Literature reports show that bipolar offspring (BO) present with a wide range of psychiatric disorders. Comparison between BO and control parent offspring (CPO) may help to identify which psychopathological findings are specific to this high-risk group.
ObjectiveTo compare the psychopathological characteristics between a group of BO type-I and a group of CPO, by identifying the presence of psychiatric disorders according the DSM-IV-TR.
MethodsA descriptive-correlational, cross-sectional and comparative study was conducted with 127 offspring of parents with bipolar disorder type-I from the multimodal intervention programme (PRISMA) and with 150 CPO between 6 and 30 years of age. Subjects were evaluated with validated diagnostic interviews (K-SADS-PL and DIGS).
ResultsThe BO group showed higher frequencies for bipolar disorder (prevalence ratio [PR]=17.70; 95% confidence interval [CI]; 1.02–306.83), bipolar disorder not otherwise specified (PR=23.07, 95% CI; 2.8–189.0, p=0.0001), disorders due to psychoactive substance use (PR=9.52, 95% CI; 2.93–30.90), oppositional defiant disorder (PR=4.10, 95% CI; 1.70–9.89), posttraumatic stress disorder (PR=3.90, 95% CI 1.30–11.66), disorder due to alcohol use (PR=3.84, 95% CI; 1.28–11.48), attention deficit/hyperactivity disorder (PR=2.26, 95% CI; 1.37–3.75), and major depressive disorder (PR=2.25, 95% CI; 1.13–4.50). Statistically significant differences were also found in the CGAS and GAF functional scales, with lower scores for the BO group.
ConclusionThese findings confirm previous literature reports showing that BO have higher rates of affective and non-affective psychiatric disorders than control subjects, and also a lower level of global functioning.
Reportes en la literatura muestran que los Hijos de Padres con Trastorno Bipolar tipo I (HPTB) manifiestan un amplio rango de trastornos psiquiátricos. La comparación entre los HPTB y los Hijos de Padres Control (HPC) permite establecer cuáles hallazgos psicopatológicos son específicos de este grupo de alto riesgo.
ObjetivoComparar las características psicopatológicas entre un grupo de HPTB tipo I y un grupo de HPC, mediante la identificación de la presencia de trastornos psiquiátricos según el DSM-IV-TR.
MetodologíaSe realizó un estudio descriptivo-correlacional, comparativo de corte transversal con 127 Hijos de Padres con TAB tipo I (HPTB-I) dentro de un programa de intervención multimodal (PRISMA) y 150 HPC, con edades entre los seis y 30 años. Los sujetos fueron evaluados con entrevistas diagnósticas validados (K-SADS-PL y DIGS).
ResultadosEl grupo de HPTB mostró mayor frecuencias de trastorno bipolar (Razón de Prevalencia [RP]=17,70; Intervalo de Confianza [IC] del 95%, 1,02-306,83), trastorno bipolar no especificado (RP=23,07, IC 95% 2,8 -189, p=0.0001), trastorno por uso de sustancias psicoactivas (RP=9,52; IC 95%, 2,93-30,90), trastorno oposicionista desafiante (RP=4,10; IC 95%, 1,70-9,89); trastorno de estrés postraumático (RP=3,90; IC 95%, 1,30-11,66), trastorno por uso de alcohol (RP=3,84; IC 95%, 1,2811,48), trastorno por déficit de atención e hiperactividad (RP=2,26; IC 95%, 1,37-3,75) y trastorno depresivo mayor (RP=2,25; IC 95%, 1,13-4,50). Tambien se encontraron diferencias estadisticamente significativas en las escalas de funcionalidad CGAS y GAF, con menor puntaje en el grupo de HPB.
ConclusiónEstos hallazgos confirman reportes previos de la literatura que demuestran que los HPTB presentan mayores tasas de trastornos psiquiatricos afectivos y no afectivos, y una menor nivel de funcionalidad global, al ser comparados con sujetos controles de la comunidad.
Bipolar affective disorder (BAD) is a recurrent entity that affects aspects of the individual's behaviour and functioning.1 It has a prevalence of 1.3% in the general population2 and 1.8% in the Colombian population.3 Several authors have demonstrated its high heritability,4–9 thus indicating that studying the population of children of parents with bipolar disorder (CPBD) could be an opportunity to learn about the natural history and prodrome symptoms of this condition. Moreover, it would allow for the adoption of early management strategies and the achievement of better long-term psychosocial outcomes.
Descriptions in the literature show that CPBD have a higher risk of suffering mental disorders than children of control parents (CCP).10,11 In the CPBD group of their meta-analysis, Lapalme et al. found a 2.7-fold increase in the risk of a psychiatric disorder and a 4-fold increase in the risk of an affective disorder.12 Meanwhile, Birmaher et al. found that CPBD have a 13.4-fold increase in the risk of having a bipolar spectrum disorder (BAD I–II/NOS) compared to CCP.13 Likewise, higher prevalences of non-affective psychopathology, subthreshold psychiatric symptoms and reduced functionality have been reported in this population; anxiety disorders, disruptive disorders and substance use disorders are the most frequently encountered conditions. However, there is still no consensus on which is the most prevalent.13–25 Although there are few reports outside the United States and Europe, studies in Latin America have shown some similar results.11,26
Preliminary results from a local study on children of parents with BAD-I (CPBD-I), within a multimodal intervention programme (PRISMA) conducted by our research group, show that the most prevalent diagnoses are attention deficit hyperactivity disorder (ADHD), major depressive disorder (MDD), and separation anxiety disorder (SAD).27,28 However, it is not possible to establish if these frequencies are characteristic of CPBD or whether they would be the same as those of a control group from the community. To address this question, a comparison group from the same geographical area is required. Furthermore, according to the authors’ knowledge, there are no comparative studies with these characteristics and a significant number of participants to date in Colombia.
