Bipolar disorder (BD) has a large hereditary component. It is a disorder that begins in early adulthood, but about which it has been described a premorbid period preceding the onset of BD. During this herald expression psychiatric disorders and symptoms, such as depressive, manic, psychotic, anxious and others, may appear.
ObjectiveTo determine the psychopathological profile of a Bipolar Offspring (BO) group compared with the Community Control Offspring (CCO) group, and its evolution over time, including subthreshold symptoms and mental disorders.
MethodsWe conducted an observational mixed cohort study, with a prospective design. We included subjects from six to 30 years of age, from the region of Antioquia, Colombia. A total of 131 subjects from the risk group BO and 150 subjects from the CCO group were evaluated through validated psychiatric diagnostic interviews (K-SADS-PL and DIGS) at baseline and at 4 years follow up. All interviews were carried out by a staff blind to parent diagnoses. Follow-up assessment were complete in 72% of the offspring. Forty-two subjects were excluded as they surpassed the age of 30 years, and only 46 subjects were not followed (change of address or did not consent to participate).
ResultsCompared with the CCO group, the BO group had a higher frequency of affective disorder, psychotic disorder, externalizing disorders and use of the psychoactive substances during both assessments at time 1 and 2. The magnitude of the differences between the groups increased when they reach time 2. The BO group had a greater risk for presenting subthreshold symptoms and definitive psychiatric disorders, such as affective disorders, psychotic disorders and externalizing disorders. In addition, the BO group had a younger age of onset for psychoactive substances consumption.
ConclusionDuring the follow-up period, the BO group had a higher risk of presenting mental disorders compared with the CCO group. The most relevant symptoms and disorders that could precede the onset of BD were depressive, bipolar not otherwise specified, psychotic and substance use.
El trastorno bipolar (TB) tiene un gran componente hereditario. Es un trastorno que comienza en la edad adulta temprana, pero acerca del cual se ha descrito un período premórbido que precede al inicio de TB. Durante esta expresión heraldo, pueden aparecer trastornos y síntomas psiquiátricos, como depresivos, maníacos, psicóticos, ansiosos y otros.
ObjetivoDeterminar el perfil psicopatológico de un grupo de hijos de padres con TB (BO) en comparación con el grupo de hijos de padres control de la misma comunidad (CCO), y su evolución en el tiempo. Los síntomas subumbrales y los trastornos mentales serán incluidos.
MétodosNosotros llevamos a cabo un estudio observacional mixto de cohorte, con diseño prospectivo. Incluimos sujetos de seis a 30 años de edad, de la región de Antioquia, Colombia. Un total de 131 sujetos del grupo de riesgo BO y 150 sujetos del grupo CCO fueron evaluados a través de entrevistas de diagnóstico psiquiátricas validadas (K-SADS-PL y DIGS), al inicio y a los 4 años de seguimiento. Todas las entrevistas se llevaron a cabo por personal ciego a los diagnósticos de los padres. La evaluación de seguimiento se completó en el 72% de la descendencia. Cuarenta y dos sujetos fueron excluidos ya que superaron la edad de 30 años, y solo 46 sujetos no fueron seguidos (cambio de dirección o no dieron su consentimiento para participar).
ResultadosEn comparación con el grupo CCO, el grupo BO tuvo una mayor frecuencia de trastorno afectivo, el trastorno psicótico, los trastornos de externalización y el uso de las sustancias psicoactivas durante ambas evaluaciones en los tiempos 1 y 2. La magnitud de las diferencias entre los grupos aumentó cuando alcanzaron el tiempo 2. El grupo BO tuvo un mayor riesgo de presentar síntomas subumbrales y trastornos psiquiátricos definitivos, tales como trastornos afectivos, trastornos psicóticos y trastornos de externalización. Además, el grupo BO tuvo una edad de comienzo más baja para el consumo de sustancias psicoactivas.
ConclusiónDurante el período de seguimiento, el grupo BO tuvo un mayor riesgo de presentar trastornos mentales en comparación con el grupo CCO. Los síntomas y trastornos más importantes que preceden al inicio del TB fueron: depresivo, bipolar no especificado de otra manera, psicóticos y el uso de sustancias.
