To establish the occurrence of caregiver syndrome in caregivers of people with mental illness participating in the day hospital programme of a tertiary institution in the city of Cali.
Material and methodsA descriptive, cross-sectional observational study was carried out to evaluate the occurrence of overload syndrome in 70 caregivers of people with mental illness, through interviews and the formal application of the Zarit scale and the WHO-DAS 2.0 questionnaire.
ResultsIt was established that 68.6% of the participating population presented some level of overload. The caregiver profile corresponds to women, over the age of 55, who belonged to the subsidised health system; earning a low income, and with an average of 8 years in caregiver role for at least 12 hours per day. The long time dedicated to the role's activities and the level of demand resulting from the degree of disability of the person receiving care, appear as associated factors for the presence of higher levels of overload for the caregiver, for which they are a factor to consider when implementing interventions and research processes in which the caregiver is involved as a key agent for improving the quality of life of people with mental illness.
Establecer la ocurrencia del síndrome del cuidador entre los cuidadores de personas con enfermedad mental vinculadas al programa de hospital de día de una institución de tercer nivel de la ciudad de Cali (Colombia).
Material y métodosSe realizó un estudio descriptivo y observacional de corte transversal, para evaluar la ocurrencia del síndrome de sobrecarga en 70 cuidadores de personas con enfermedad mental, a través de entrevistas y la aplicación formal de la escala de Zarit y el cuestionario WHO-DAS 2.0.
ResultadosSe estableció que el 68,6% de la población participante presenta algún grado de sobrecarga; el perfil del cuidador es el de una mujer, mayor de 55 años, madre de familia, perteneciente al régimen subsidiado de salud y con bajo ingreso económico que, en promedio, lleva 8 años ejerciendo el rol de cuidador por lo menos 12h diarias. El largo tiempo de dedicación a las actividades propias del rol y el nivel de demanda, producto del grado de discapacidad de la persona a la que se cuida, aparecen como factores asociados a la aparición de un mayor grado de sobrecarga para el cuidador, por lo que constituyen un factor que considerar en la implementación de procesos de intervención e investigación que vinculen al cuidador como agente clave en el mejoramiento de la calidad de vida de las personas con enfermedad mental.
In families caring for a family member with an illness, the role of carer arises. In the particular case of mental health, this carer plays a determining role in ensuring adherence to psychosocial rehabilitation processes, contributing to decision-making by establishing mechanisms by which the person with mental illness can participate.1,2 However, since this role negatively impacts occupational performance due to the high demands in terms of time and effort, carers face constant stress, anxiety and despair, which have a direct impact on their productivity and ability to adapt to life situations; these symptoms constitute caregiver syndrome.1,2
In recent years, this condition has been a common issue in services caring for users with mental illnesses, giving rise to bases for different research and intervention processes. In this case, from occupational therapy, we seek to estimate the direct consequences of performing the role of carer and their relationship with the psychosocial rehabilitation processes of users attending the day hospital programme.
Informal or family carers assume the responsibility of providing basic care to the person with mental illness and are one of the main sources of social and emotional support when living with such a condition (2).
Being a part of the immediate context in which the person is living, the family member plays a leading role in inclusion processes from the point of view of social and community participation and home dynamics, regardless of the diagnosis of mental illness. The involvement of the family group in processes relating to mental illness has psychological consequences associated with high stress levels for all members of the family.3 Therefore, ensuring the well-being of the family and carers galvanises adherences to psychosocial rehabilitation programmes, in which current knowledge of the illness, attitudes towards the person with mental illness and practices that can encourage or foster occupational performance in activities of daily living or participation in social and community settings are prioritised.2,3
In the direct relationship between the carer and the person with mental illness, it is possible to identify a predisposition to vulnerabilities or psychosocial alterations associated with symptoms of personal suffering, frustration, stress, reduced social interaction and even depression and loss of self-esteem. These situations can lead to the development of caregiver syndrome, which reduces both the carer's ability to enjoy their day-to-day life and the mechanisms by which they face and adapt to everyday demands.2
In a country like Colombia, an estimate is needed of the impact that the role of carer can have on the quality of life of family members who assume responsibility for providing emotional support and assistance with carrying out activities of daily living, as well as serving as an intermediary between the person with mental illness and the entities providing healthcare services.2–4 Although there is some previous research on the role of the carer, it exists primarily in the fields of neurology and geriatrics, as well as isolated cases of mental illness such as bipolar disorder, schizophrenia and some forms of dementia.5–9 There are still gaps in the research in the field of mental health when it comes to estimating the well-being and quality of life of carers in the population with long-term conditions and a high level of dependence, as well as evidence of the perceived needs and mechanisms to meet those needs, based on their experience and the established link with healthcare services such as day hospital programmes, community mental health strategy and hospital management.