The objective of this study is to compare the psychopathological characteristics of a group of CPBD and a group of CCP using validated diagnostic instruments. It also seeks to determine the psychopathological differences of psychiatric disorders.
MethodsDescriptive, comparative and cross-sectional study. Patients diagnosed with BAD-I enrolled in a multimodal intervention programme (PRISMA) were invited to participate, and their partners (known as “biological co-parents”) and all children aged 6–30 years were also invited to take part. These families were received by the Affective Disorders Group of the Hospital Universitario San Vicente Fundación from June 2009 to February 2014 as well as by the PRISMA programme. Some preliminary results of this study have already been published.27,29,30
Study populationThose who were included formed the CPBD and CCP populations if they met the following eligibility criteria: aged 6–30 years with no health problems preventing them from participating in a clinical interview, moderate or severe mental retardation, or classic autism according to criteria of the Fourth Edition of the Diagnostic and Statistical Manual of Mental Disorders-Revised Text (DSM-IV-RT).31
To calculate the sample size, a prevalence of general psychiatric disorders among CPBD of 16%,32 a power of 80% and a type I error of 5% were taken as a reference. As a result, the sample size for this study would be 90 CPBD and 90 CCP (with Yates correction, 100 CPBD and 101 CCP). After calculating a margin of loss of 20%, the final sample should be composed of 126 CPBD and 128 CCP.
ProceduresThe research protocol was approved by the Ethics Committee of the Centre for Medical Research of the Universidad de Antioquia's Faculty of Medicine, and by the Ethics Committee of the Hospital Universitario de San Vicente Fundación for the subjects’ evaluation.
200 BAD-I patients who were already known to the Psychiatric Research Group (GIPSI) of the Universidad de Antioquia and managed by the Affective Disorders Group of the Hospital Universitario de San Vicente Fundación were invited to participate, along with their partners (defined by the researchers as “biological co-parents”) and their children. The parents’ inclusion criteria were: having a diagnostic interview for genetic studies (DIGS)33 that confirmed the BAD-I diagnosis according to the DSM-IV-TR31 criteria, belonging to families from Antioquia for more than two generations, having had at least one psychiatric hospitalisation before the age of 50 (with a clinical record to document it), being over 18 years of age and having no mental disorder of organic origin.
In addition, a control group of parents from the same geographical area was invited to participate, along with their partners and their children. None of the control parents could have been diagnosed with BAD or psychotic disorders according to the DIGS interview,33 but the inclusion of parents with other disorders such as MDD or anxiety disorders was permitted. Parents and co-parents from this group should not have any first-degree relatives with a history of BAD. In order to match the parental control group, the mean age, gender and urban or rural origin were taken into account (those from the urban area were received in Medellín and the metropolitan area, while those from the urban area, in the municipalities of origin of the parents with BD: Marinilla, Guarne, Santuario, Carmen del Viboral, La Ceja and El Retiro, mostly).
The eligible children of both groups were included, with their parents’ prior approval to participate in the study (for children under 18 years of age). Each of the subjects and parents who agreed to participate were clearly and truthfully informed of the study's purpose and objective, as well as the meaning of their participation, which was corroborated by signing an informed consent form. Thus, each parent signed their own consent form and as well as an additional consent form for each child under 18 years of age who was due to participate in the study (who also had to agree to participate).
The ages of 6 and 30 years were taken as limits for the children of both groups, considering that subjects below 6 years of age could have limitations in their communicative capacities and also because the diagnostic interview that was used for children under 18 years only evaluated subjects of that age and above. The children's upper limit of 30 years was arbitrarily defined, considering that late-onset psychiatric disorders can be identified between the ages of 18 and 30 years. The screening of the sample of children was initially carried out among the CPBD, followed by the CCP, until a sufficient number of comparable children was found according to the variables of gender, age group and origin. All the children of families who wanted to participate in the study were included as long as they fulfilled the criteria.
InstrumentsParentsThe parents of both groups and the biological co-parents who participated in the study underwent the DIGS33 in order to determine their status of being clinically affected or unaffected by BAD and other psychiatric disorders.
ChildrenCPBD under the age of 18 were subjected to the Schedule for Affective Disorders and Schizophrenia for School Aged Children Lifetime version (K-SADS-PL),34,35 with the aim of establishing the presence of psychiatric diagnoses according to the DSM-IV-RT criteria. Moreover, the Children's Global Assessment Scale (CGAS)36 was applied to measure functionality at the present time, during the latest episode of any psychiatric disorder, and at the best time of life (scored from 0 to 100 points). CPBD under 18 years of age underwent the DIGS and an additional document was also applied with sections of anxiety disorders and disruptive disorders from the K-SADS-LP. Meanwhile, adult children were subjected to the global assessment of functioning (GAF) scale to measure functionality at the present time and during the past month (scored from 0 to 100 points).
The interviews were conducted by a psychiatry resident or a psychiatrist who had received previous training on the use of the DIGS and K-SADS-LP. The children's diagnoses were masked for the evaluators. Finally, two expert psychiatrists, different from those who performed the diagnostic interviews, performed a best diagnostic estimate procedure in order to corroborate the psychiatric diagnosis. If they did not agree, the input of a third evaluator was added.
Demographic and clinical variablesThe following were used as demographic variables: gender, age, education, number of years repeated, occupation, place of residence (rural or urban) and socio-economic status. The clinical variables considered were the presence of the following psychiatric diagnoses according to the DSM-IV-RT31: ADHD, oppositional defiant disorder (ODD), antisocial personality disorder (APD), BAD, MDD, psychotic disorders, panic disorders, SAD, avoidant disorder/social phobia, agoraphobia and specific phobias, generalised anxiety disorder (GAD) obsessive-compulsive disorder (OCD), enuresis, encopresis, anorexia nervosa, bulimia nervosa, tic disorders, post-traumatic stress disorder (PTSD) and substance use disorder (SUD): tobacco, alcohol, and/or psychoactive substances (PAS).