Bipolar disorder (BD) is a severe and chronic mental disorder characterized by affective episodes of depression or mania, which significantly affects the patient's functionality.1,2 The global prevalence of the bipolar spectrum disorders (BSD) is 2.4%, distributed in BD type I 0.6%, BD type II 0.4% and BD not specified 1.4%.2,3 Its prevalence in Colombia is 1.8%.4 The disorder mainly affects people of productive age, occupying the fifth place of burden of mental illness globally.5 It has a risk of suicide up to 23 times higher than the general population, and up to three times greater than the risk of patients with Major Depressive Disorder (MDD).6
Although BD typically begins in early adulthood,7 several studies have shown premorbid psychopathology during the first two decades, such as, affective lability, depressive symptoms, subthreshold manic symptoms, symptoms of bipolar spectrum disorders, psychotic symptoms and especially MDD or subthreshold hypomanic episodes.8–15
Major affective disorders are 2.7 times more frequent in bipolar offspring (BO), compared to controls; It has been concluded that the most important risk factor for developing the condition is the family history.11,16–18 The BD heritability is estimated about 85%.1,19
Genetic studies in Colombia have been carried out in a population with BD and other diseases of hereditary transmission20,21; an initiative that arose from findings in a geographically and culturally isolated population, in which the characteristics of an isolate were confirmed, known as the “paisa genetic isolate”.22,23 These types of populations offer excellent possibilities for performing low frequency gene analysis. Thus, the group of research in psychiatry (GIPSI) of the University of Antioquia has conducted studies in this high-risk population of BO. Preliminary studies described that BO group presents subthreshold affective episodes, or affective symptoms, and high frequency of psychiatric disorders such as MDD, attention deficit hyperactivity disorder (ADHD) and separation anxiety disorder (SAD); in addition to alterations in cognitive functions such as attention, verbal fluency, working memory and processing speed.24–26
In a previous study about life time mental disorders, we found that in comparison with the community control offspring (CCO) group,26 the BO group presented a higher frequency of BD, unspecified BD, MDD, substance use disorder (SUD), alcohol use disorder, ADHD, oppositional defiant disorder (ODD) and post-traumatic stress disorder (PTSD).
Prospective studies in the BO population in the United States,11,27–29 Canada,14,19 Netherlands,30 and Switzerland,31 had documented precursors of BD such as: depressive episodes, sleep disturbances, subthreshold mania episodes, subthreshold psychotic episodes, psychotic symptoms during an affective episode, disruptive disorders and, to a lesser extent, symptoms of anxiety disorders.32
To our knowledge, there is only one prospective study in a genetically isolated population about a population at risk of presenting BD.29
This is the continuation of a study 26whose main objective was to determine the psychopathological profile of the BO group compared to the CCO group, and to evaluate its evolution in a time 2 assessment, in subjects from the paisa genetic isolated.
Materials and methodsThis is an observational study of a mixed cohort, with a prospective design. It is a continuation of the study “Psychiatric disorders through life”, which time 1 assessment was completed in 2014.26 The current data were obtained in an evaluation 3-4 years later (time 2 assessment), with a cut-off date of December 2017.
This is part of the “Cambios tempranos en población de alto riesgo para trastorno afectivo bipolar tipo I: comparación de trastornos psiquiátricos, alteraciones del sueño y neuroimágenes entre hijos de pacientes con trastorno afectivo bipolar versus controles” project, that was approved by the University of Antioquia's Bioethics Committee and the research ethics committee of the Hospital San Vicente Fundación. All ethical principles for medical research in humans of the Declaration of Helsinki were fulfilled.33 The informed consent was completed before every evaluation of parents, co-parents and offspring's (the minors granted informed assent).
Sample selectionDetails of subject selection methodology could be found in a previous paper.26
Parents of exposed subjectsPatients belonging to the genetic isolate “paisa”, diagnosed BD type-I by using the Interview Diagnostic Interview for Genetic Studies (DIGS) 34validated in Colombia,35 according to criteria of the Diagnostic and Statistical Manual of Mental Disorders fourth revised edition (DSM IV- TR).36
Parents of subjects not exposedCommunity people originally from the same geographical area, who did not have a diagnosis of BD or psychotic disorders according to the DIGS, and who did not have first-degree relatives with BD. The presence of depressive or anxiety disorders was allowed. These parents were matched by age, sex, and housing area (??urban or rural).
Study populationThe risk BO group and the CCO group of subjects were already assessed in 2014 (time 1).26 They were recruited aged from 6 to 30 years, and also with a Paisa origin in at least two generations. At time 1, subjects with diagnoses of mental disorders secondary to medical conditions or medication use were excluded. Subjects with moderate/severe cognitive disability, classic autism according to DSM IV-TR criteria were also excluded. The CCO group consisted of children of community parents. Parents of these children, did not have psychotic disorder or bipolar spectrum, and did not have first-degree relatives with BD.
Sample sizeThe sample size for the study at time 1 26was calculated from a psychiatric disorder prevalence of 16% in BO,37 a power of 80% and a type I error of 5%. With a sample of 90 subjects for the BO group and 90 subjects for the CCO group (with Yates correction, 100 BO and 101 CCO) and with a margin of losses of 20%, the final sample was planned with 126 BO subjects and 128 CCO subjects.26 At time 2, we started with the sample already studied at time 1 of 127 BO subjects, and 150 CCO subjects. Four subjects who had been evaluated in time 1, were added to the BO group, they were not included in the publication since they were in the process of evaluation during the cut-off point.