The objective of this study was to establish the incidence of overload syndrome among carers of people with mental illness linked to the day hospital programme of a tertiary institution in the city of Cali (Colombia). The research was conducted from the perspective of the relationship, including the galvanising effect of the carer on psychosocial rehabilitation processes in a group of people who regularly attend the day hospital programme.
Material and methodsA descriptive, observational, cross-sectional study was conducted to determine carer overload and estimate the general characteristics of 70 carers of people with mental illness linked to the programme of the Day Hospital Centre (DHC) of the Hospital Psiquiátrico Universitario del Valle [Del Valle University Psychiatric Hospital] (HPUV) in the city of Cali, Colombia.
The inclusion criteria were: men and women over 18 years of age caring for people with mental illness who were actively linked to the day hospital programme during the period from November 2015 to June 2016. The exclusion criteria were: professional carers with a contract-based working relationship and hospitalisation of the person with mental illness in the last 30 days.
The study sample was chosen for convenience, with all carers of users of the programme invited. This was a total of 75 people. Information was obtained from 70 carers, a response rate of 92% of the DHC's beneficiaries.
Personal contact was established to introduce the project and obtain the signature of the informed consent. The Zarit scale1,8 was used as a tool to determine the presence of caregiver overload syndrome. It has been validated in the Colombian setting, with an established reliability of 0.81, attesting the relevance of the application of this test in the Colombian population.1 According to the guidelines included in this version of the scale, overload levels should be understood based on the score obtained, interpreting scores <24 “no burden”; between 24 and 33 as a “mild burden”; and ≥24 as a “severe burden”.
In addition, the World Health Organization Disability Assessment Schedule 2.0 (WHO-DAS 2.0) was used to determine the burden of disability of the person with mental illness. This tool has a transculturally adapted Spanish version and allows the degree of disability to be described independently of the clinical diagnosis.10,11 It has been used in Colombia to assess the variable in individuals with a history of spinal trauma12 and injuries with external causes such as accidents and suicide attempts13.
Statistical analysisA univariate analysis was carried out in order to verify the behaviour of the data and form a descriptive estimate of the variables of interest, summarised based on measures of central tendency (mean, median) and dispersion depending on the nature of the data. A bivariate analysis was performed to identify possible relationships between the outcome variable and the exposure variables. Based on a bootstrapping process for 500 random samples, statistical tests were used in accordance with the nature and distribution of the data and processed using the SPSS version 21 for Windows® statistical software.
Ethical considerationsIn conducting the study, the ethical principles set out in the Declaration of Helsinki and Colombian Ministry of Health Resolution 8430 of 1993 were taken into account.
The study was a minimal risk research study under the aforementioned Resolution. The research protocol was submitted to the Ethics Committee of the Universidad del Valle for assessment and received its endorsement. To minimise risk, the questionnaires were administered in the presence of personnel who had received prior training.
As established in the informed consent form, the confidentiality of the information was guaranteed by assigning codes to the participants and the right to withdraw at any stage of the study was respected.