Age groups of childrenTo describe the differences in psychiatric disorders between CPBD and CCP, three age groups were considered. The schoolchildren group comprised subjects aged 6–11 years; the adolescent group, those aged 12–17 years; and the adult group, those aged 18–30 years. In order to match the CPBD group, age, gender and urban or rural origin variables were taken into account so that, once the CPBD sample was attained, it was paired up so that the CCP group had a comparable number of subjects in each age group, gender and area of origin.
Statistical analysisTo describe the subjects participating in the study, absolute and relative frequency (percentage) measures were used to calculate the proportion of children (schoolchildren, adolescents and adults) with general and specific psychopathological characteristics (qualitative variables). To compare and determine the differences in the psychopathological characteristics between the groups of children and by age group, the χ2 test of independence and the Fisher's exact test were used, and the prevalence ratio (PR) was calculated with its respective 95% confidence interval (95% CI). When empty boxes were found in the comparisons between CPBD and CCP due to the absence of individuals with a certain characteristic, a Yates's correction was performed. Mann–Whitney (for quantitative variables of non-normal distribution) and t-tests (for quantitative variables of normal distribution) were also used for the analysis. A level of significance of p<0.05 was used. Data analysis was performed using the IBM SPSS Statistics software, version 19.
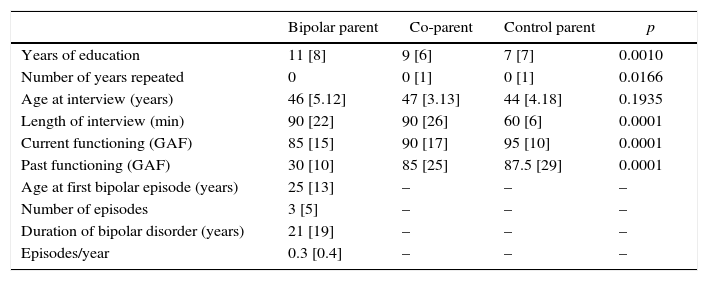
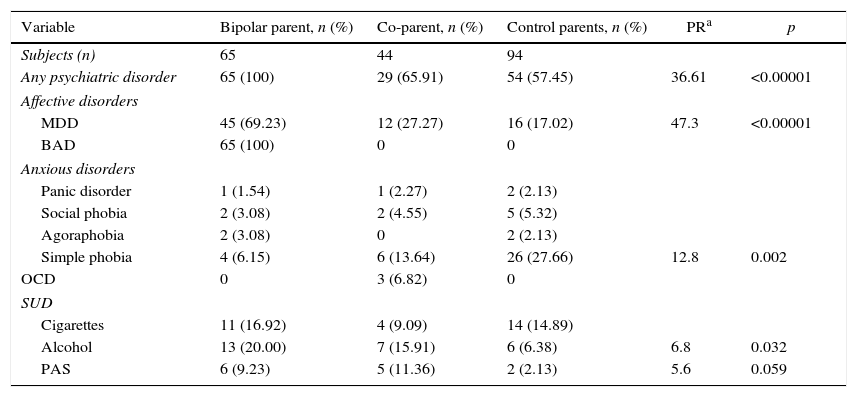
ResultsThe characteristics of the parents with BAD, the co-parents and the control parents are collected in Table 1. 66% of the parents with BAD and 60% of the control parents were women. The mean age at the first BAD episode was 25.1±8.68 years. 58.5% began with a manic episode; 32.3% with a depressive episode and 9.2% with a mixed episode. The average number of bipolar episodes that parents with BAD have suffered throughout life was 5.92±6.4, and the average duration of the disease was 20.5±11.8 years. The number of participant children in the groups of parents with BAD and control parents was 1.92±1.3 and 2.49±0.9, respectively. Table 2 shows a comparison of the psychiatric disorders of the three groups of parents. 57% of parents in the control group suffer from some form of psychiatric disorder.
Demographic characteristics and functionality of parents with bipolar disorder, biological co-parents and control parents.
| Bipolar parent | Co-parent | Control parent | p | |
|---|---|---|---|---|
| Years of education | 11 [8] | 9 [6] | 7 [7] | 0.0010 |
| Number of years repeated | 0 | 0 [1] | 0 [1] | 0.0166 |
| Age at interview (years) | 46 [5.12] | 47 [3.13] | 44 [4.18] | 0.1935 |
| Length of interview (min) | 90 [22] | 90 [26] | 60 [6] | 0.0001 |
| Current functioning (GAF) | 85 [15] | 90 [17] | 95 [10] | 0.0001 |
| Past functioning (GAF) | 30 [10] | 85 [25] | 87.5 [29] | 0.0001 |
| Age at first bipolar episode (years) | 25 [13] | – | – | – |
| Number of episodes | 3 [5] | – | – | – |
| Duration of bipolar disorder (years) | 21 [19] | – | – | – |
| Episodes/year | 0.3 [0.4] | – | – | – |
The values express the median [interquartile range].
Comparison of psychiatric disorders between parents with bipolar disorder, biological co-parents and control parents.
| Variable | Bipolar parent, n (%) | Co-parent, n (%) | Control parents, n (%) | PRa | p |
|---|---|---|---|---|---|
| Subjects (n) | 65 | 44 | 94 | ||
| Any psychiatric disorder | 65 (100) | 29 (65.91) | 54 (57.45) | 36.61 | <0.00001 |
| Affective disorders | |||||
| MDD | 45 (69.23) | 12 (27.27) | 16 (17.02) | 47.3 | <0.00001 |
| BAD | 65 (100) | 0 | 0 | ||
| Anxious disorders | |||||
| Panic disorder | 1 (1.54) | 1 (2.27) | 2 (2.13) | ||
| Social phobia | 2 (3.08) | 2 (4.55) | 5 (5.32) | ||
| Agoraphobia | 2 (3.08) | 0 | 2 (2.13) | ||
| Simple phobia | 4 (6.15) | 6 (13.64) | 26 (27.66) | 12.8 | 0.002 |
| OCD | 0 | 3 (6.82) | 0 | ||
| SUD | |||||
| Cigarettes | 11 (16.92) | 4 (9.09) | 14 (14.89) | ||
| Alcohol | 13 (20.00) | 7 (15.91) | 6 (6.38) | 6.8 | 0.032 |
| PAS | 6 (9.23) | 5 (11.36) | 2 (2.13) | 5.6 | 0.059 |
PR: prevalence ratio; PAS: psychoactive substances; BAD: bipolar affective disorder; MDD: major depressive disorder; PTSD: post-traumatic stress disorder; OCD: obsessive-compulsive disorder; SUD: substance use disorder.