InstrumentsSchedule for Affective Disorders and Schizophrenia for School Aged Children Lifetime (K-SADS-PL) 38validated for Latin America.39–41 It is a semi-structured diagnostic interview designed to evaluate current and past episodes of psychopathology according to the DSM-5 criteria. It identifies the presence of several definitive mental disorders, and can identify subthreshold symptoms of the different disorders. It has good inter-rater performance in the Latin American version. Good to excellent kappa coefficients have been quantified for MDD κ=0.76, any anxiety disorder κ=0.84, ADHD κ=0.9 and conduct disorder (CD) κ=1.39–41 It has a PTSD component that assesses the presence of the following stressful events: car accidents, other accidents, fires, witnessing a natural disaster, being a witness or victim of a violent crime, having received traumatic news, witnessing terrorist acts, having witnessed war-like conflicts, witness domestic violence, be a victim of physical abuse or sexual abuse and others.
DIGS Colombian validated version.35 It is a semi-structured diagnostic interview, designed to evaluate psychiatric disorders, in genetic studies. This instrument evaluates mood and psychotic disorders, substance use disorders, anxiety disorders, eating behavior disorders and others.
Children's Global Assessment Scale (CGAS) is an instrument to provide a global measure of the functioning level in children and adolescents.42 The measure provides a global rating, on a scale of 0-100 in a hypothetical health-disease continuum.43
Global Assessment of Functioning scale (GAF) is widely used in the DSM-IV,36 which provides a subjective appreciation on a scale of 0 to 100, in a hypothetical health-disease continuum, about the individual's general functioning.
ProceduresSubjects from BO or CCO groups under 18 years old were assessed with K-SADS-PL-5 Latin American version,36,37 to determine the presence of subthreshold symptoms, and episodes of psychiatric diagnoses. Additionally, the CGAS was carried out.42 Subjects older than 18 years old were assessed with the DIGS. In addition, sections of the K-SADS-PL-5 were carried out, including simple anxiety disorder (SAD), specific phobia, generalized anxiety disorder (GAD), ADHD, ODD, CD, disruptive mood dysregulation disorder (DMDD), non-suicidal self-injury (NSSI) and PTSD. The GAF for each subject was also carried out.
The interviews were applied by a psychiatry resident or a psychiatrist previously trained in the use of DIGS and K-SADS-PL-5, who were blind to the parents’ diagnosis. For the Best Estimated procedure; two expert psychiatrists, who did not conduct the diagnostic interviews, corroborated the psychiatric diagnosis of each individual. When they did not agree, a third expert evaluator was consulted. When a diagnosis was found during the evaluation, the evaluated subject was immediately referred to the national health system service.
VariablesThe following demographic variables were considered: sex, age, schooling (in years), number of schooling failing years, housing area (rural or urban), and socio-economic status (SES). Colombian SES is divided into 6 levels: lowest status from 1 to 3, and highest status from 4 to 6. The clinical variables were obtained from the DIGS and K-SADS-PL-5 interviews: Depressive episode, subthreshold depressive symptoms, MDD, BD, unspecified BD symptoms, BSD and episodes, psychosis, subthreshold psychotic symptoms, psychotic symptoms associated with BSD, panic disorder, SAD, social anxiety disorder, agoraphobia, simple phobia, GAD, obsessive-compulsive disorder, anorexia or bulimia, ADHD, ODD, CD, PTSD, experimental use of tobacco, regular use of tobacco, experimental use of liquor, abuse or dependence on alcohol, experimental use of psychoactive substances (PS) and SUD. The age of onset of psychiatric disorder or subthreshold psychiatric symptoms were included.
Statistical analysisThe qualitative variables were evaluated using frequencies and percentages, and the quantitative variables were evaluated using measures of central tendency and dispersion. The t-test was used for quantitative variables of normal distribution (i.e.: schooling) and the U of Mann-Whitney and W of Wilcoxon for non-normal distribution quantitative variables (i.e.: schooling failing years, functionality scales and age of onset of any psychiatric disorder). For the analysis of clinical variables differences, Pearson Chi-square test for independence and Fisher's exact test were used (when there were no cases in a given group). The odds ratio (OR) prevalence was calculated with 95% confidence intervals. A logistic regression analysis was performed with the variables of: age, sex, housing area, schooling and socioeconomic level. Same procedure was used for the analysis of psychiatric disorders groups: internalizing (anxiety and depression) externalizing (ADHD, ODD, or CD) and SUD. McNemar and McNemar-Bowker test were used to evaluated evolution of this cohort over time, and the statistical significance of the diagnostic changes for every single subject.