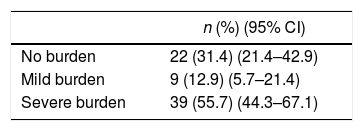
ResultsBetween November 2015 and June 2016, 75 carers of people with mental illness who attended the Hospital Psiquiátrico Universitario del Valle's DHC programme were invited to participate, with 70 choosing to do so. Table 1 summarises the incidence of caregiver overload syndrome; it can be seen that 68.6% (n=48) of the study sample presented some degree of caregiver burden. The presence of a mild burden in 12.9% (95% confidence interval [95% CI]: 5.7–21.4) means this is a factor that should be taken into account by the programme, as it suggests that this group of people is exposed to risks that could lead to physical or psychosocial morbidity, which are key elements in determining the presence of a severe burden.
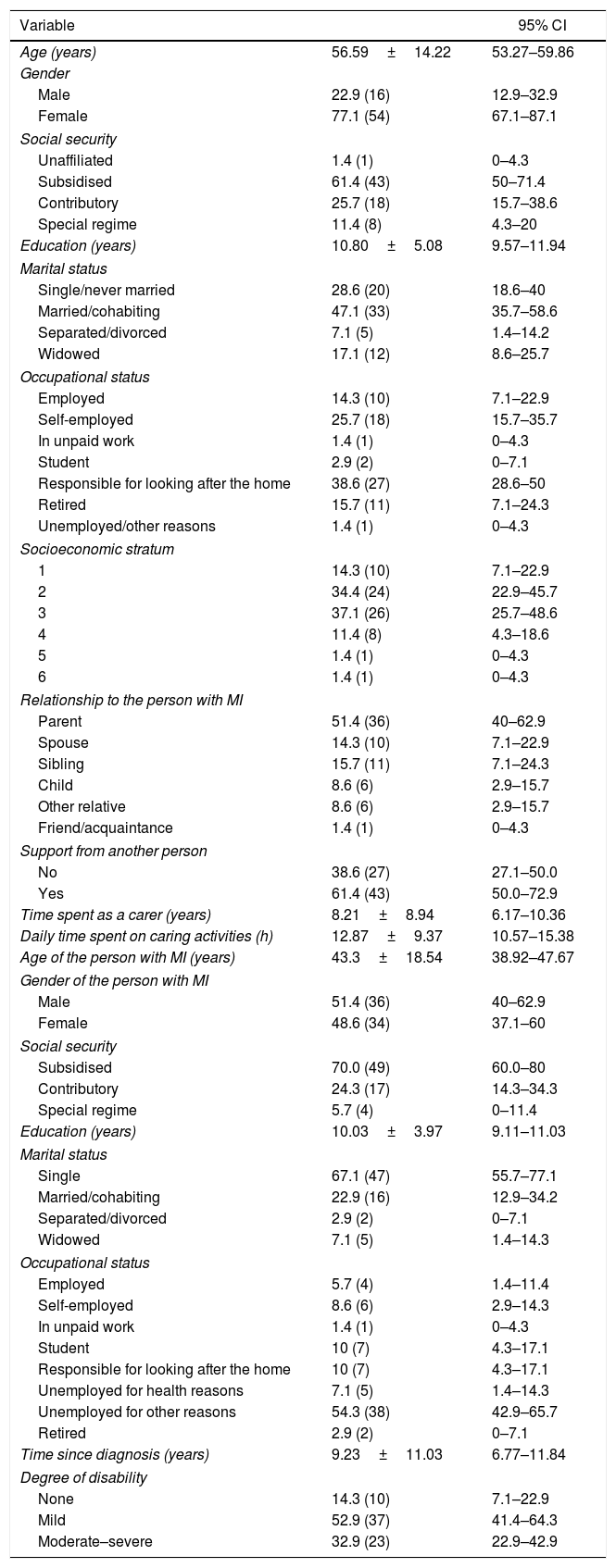
Table 2 summarises the sociodemographic characteristics of the carers and individuals with mental illness participating in the study.