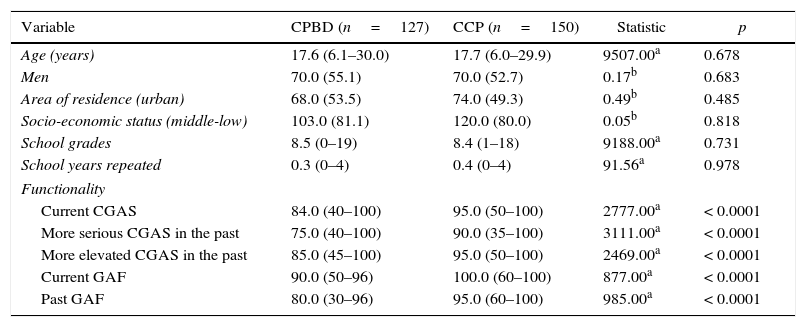
127 CPBD and 150 CCP were evaluated. The schoolchildren group had 63 participants (CPBD, 24; CCP, 39); the adolescent group, 86 (CPBD, 44, HPC, 42) and the adult children group, 128 (CPBD, 59; CCP, 69). 19 CPBD and 28 CCP were excluded from the study (16 were older than 30 years, 8 were younger than 6 years, 1 patient had Down's syndrome, 1 patient was diagnosed with autism, 1 subject was not a biological child, 15 were not available for evaluation and 5 did not agree to participate).
On comparing the demographic variables of both groups, no statistically significant differences were found. The majority of the subjects evaluated in the two groups belonged to middle-low socio-economic strata. CPBD had lower functionality scores on current and past measurements, with statistically significant differences (Table 3).
Demographic characteristics and functionality of children of parents with bipolar disorder and children of control parents.
| Variable | CPBD (n=127) | CCP (n=150) | Statistic | p |
|---|---|---|---|---|
| Age (years) | 17.6 (6.1–30.0) | 17.7 (6.0–29.9) | 9507.00a | 0.678 |
| Men | 70.0 (55.1) | 70.0 (52.7) | 0.17b | 0.683 |
| Area of residence (urban) | 68.0 (53.5) | 74.0 (49.3) | 0.49b | 0.485 |
| Socio-economic status (middle-low) | 103.0 (81.1) | 120.0 (80.0) | 0.05b | 0.818 |
| School grades | 8.5 (0–19) | 8.4 (1–18) | 9188.00a | 0.731 |
| School years repeated | 0.3 (0–4) | 0.4 (0–4) | 91.56a | 0.978 |
| Functionality | ||||
| Current CGAS | 84.0 (40–100) | 95.0 (50–100) | 2777.00a | < 0.0001 |
| More serious CGAS in the past | 75.0 (40–100) | 90.0 (35–100) | 3111.00a | < 0.0001 |
| More elevated CGAS in the past | 85.0 (45–100) | 95.0 (50–100) | 2469.00a | < 0.0001 |
| Current GAF | 90.0 (50–96) | 100.0 (60–100) | 877.00a | < 0.0001 |
| Past GAF | 80.0 (30–96) | 95.0 (60–100) | 985.00a | < 0.0001 |
CGAS: children's global assessment scale (part of the K-SADS-PL, applied to subjects aged 6–18 years); GAF: global assessment of functioning (part of DIGS, applied to subjects aged 18–30 years); CCP: children of control parents; CPBD: children of parents with bipolar disorder.
The values express the n (%) or median (range).
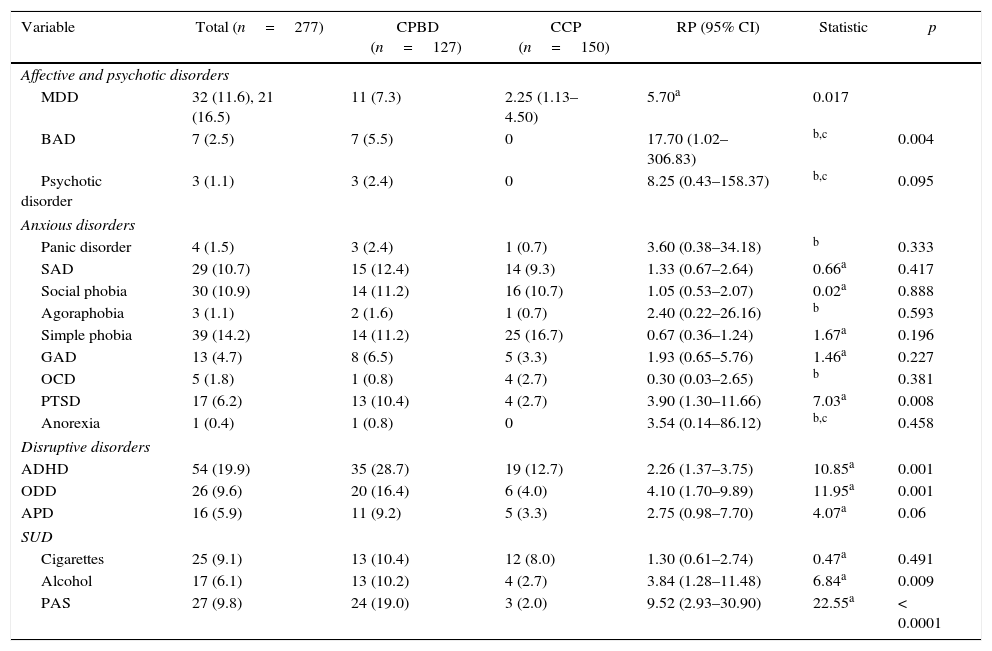
CPBD showed higher rates of psychiatric disorders. Among the affective disorders, BAD (PR=17.70; 95% CI, 1.02–306.83) and MDD (PR=2.25; 95% CI, 1.13–4.50) were found to have the greatest frequency. In anxious disorders a higher frequency of PTSD was found (PR=3.90; 95% CI, 1.30–11.66). In the disruptive disorders, there was a higher frequency of ODD (PR=4.10; 95% CI, 1.70–9.89) and ADHD (PR=2.26; 95% CI, 1.37–3.75). With regard to SUDs, there was a higher frequency due to alcohol (PR=3.84; 95% CI, 1.28–11.48) and PAS (PR=9.52; 95% CI, 2.93–30.90).
