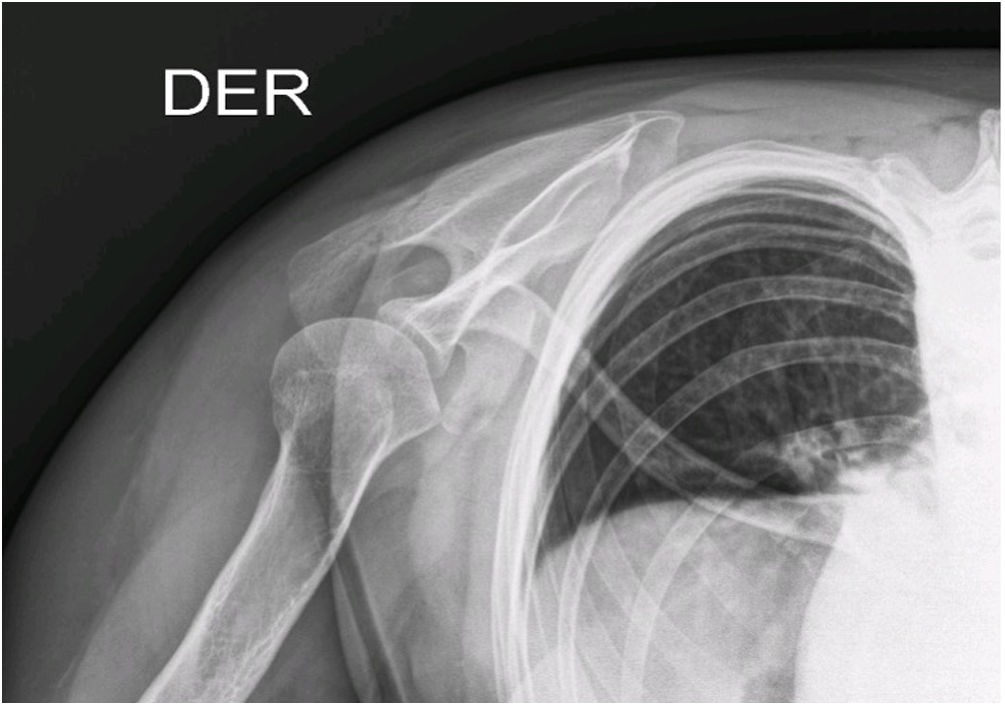
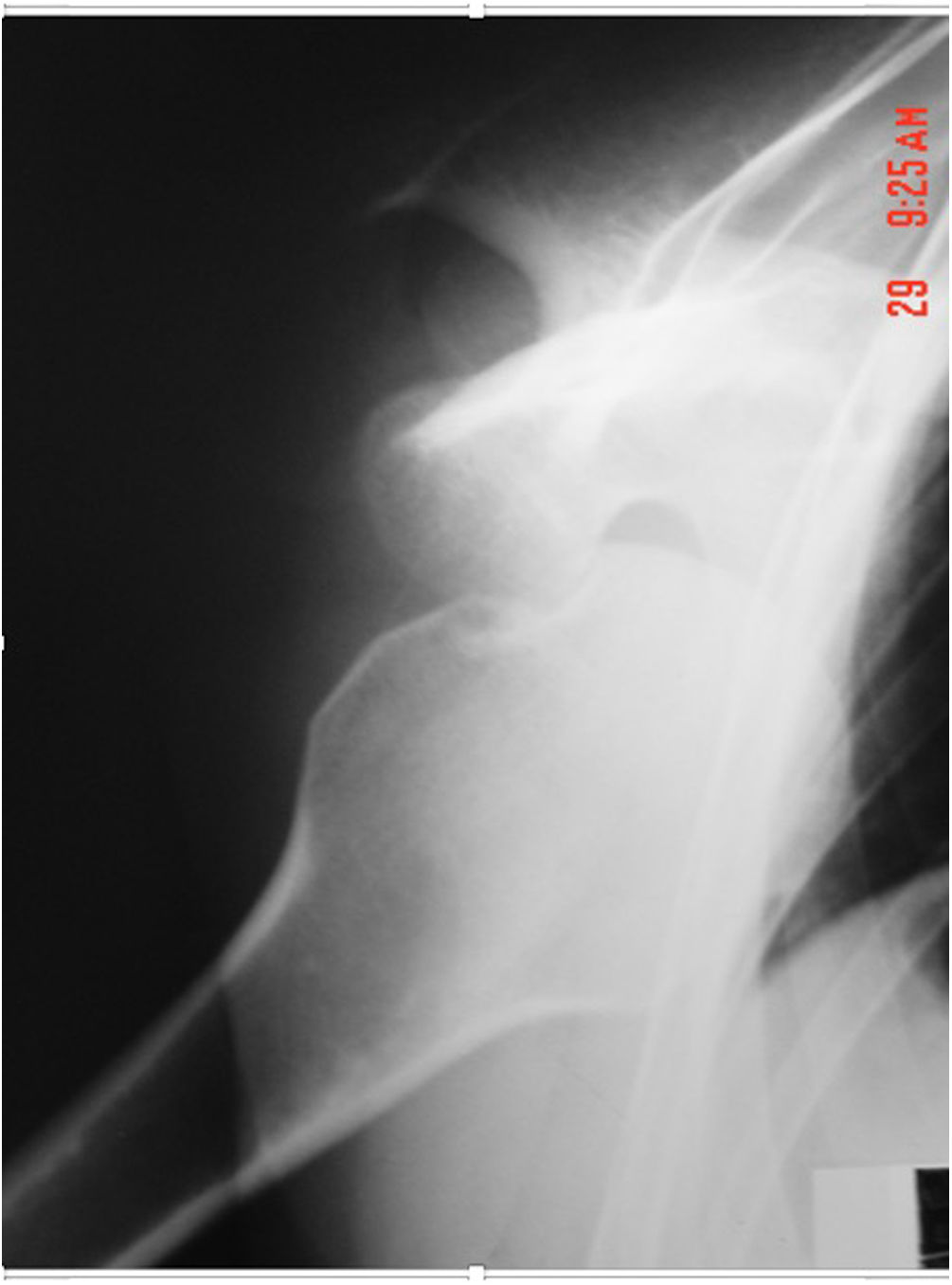
Axial views obtained using this technique are similar to the true axial projection and all anatomical structures of interest are easily identified. Figure 3 shows a normal shoulder, Figure 4 depicts an anterior shoulder dislocation, and Figure 5 depicts a posterior shoulder dislocation.
To accurately assess shoulder injuries, at least three X-ray views are required, particularly in cases of posterior shoulder dislocation. The technique outlined here is easily reproducible, causes little discomfort to the patient, and allows for a proper diagnosis of any type of dislocation.