Sociodemographic characteristics of the carers and people with mental illness.
| Variable | 95% CI | |
|---|---|---|
| Age (years) | 56.59±14.22 | 53.27–59.86 |
| Gender | ||
| Male | 22.9 (16) | 12.9–32.9 |
| Female | 77.1 (54) | 67.1–87.1 |
| Social security | ||
| Unaffiliated | 1.4 (1) | 0–4.3 |
| Subsidised | 61.4 (43) | 50–71.4 |
| Contributory | 25.7 (18) | 15.7–38.6 |
| Special regime | 11.4 (8) | 4.3–20 |
| Education (years) | 10.80±5.08 | 9.57–11.94 |
| Marital status | ||
| Single/never married | 28.6 (20) | 18.6–40 |
| Married/cohabiting | 47.1 (33) | 35.7–58.6 |
| Separated/divorced | 7.1 (5) | 1.4–14.2 |
| Widowed | 17.1 (12) | 8.6–25.7 |
| Occupational status | ||
| Employed | 14.3 (10) | 7.1–22.9 |
| Self-employed | 25.7 (18) | 15.7–35.7 |
| In unpaid work | 1.4 (1) | 0–4.3 |
| Student | 2.9 (2) | 0–7.1 |
| Responsible for looking after the home | 38.6 (27) | 28.6–50 |
| Retired | 15.7 (11) | 7.1–24.3 |
| Unemployed/other reasons | 1.4 (1) | 0–4.3 |
| Socioeconomic stratum | ||
| 1 | 14.3 (10) | 7.1–22.9 |
| 2 | 34.4 (24) | 22.9–45.7 |
| 3 | 37.1 (26) | 25.7–48.6 |
| 4 | 11.4 (8) | 4.3–18.6 |
| 5 | 1.4 (1) | 0–4.3 |
| 6 | 1.4 (1) | 0–4.3 |
| Relationship to the person with MI | ||
| Parent | 51.4 (36) | 40–62.9 |
| Spouse | 14.3 (10) | 7.1–22.9 |
| Sibling | 15.7 (11) | 7.1–24.3 |
| Child | 8.6 (6) | 2.9–15.7 |
| Other relative | 8.6 (6) | 2.9–15.7 |
| Friend/acquaintance | 1.4 (1) | 0–4.3 |
| Support from another person | ||
| No | 38.6 (27) | 27.1–50.0 |
| Yes | 61.4 (43) | 50.0–72.9 |
| Time spent as a carer (years) | 8.21±8.94 | 6.17–10.36 |
| Daily time spent on caring activities (h) | 12.87±9.37 | 10.57–15.38 |
| Age of the person with MI (years) | 43.3±18.54 | 38.92–47.67 |
| Gender of the person with MI | ||
| Male | 51.4 (36) | 40–62.9 |
| Female | 48.6 (34) | 37.1–60 |
| Social security | ||
| Subsidised | 70.0 (49) | 60.0–80 |
| Contributory | 24.3 (17) | 14.3–34.3 |
| Special regime | 5.7 (4) | 0–11.4 |
| Education (years) | 10.03±3.97 | 9.11–11.03 |
| Marital status | ||
| Single | 67.1 (47) | 55.7–77.1 |
| Married/cohabiting | 22.9 (16) | 12.9–34.2 |
| Separated/divorced | 2.9 (2) | 0–7.1 |
| Widowed | 7.1 (5) | 1.4–14.3 |
| Occupational status | ||
| Employed | 5.7 (4) | 1.4–11.4 |
| Self-employed | 8.6 (6) | 2.9–14.3 |
| In unpaid work | 1.4 (1) | 0–4.3 |
| Student | 10 (7) | 4.3–17.1 |
| Responsible for looking after the home | 10 (7) | 4.3–17.1 |
| Unemployed for health reasons | 7.1 (5) | 1.4–14.3 |
| Unemployed for other reasons | 54.3 (38) | 42.9–65.7 |
| Retired | 2.9 (2) | 0–7.1 |
| Time since diagnosis (years) | 9.23±11.03 | 6.77–11.84 |
| Degree of disability | ||
| None | 14.3 (10) | 7.1–22.9 |
| Mild | 52.9 (37) | 41.4–64.3 |
| Moderate–severe | 32.9 (23) | 22.9–42.9 |
MI: mental illness; 95% CI: 95% confidence interval.