Of the total sample, 7 CPBD were found to have BAD, 4 of whom were women. The age at which BAD presented ranged from 10 to 21 years, with a mean of 17 years. The mean duration of the disease was 2.1 (range, 1–4) years; the average number of affective episodes was 1.86 (1–3), with an annual mean of 1.13 (0.2–2.15) affective episodes. The polarity of the first episode was depressive in 42.8%, manic in 42.8% and mixed in 14.2%. All children affected by BAD had psychotic symptoms associated with depressive or manic symptoms, which were mostly marked by auditory hallucinations. They also presented comorbidity with anxiety disorders; 5 of them with SAD and 3 with panic disorder; 1 subject presented comorbidity with OCD, GAD and social phobia. As for the externalising disorders, 2 affected children presented ADHD; 1 ODD and 1 APD.
On the other hand, it was found in the CPBD group that 17 subjects (13.4%) had a diagnosis of BAD NOS compared to 1 (0.7%) of the CCP group, with a significant difference (PR=23.07; 95% CI, 2.8–189; p<0.001).
Moreover, in male CPBD there was a higher risk of ADHD (PR=3.76, 95% CI, 1.84–7.70, p=0.001), any externalising disorder (PR=3.32, 95% CI, 1.74–6.34, p=0.001) and any SUD—cigarettes, alcohol and/or PAS (PR=2.31, 95% CI, 1.16–4.59, p<0.001). Also, in the CPBD there was a higher risk of suffering an externalising disorder plus a comorbid internalising disorder (PR=2.85; 95% CI, 1.31–6.18; p=0.001).
Although no significant differences were found between groups, there was a trend towards a higher risk of APD among CPBD (9.2 vs 3.3%; PR=2.75; 95% CI, 0.98–7.70; p=0.06). Although a greater number of subjects who had smoked on at least one occasion (33.6 vs 22.0%, p=0.032) were found in the CPBD group, there were no differences between groups when evaluating the presence of SUD due to cigarettes. There were also no differences on evaluating prior exposure to alcohol at any time in life (63.8 vs 54.7%, p=0.125) and having consumed a PAS at any point (23.6 vs 16.0%, p=0.11). A significant difference was found in SUDs due to PAS in CPBD (Table 4).
Comparison of psychiatric disorders according to the DSM-IV-RT among children of parents with bipolar disorder and children of control parents.
| Variable | Total (n=277) | CPBD (n=127) | CCP (n=150) | RP (95% CI) | Statistic | p |
|---|---|---|---|---|---|---|
| Affective and psychotic disorders | ||||||
| MDD | 32 (11.6), 21 (16.5) | 11 (7.3) | 2.25 (1.13–4.50) | 5.70a | 0.017 | |
| BAD | 7 (2.5) | 7 (5.5) | 0 | 17.70 (1.02–306.83) | b,c | 0.004 |
| Psychotic disorder | 3 (1.1) | 3 (2.4) | 0 | 8.25 (0.43–158.37) | b,c | 0.095 |
| Anxious disorders | ||||||
| Panic disorder | 4 (1.5) | 3 (2.4) | 1 (0.7) | 3.60 (0.38–34.18) | b | 0.333 |
| SAD | 29 (10.7) | 15 (12.4) | 14 (9.3) | 1.33 (0.67–2.64) | 0.66a | 0.417 |
| Social phobia | 30 (10.9) | 14 (11.2) | 16 (10.7) | 1.05 (0.53–2.07) | 0.02a | 0.888 |
| Agoraphobia | 3 (1.1) | 2 (1.6) | 1 (0.7) | 2.40 (0.22–26.16) | b | 0.593 |
| Simple phobia | 39 (14.2) | 14 (11.2) | 25 (16.7) | 0.67 (0.36–1.24) | 1.67a | 0.196 |
| GAD | 13 (4.7) | 8 (6.5) | 5 (3.3) | 1.93 (0.65–5.76) | 1.46a | 0.227 |
| OCD | 5 (1.8) | 1 (0.8) | 4 (2.7) | 0.30 (0.03–2.65) | b | 0.381 |
| PTSD | 17 (6.2) | 13 (10.4) | 4 (2.7) | 3.90 (1.30–11.66) | 7.03a | 0.008 |
| Anorexia | 1 (0.4) | 1 (0.8) | 0 | 3.54 (0.14–86.12) | b,c | 0.458 |
| Disruptive disorders | ||||||
| ADHD | 54 (19.9) | 35 (28.7) | 19 (12.7) | 2.26 (1.37–3.75) | 10.85a | 0.001 |
| ODD | 26 (9.6) | 20 (16.4) | 6 (4.0) | 4.10 (1.70–9.89) | 11.95a | 0.001 |
| APD | 16 (5.9) | 11 (9.2) | 5 (3.3) | 2.75 (0.98–7.70) | 4.07a | 0.06 |
| SUD | ||||||
| Cigarettes | 25 (9.1) | 13 (10.4) | 12 (8.0) | 1.30 (0.61–2.74) | 0.47a | 0.491 |
| Alcohol | 17 (6.1) | 13 (10.2) | 4 (2.7) | 3.84 (1.28–11.48) | 6.84a | 0.009 |
| PAS | 27 (9.8) | 24 (19.0) | 3 (2.0) | 9.52 (2.93–30.90) | 22.55a | < 0.0001 |
CCP: children of control parents; CPBD: children of parents with bipolar disorder; PR: prevalence ratio; PAS: psychoactive substances; BAD: bipolar affective disorder; GAD: generalised anxiety disorder; SAD: separation anxiety disorder; ADHD: attention deficit hyperactivity disorder; APD: antisocial personality disorder; MDD: major depressive disorder; PTSD: post-traumatic stress disorder; OCD: obsessive-compulsive disorder; ODD: oppositional defiant disorder; SUD: substance use disorder.