Values are expressed as the % (n) or mean±standard deviation.
The carer sociodemographic profile is identified as predominantly female (71.4%), with an average age of 56.6 years, members of the subsidised healthcare regime (61.4%), with an average time in education of 10.8 years, married or cohabiting (47.1%) and responsible for looking after the home (38.6%). Out of the sample as a whole, 85.8% belong to low socioeconomic strata; primarily the relationship to the person with mental illness was that of mother (51.4%); 61.4% are supported by another person; they have been in the role for an average of 8.21 years and perform it for around 12 hours per day.
In terms of the characteristics of the individuals with mental illness, 51.4% are male, they are members of the subsidised healthcare regime (70%), single (67.1%); 61.4% are unemployed; on average they have been living with the diagnosis for 9.23 years and 85.2% present some degree of disability.
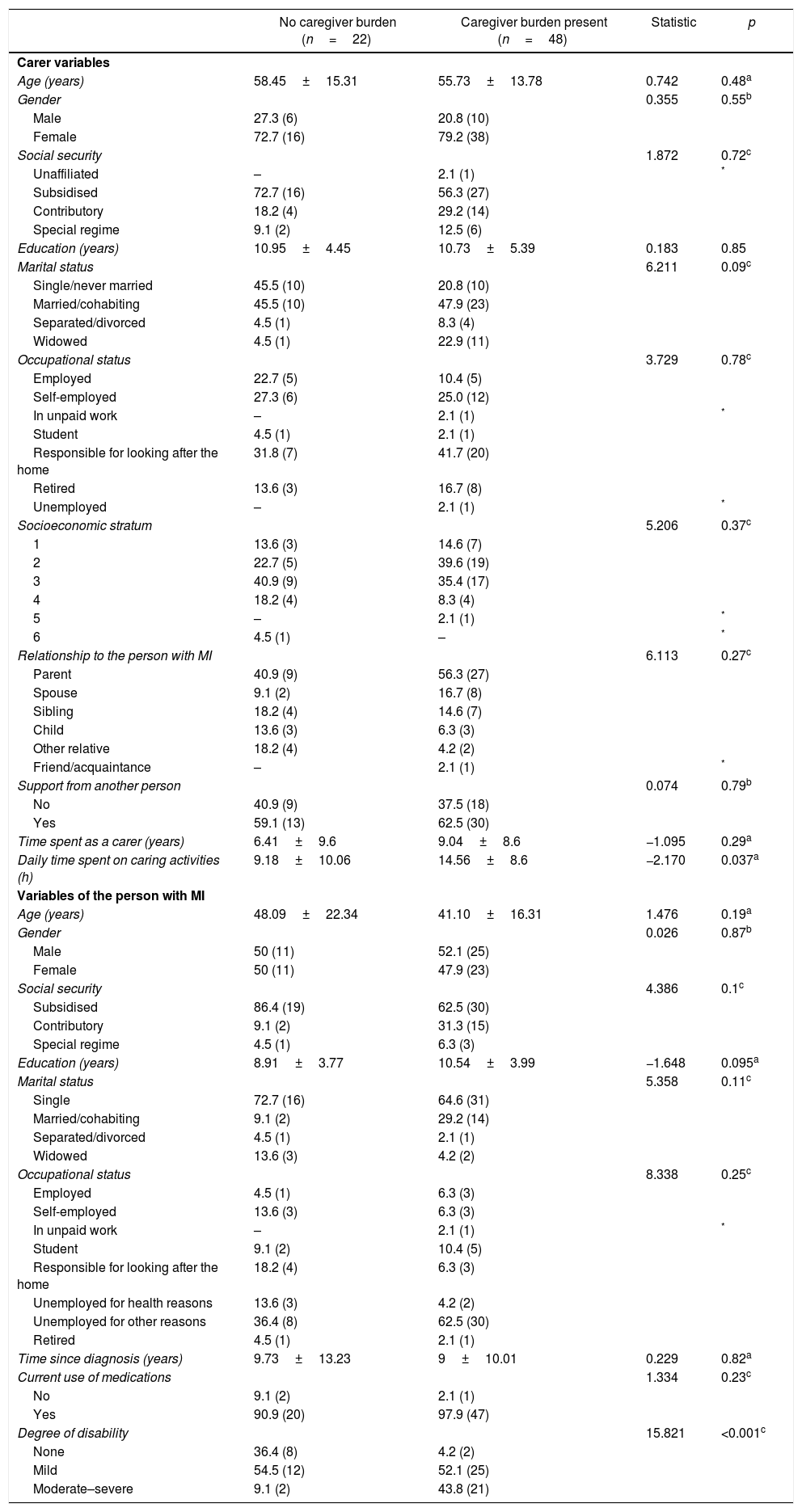
Variables associated with the incidence of caregiver burdenTo identify possible associations between the sociodemographic and clinical variables, a bivariate analysis was performed with caregiver burden as a dichotomous variable. The presence of the event was defined as any case with a direct score >22 on the Zarit scale (Table 3).