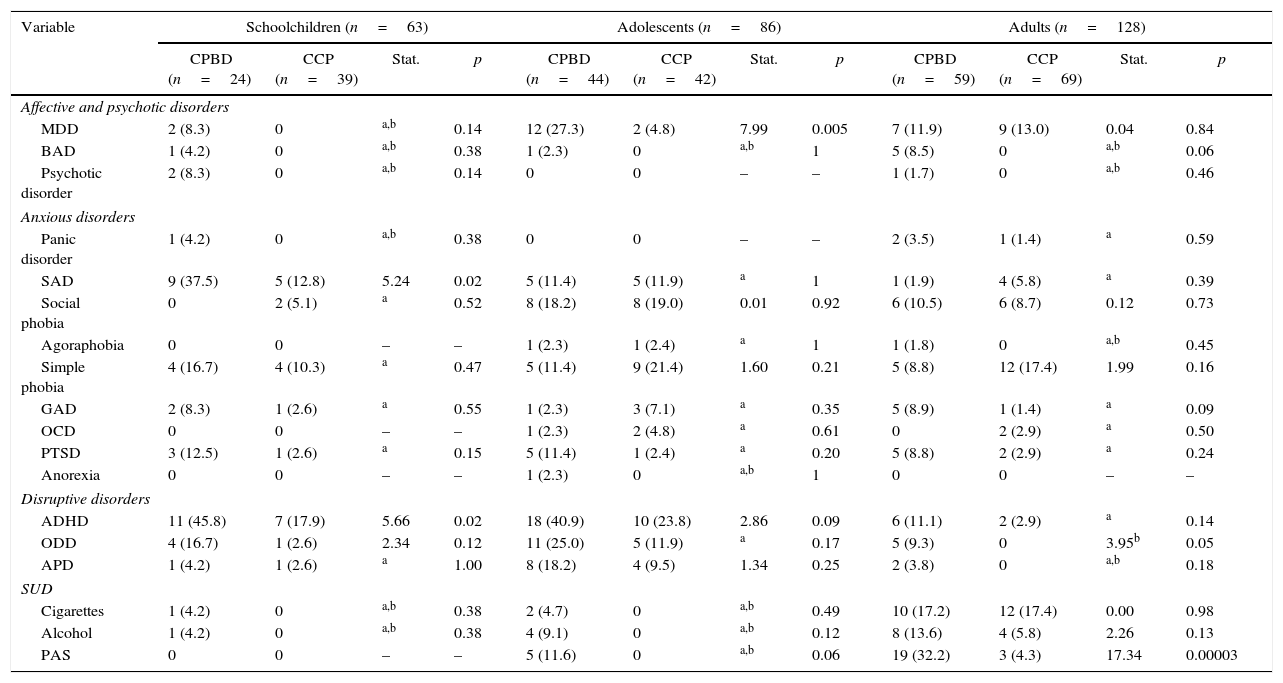
In the exploratory analysis by age group, the CPBD schoolchildren group had higher frequencies of SAD (PR=2.93, 95% CI, 1.11–7.70) and ADHD (PR=2.55, 95% CI, 1.15–5.69); the adolescent group had higher frequencies of MDD (PR=5.73, 95% CI, 1.36–24.08) and the CPBD adult group, of SUD due to PAS (PR=7.41, 95% CI, 2.31–23.80). Table 5 details the findings and their statistical value. It should be noted that the sample size of each subgroup (schoolchildren, adolescents, and adults) was not calculated.
Comparison of psychiatric disorders according to the DSM-IV-RT among children of parents with bipolar disorder and children of control parents by age group.
| Variable | Schoolchildren (n=63) | Adolescents (n=86) | Adults (n=128) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CPBD (n=24) | CCP (n=39) | Stat. | p | CPBD (n=44) | CCP (n=42) | Stat. | p | CPBD (n=59) | CCP (n=69) | Stat. | p | |
| Affective and psychotic disorders | ||||||||||||
| MDD | 2 (8.3) | 0 | a,b | 0.14 | 12 (27.3) | 2 (4.8) | 7.99 | 0.005 | 7 (11.9) | 9 (13.0) | 0.04 | 0.84 |
| BAD | 1 (4.2) | 0 | a,b | 0.38 | 1 (2.3) | 0 | a,b | 1 | 5 (8.5) | 0 | a,b | 0.06 |
| Psychotic disorder | 2 (8.3) | 0 | a,b | 0.14 | 0 | 0 | – | – | 1 (1.7) | 0 | a,b | 0.46 |
| Anxious disorders | ||||||||||||
| Panic disorder | 1 (4.2) | 0 | a,b | 0.38 | 0 | 0 | – | – | 2 (3.5) | 1 (1.4) | a | 0.59 |
| SAD | 9 (37.5) | 5 (12.8) | 5.24 | 0.02 | 5 (11.4) | 5 (11.9) | a | 1 | 1 (1.9) | 4 (5.8) | a | 0.39 |
| Social phobia | 0 | 2 (5.1) | a | 0.52 | 8 (18.2) | 8 (19.0) | 0.01 | 0.92 | 6 (10.5) | 6 (8.7) | 0.12 | 0.73 |
| Agoraphobia | 0 | 0 | – | – | 1 (2.3) | 1 (2.4) | a | 1 | 1 (1.8) | 0 | a,b | 0.45 |
| Simple phobia | 4 (16.7) | 4 (10.3) | a | 0.47 | 5 (11.4) | 9 (21.4) | 1.60 | 0.21 | 5 (8.8) | 12 (17.4) | 1.99 | 0.16 |
| GAD | 2 (8.3) | 1 (2.6) | a | 0.55 | 1 (2.3) | 3 (7.1) | a | 0.35 | 5 (8.9) | 1 (1.4) | a | 0.09 |
| OCD | 0 | 0 | – | – | 1 (2.3) | 2 (4.8) | a | 0.61 | 0 | 2 (2.9) | a | 0.50 |
| PTSD | 3 (12.5) | 1 (2.6) | a | 0.15 | 5 (11.4) | 1 (2.4) | a | 0.20 | 5 (8.8) | 2 (2.9) | a | 0.24 |
| Anorexia | 0 | 0 | – | – | 1 (2.3) | 0 | a,b | 1 | 0 | 0 | – | – |
| Disruptive disorders | ||||||||||||
| ADHD | 11 (45.8) | 7 (17.9) | 5.66 | 0.02 | 18 (40.9) | 10 (23.8) | 2.86 | 0.09 | 6 (11.1) | 2 (2.9) | a | 0.14 |
| ODD | 4 (16.7) | 1 (2.6) | 2.34 | 0.12 | 11 (25.0) | 5 (11.9) | a | 0.17 | 5 (9.3) | 0 | 3.95b | 0.05 |
| APD | 1 (4.2) | 1 (2.6) | a | 1.00 | 8 (18.2) | 4 (9.5) | 1.34 | 0.25 | 2 (3.8) | 0 | a,b | 0.18 |
| SUD | ||||||||||||
| Cigarettes | 1 (4.2) | 0 | a,b | 0.38 | 2 (4.7) | 0 | a,b | 0.49 | 10 (17.2) | 12 (17.4) | 0.00 | 0.98 |
| Alcohol | 1 (4.2) | 0 | a,b | 0.38 | 4 (9.1) | 0 | a,b | 0.12 | 8 (13.6) | 4 (5.8) | 2.26 | 0.13 |
| PAS | 0 | 0 | – | – | 5 (11.6) | 0 | a,b | 0.06 | 19 (32.2) | 3 (4.3) | 17.34 | 0.00003 |
Stat.: statistic; CCP: children of control parents; CPBD: children of parents with bipolar disorder; PAS: psychoactive substances; BAD: bipolar affective disorder; GAD: generalised anxiety disorder; SAD: separation anxiety disorder; ADHD: attention deficit hyperactivity disorder; APD: antisocial personality disorder; MDD: major depressive disorder; PTSD: post-traumatic stress disorder; OCD: obsessive-compulsive disorder; ODD: oppositional defiant disorder; SUD: substance use disorder.
This study allowed the inclusion of parents with certain psychiatric disorders, except BAD and schizophrenia. Among the co-parents and parents of the control group, the number of subjects affected by a psychiatric disorder is striking; however, in said group, a significant proportion is explained by the prevalence of simple phobia. For this comparison, we believe it is important to select a group of parents who present some form of disorder, and not a “pure” control group.
This study shows that CPBD had higher prevalences of psychiatric disorders than CCP. The CPBD group showed higher prevalences of affective conditions, followed by disruptive and anxious disorders. Moreover, significant differences were found in SUDs.
These findings are similar to those of other studies with similar methodologies which support the hypothesis that the CPBD group has an increased risk of suffering a wide range of psychiatric disorders. Other authors have even reported higher prevalences of affective disorders (5–67% vs 0–38%) and non-affective disorders (5–52% vs 0–25%).12–14,37 Moreover, our findings are in line with other studies that show differences between the two groups when assessing affective,7,13,16,24,38–43 anxious11,13,16,19,20,38,42,44–49 and disruptive7,11,13,16,19,32,44,50 disorders.
Of the disruptive disorders, ADHD is the most frequent diagnosis in this sample of CPBD (28.7%). Although this ADHD figure is greater than that found in a comparison study between CPBD and CCP conducted in Brazil (11.6%),11 it is close to the prevalences reported by other authors (27%).50 In the CCP group, a prevalence of 12.7% was found, which, although higher than those reported in the literature (5.9–7.1%),51,52 is lower than those found in studies in the Paisa region (15.8–17.1%).53,54 In this respect, there are disputes in the literature when trying to define the relationship between BAD and ADHD, as some authors describe high comorbidity and family association between the two entities11,13,16,19,44 while others do not.42,47,55 Moreover, it has been described that differences would be attributable to the prevalence of ADHD in the parents, the presence of a general psychopathology in the parents (more than the exclusive presence of BAD) or methodological differences of the studies (small samples, biases in the evaluations, use of different measurement instruments, lack of specification of the type of BAD among the parents and studies with healthy control groups or with a different psychopathology to BAD).13,14
As for affective disorders, 7 subjects were found to have BAD, all of whom belonged to the CPBD group (5.5%). Likewise, higher frequencies of BAD-NOS (13.4%) were found in the risk group, with statistically significant differences. As shown, these results complement those of other authors who report higher rates of BAD in the risk group, with variable figures ranging from 2.3%20 to 33–40% of samples.16,24 This can be explained by the methodological differences between the studies, such as the inclusion of parents with different BAD subtypes (BAD-I/II-NOS), the inclusion or exclusion of children with BAD-NOS, different age groups of the children at the time of the evaluation and cross-sectional versus longitudinal studies, among others.56 The results of this study provide evidence for the discussion of these disputes, as the children come from parents with a single subtype of the disorder (BAD-I), thus representing a more homogeneous sample.