Bivariate analysis caregiver burden and sociodemographic and clinical variables.
| No caregiver burden (n=22) | Caregiver burden present (n=48) | Statistic | p | |
|---|---|---|---|---|
| Carer variables | ||||
| Age (years) | 58.45±15.31 | 55.73±13.78 | 0.742 | 0.48a |
| Gender | 0.355 | 0.55b | ||
| Male | 27.3 (6) | 20.8 (10) | ||
| Female | 72.7 (16) | 79.2 (38) | ||
| Social security | 1.872 | 0.72c | ||
| Unaffiliated | – | 2.1 (1) | * | |
| Subsidised | 72.7 (16) | 56.3 (27) | ||
| Contributory | 18.2 (4) | 29.2 (14) | ||
| Special regime | 9.1 (2) | 12.5 (6) | ||
| Education (years) | 10.95±4.45 | 10.73±5.39 | 0.183 | 0.85 |
| Marital status | 6.211 | 0.09c | ||
| Single/never married | 45.5 (10) | 20.8 (10) | ||
| Married/cohabiting | 45.5 (10) | 47.9 (23) | ||
| Separated/divorced | 4.5 (1) | 8.3 (4) | ||
| Widowed | 4.5 (1) | 22.9 (11) | ||
| Occupational status | 3.729 | 0.78c | ||
| Employed | 22.7 (5) | 10.4 (5) | ||
| Self-employed | 27.3 (6) | 25.0 (12) | ||
| In unpaid work | – | 2.1 (1) | * | |
| Student | 4.5 (1) | 2.1 (1) | ||
| Responsible for looking after the home | 31.8 (7) | 41.7 (20) | ||
| Retired | 13.6 (3) | 16.7 (8) | ||
| Unemployed | – | 2.1 (1) | * | |
| Socioeconomic stratum | 5.206 | 0.37c | ||
| 1 | 13.6 (3) | 14.6 (7) | ||
| 2 | 22.7 (5) | 39.6 (19) | ||
| 3 | 40.9 (9) | 35.4 (17) | ||
| 4 | 18.2 (4) | 8.3 (4) | ||
| 5 | – | 2.1 (1) | * | |
| 6 | 4.5 (1) | – | * | |
| Relationship to the person with MI | 6.113 | 0.27c | ||
| Parent | 40.9 (9) | 56.3 (27) | ||
| Spouse | 9.1 (2) | 16.7 (8) | ||
| Sibling | 18.2 (4) | 14.6 (7) | ||
| Child | 13.6 (3) | 6.3 (3) | ||
| Other relative | 18.2 (4) | 4.2 (2) | ||
| Friend/acquaintance | – | 2.1 (1) | * | |
| Support from another person | 0.074 | 0.79b | ||
| No | 40.9 (9) | 37.5 (18) | ||
| Yes | 59.1 (13) | 62.5 (30) | ||
| Time spent as a carer (years) | 6.41±9.6 | 9.04±8.6 | −1.095 | 0.29a |
| Daily time spent on caring activities (h) | 9.18±10.06 | 14.56±8.6 | −2.170 | 0.037a |
| Variables of the person with MI | ||||
| Age (years) | 48.09±22.34 | 41.10±16.31 | 1.476 | 0.19a |
| Gender | 0.026 | 0.87b | ||
| Male | 50 (11) | 52.1 (25) | ||
| Female | 50 (11) | 47.9 (23) | ||
| Social security | 4.386 | 0.1c | ||
| Subsidised | 86.4 (19) | 62.5 (30) | ||
| Contributory | 9.1 (2) | 31.3 (15) | ||
| Special regime | 4.5 (1) | 6.3 (3) | ||
| Education (years) | 8.91±3.77 | 10.54±3.99 | −1.648 | 0.095a |
| Marital status | 5.358 | 0.11c | ||
| Single | 72.7 (16) | 64.6 (31) | ||
| Married/cohabiting | 9.1 (2) | 29.2 (14) | ||
| Separated/divorced | 4.5 (1) | 2.1 (1) | ||
| Widowed | 13.6 (3) | 4.2 (2) | ||
| Occupational status | 8.338 | 0.25c | ||
| Employed | 4.5 (1) | 6.3 (3) | ||
| Self-employed | 13.6 (3) | 6.3 (3) | ||
| In unpaid work | – | 2.1 (1) | * | |
| Student | 9.1 (2) | 10.4 (5) | ||
| Responsible for looking after the home | 18.2 (4) | 6.3 (3) | ||
| Unemployed for health reasons | 13.6 (3) | 4.2 (2) | ||
| Unemployed for other reasons | 36.4 (8) | 62.5 (30) | ||
| Retired | 4.5 (1) | 2.1 (1) | ||
| Time since diagnosis (years) | 9.73±13.23 | 9±10.01 | 0.229 | 0.82a |
| Current use of medications | 1.334 | 0.23c | ||
| No | 9.1 (2) | 2.1 (1) | ||
| Yes | 90.9 (20) | 97.9 (47) | ||
| Degree of disability | 15.821 | <0.001c | ||
| None | 36.4 (8) | 4.2 (2) | ||
| Mild | 54.5 (12) | 52.1 (25) | ||
| Moderate–severe | 9.1 (2) | 43.8 (21) | ||
MI: mental illness; 95% CI: 95% confidence interval.
The results of this study suggest that there is an association with daily time (t=−2.170; p=0.037), a variable linked to the characteristics of the person being cared for. In terms of clinical variables, an association was found with the presence of any degree of disability in the person with mental illness (χ2=15.821; p<0.001). Other variables described by the literature were considered, but no association with the presence of an event was found in the reference population.
DiscussionThis study enables us to establish a carer profile of people with mental illness treated in the DHC programme of a tertiary institution in the city of Cali; in this profile, high caregiver burden can be identified among the people undertaking this role. Although 68% of the sample presented some degree of burden, it is noteworthy that those with a severe burden accounted for 57% of all participants. Some studies have obtained similar results, including in particular a higher incidence of this phenomenon among carers of people with neuropsychiatric symptoms.14,15 In this respect, Rodríguez-González et al.16 reported that alterations in mood and behaviour are predictors of overload.
In the literature, factors are recognised that allow the negative effects of the role and general characteristics of the carer to be recognised, and variables such as gender, age, support from other family members in assuming the role of carer, duration in the role and daily time spent on caring activities are clear to see.16–18 The results of this research are comparable to previous work identifying that the role falls primarily on women over 55 years of age who are responsible for looking after the home, usually the mothers of the person with mental illness. In the case of the carers of the DHC programme's beneficiaries, it was established that daily time spent in caring activities >13 hours and the presence of high levels of disability are the main factors indicating a high degree of overload. Environmental factors such as not receiving support from another person and occupational status can also influence this. The relevance of these results pertains to the fact that the carer is assumed to be close to the person with mental illness, in most cases a family member, and must therefore take on new commitments and perform some duties that were previously taken on by the person under their care.18–20 In this regard, a study conducted by Ocampo et al.21 in the older adult population of Buenaventura (Valle del Cauca) concludes that elements such as independence and autonomy influence the subjective burden manifested by the carer.