A Latin American study conducted in Brazil11 found no differences between groups when evaluating affective disorders, which could be due to the young age of the children of the sample assessed (mean, 11.2 years), since this age is not at the highest risk of developing affective disorders,47 unlike late adolescence or early adulthood. Another study conducted in Mexico reports 6.5% of CPBD with BAD-NOS, although this study has a very small sample.26
When considering anxious disorders, our results show that CPBD had higher frequencies of PTSD. This finding is striking, since the most common differences found in the different studies have been reported in SAD, GAD, social phobia and OCD.13,16,20,44–46 Given that both groups had a similar number of individuals exposed to some form of traumatic event, this finding could indicate a greater specific vulnerability to the onset of PTSD in the CPBD group. However, it should be considered that the methodology of this study does not allow definitive conclusions to be reached in this regard because potentially influential factors, such as history of PTSD in parents (the DIGS does not evaluate this diagnosis), family functioning, levels of social support and characteristics of exposure to trauma (type of trauma, frequency, intensity, single or repeated, among others)57,58 were not taken into account. As such, a study with a methodological design that includes these variables is required.
Furthermore, in this study, CPBD were found to have higher SUD frequencies and lower levels of functionality, with these findings having previously been described by other investigators.21,38,59–61
The analysis of psychiatric disorders by age group showed statistically significant differences in ADHD and SAD in the schoolchildren group, in MDD in the adolescent group, and in SUD due to PAS in the adult group. These findings are similar to those of other studies, which mention that non-affective psychopathologies (such as anxiety disorders or disruptive disorders) tend to occur earlier than affective symptoms.7,45 They also report that depressive symptoms tend to occur in adolescence and that SUDs appear in later stages of development.24,47,61 These findings have led some authors to suggest that early-onset depressive episodes in CPBD may pose some risk of BAD.7,13,38–40 It should be noted that analysis by groups is exploratory, and sample size by subgroups may prove insufficient in order to estimate the actual differences between psychiatric disorders.
In short, this CPBD group had higher frequencies of each of the three symptomatic domains evaluated (affective, anxiety and disruptive) compared to the CCP group. In this regard, some studies report that affective symptoms are forerunners to future BAD, while other longitudinal studies have found that CPBD could contract the disease beginning with any of the three symptomatic domains or any of these three pathways.7,45,47 In this sense, some authors indicate that the early evaluation of subthreshold symptoms could increase the predictive capacity for many risk subjects, which could be important for a future longitudinal study.38
This study has some limitations. First, the case group was obtained from families attending a centre with a high level of complexity and is not a representative sample of the population with BAD, so the results cannot be extrapolated to other populations of CPBD. Second, given the type of study, which was cross-sectional, it cannot be determined whether the findings obtained will be stable over time and if they actually correspond to prodrome phases of BAD. Third, although we considered the sample size to be important, it might not be sufficient to adequately estimate the differences between age groups and between low prevalence disorders. Finally, in the subgroups of adult children, recall bias could affect the reported psychopathology rates.
The strengths of this study are considered to be as follows: the presence of parents with exclusive BAD-I in the case group, allowing us to reduce the inherent heterogeneity of the disease and to achieve results that may be less influenced by confounding factors; the comparison of a CPBD group with a CCP group from the same geographical area, ensuring homogeneity between the groups and allowing us to determine the real difference in the presence of psychopathologies within this risk group; parents who presented other diseases besides BAD not being excluded from the control group, thereby increasing the external validity of the results; and the wide age range of the children used in this study, allowing us to identify most of the psychopathologies that said subjects will suffer in adulthood, including BAD and SUDs. Finally, this study contributes to the scant research available on the topic in Latin America.
ConclusionsThe findings of this study demonstrate higher rates of affective and non-affective psychiatric disorders in a group of CPBD compared to a control group from the same geographical area. CPBD may be considered a population with a high risk of psychopathology in general and, once presented, they would theoretically be deemed to have an increased risk of BAD. Longitudinal studies are required to determine prodrome symptoms or prodrome psychiatric disorders of BAD and their evolution.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
FundingThis article was funded by the Psychiatric Research Group (GIPSI) of the Universidad de Antioquia, the PRISMA Temporary Union, the Faculty of Medicine of the Universidad de Antioquia and the University Research System of the Universidad de Antioquia, CODI. This study forms part of the project “Early Detection of Severe Mental Illness in Children of Bipolar Patients Using Endophenotypes in the Genetic Isolation of Paisa residents”. Call for Biomedical and Health Sciences Papers 2012–2013, Code 8700–3250, project registered in the university research system of the Universidad de Antioquia. It forms part of the Sustainability Strategy of the Universidad de Antioquia Faculty of Medicine.
Conflicts of interestThe authors have no conflicts of interest to declare.
University research system of the Universidad de Antioquia, CODI. Sustainability Strategy of the Universidad de Antioquia Faculty of Medicine. Multimodal Intervention Programme (PRISMA). PRISMA Temporary Union: Universidad de Antioquia and COLCIENCIAS. Psychiatric Research Group (GIPSI). Mood Disorders Programme of the Hospital Universitario San Vicente Fundación.
Please cite this article as: Palacio-Ortiz JD, Peña-Quintero CE, Gómez-Valero MA, Bustamante-Gómez PA, Arroyave-Sierra PH, Vargas-Upeguí CD, et al. Trastornos psiquiátricos a través de la vida: un estudio de comparación de hijos de padres con trastorno afectivo bipolar tipo I frente a hijos de padres controles de la comunidad. Rev Colomb Psiquiat. 2017;46:129–139.