From a relationship perspective, the amount and quality of the care provided by the carer are determined by factors such as time, patient-carer relationship, the characteristics of the illness and training.16,17 In this sense, the carer as an element in the social environment can galvanise the participation of the person with mental illness in various everyday scenarios.17 The mood- and behaviour-related characteristics of a person with mental illness and some degree of dependence mean that specialised and individualised care is required. The carer plays an important role in the person's care, exerting a facilitatory effect on the satisfaction of basic needs, the creation of a safe environment and, primarily, ensuring recognition of the person's right to dignity.22,23
With regard to socioeconomic conditions, the participating population consists of beneficiaries of public sector services. It is therefore possible to identify people from low socioeconomic strata who are not in paid work and have a low level of education. The studies conducted by Pérez,17 Gutiérrez-Maldonado et al.24 and Carreño et al.25 found similar results, in which the relationship between these sociodemographic characteristics and situations of poverty and vulnerability are evident.
As a multifactorial phenomenon, caregiver overload involves social isolation, overload of activities both in and outside the home, altered behaviour of the family members receiving care, the idea of being solely “responsible” for the family member, financial difficulties and even the carer leaving employment.6,24–27 Based on the results of this research, interventions to respond to the needs of carers can be oriented in a way that prevents the infringement of rights and includes information on acquiring medications, social security, the structuring of the role and differentiation with the person to whom the care is given, social inclusion and training on the disease and their own health. In the case of mental illness, the carer is exposed to conditions including self-stigma and stigma by association, which could point to elements that predispose them to psychosocial morbidity.22,23,28,29
For occupational therapists, it is worth encouraging critical reflection on the need for carer-directed information and education, with the aim of avoiding their quality of life being negatively effected; the former is backed up by interventions that focus on reducing carer complaints, for which the discipline has not generated sufficient evidence in the Latin American context. For professionals in the discipline, initiatives must incorporate interdisciplinary approaches that foster developments to construct and maintain the autonomy of the person with mental illness, as well as providing the necessary elements to preserve the differentiation between occupational roles.30
Based on the results of this research, future studies are needed that include assessment of the impact of evidence-based interventions. Moreover, the construction of a baseline will allow the groundwork to be laid for the development of routes of action that will enhance research processes with respect to environmental factors, including studying themes relating to caregiver overload syndrome.
As limitations of the study—given the programme's administrative conditions, which define the care quota based on the installed capacity—we must highlight the convenience sampling, which means that the results must be interpreted with caution, calling their external validity into question, due primarily to the conditions of the population consulted. In future research seeking to determine causal relationships, studies will be needed with analytical methodologies that include control groups or processes of an experimental nature.
Ethical responsibilitiesProtection of people and animalsThe authors state that the procedures followed conformed to the ethical standards of the responsible committee on human experimentation and to the World Medical Association and the Declaration of Helsinki.
Data confidentialityThe authors declare that they have followed the protocols implemented in their place of work regarding the publication of patient data.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
Conflicts of interestThe authors declare that they have no conflicts of interest. The research was conducted in the context of the 2015 internal call for submissions by the Vice-Rector of Research of the University del Valle, backed by the Synergy research group of the School of Human Rehabilitation, of which the authors are members.
The research group would like to thank Hospital Psiquiátrico Universitario del Valle in Cali for allowing the research to be conducted on its premises. Thanks also go to the families and to the Occupational Therapy students of the Universidad del Valle for their valuable contributions in sharing their experiences and fully committing to the research.
Please cite this article as: Salazar-Torres LJ, Castro-Alzate ES, Dávila-Vásquez PX. Carga del cuidador en familias de personas con enfermedad mental vinculadas al programa de hospital de día de una institución de tercer nivel en Cali (Colombia). Rev Colomb Psiquiat. 2019;48:88–95.