The Kaplan-Meier procedures, Log-Rank and Cox regression were used to assess the accumulated frequencies of psychiatric disorders of the two groups by the age, in addition to evaluate the influence of the sociodemographic factors: age, sex, housing area, schooling, socioeconomic level and stressful events. Subjects with subthreshold symptoms of each psychiatric disorder were included to assess premorbid trajectories. A level of significance of 0.05 was established for all statistical tests. Data analysis was carried out in an IBM SPSS Statistics version 23 software.
ResultsThe characteristics of the parents with BD, their spouses (co-parents) and control parents from whom the initial cohort was obtained in 2014, were described in the preliminary study.26
Follow-upWe started with a cohort obtained from the preliminary studies: 150 subjects from CCO group and 131 subjects from BO group.24–26 The retention was 72% and 66% respectively. We excluded 42 subjects who exceeded the age of 30 at time 2 (26 CCO and 16 BO). We were not able to follow-up 46 subjects (they did not attend to the appointment, did not wish to participate, or contact information was not updated). Three subjects from the BO cohort died after time 1 (two suicide cases and one homicide case), they were not considered for the statistical analysis, as it was not part of the analysis protocol.
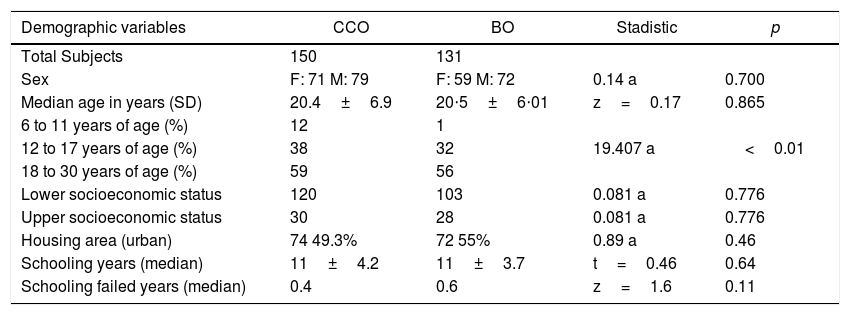
DemographicsThe BO group was similar to the CCO group at time 2, in terms of sex, age, socioeconomic status, housing area, schooling, and repeated school years.
Functionality ScalesThe BO group had a higher risk of having a functionality score lower than 70 points OR 3.4 (95% CI 2.0 - 5.8, p<0.01). The CCO group had a median functionality score higher than the BO, and was statistically significant (see Table 1).
Sample demographic features and functionality scales.
| Demographic variables | CCO | BO | Stadistic | p |
|---|---|---|---|---|
| Total Subjects | 150 | 131 | ||
| Sex | F: 71 M: 79 | F: 59 M: 72 | 0.14 a | 0.700 |
| Median age in years (SD) | 20.4±6.9 | 20⋅5±6⋅01 | z=0.17 | 0.865 |
| 6 to 11 years of age (%) | 12 | 1 | ||
| 12 to 17 years of age (%) | 38 | 32 | 19.407 a | <0.01 |
| 18 to 30 years of age (%) | 59 | 56 | ||
| Lower socioeconomic status | 120 | 103 | 0.081 a | 0.776 |
| Upper socioeconomic status | 30 | 28 | 0.081 a | 0.776 |
| Housing area (urban) | 74 49.3% | 72 55% | 0.89 a | 0.46 |
| Schooling years (median) | 11±4.2 | 11±3.7 | t=0.46 | 0.64 |
| Schooling failed years (median) | 0.4 | 0.6 | z=1.6 | 0.11 |
| Functionality scales (weighted mean) | CCO | BO | z | p |
|---|---|---|---|---|
| CGAS score during evaluation at time 2 | 90±20 | 80±20 | -2.742 | 0.01 |
| CGAS lower score during a lifetime | 80±30 | 65±19 | -3.395 | <0.01 |
| CGAS higher score during a lifetime | 90±20 | 85±21 | -2.867 | <0.01 |
| Any functionality scale: lower score | 85±30 | 70±25 | -6.160 | <0.01 |
| GAF score during evaluation at time 2 | 100±5 | 90±14 | -6.763 | <0.01 |
| GAF lower score during a lifetime | 95±20 | 75±39 | -5.895 | <0.01 |
F: female, M: male, CCO: community controls offspring, BO: bipolar offspring, Low socioeconomic status: levels 1,2 or 3, High socioeconomic status: levels 4, 5 or 6, CGAS: Children's Global Assessment Scale, GAF: Global Assessment Functioning Scale, a: Pearson Chi-square test, t: t-test, z: proximity to the normal, U: U of Mann-Whitney
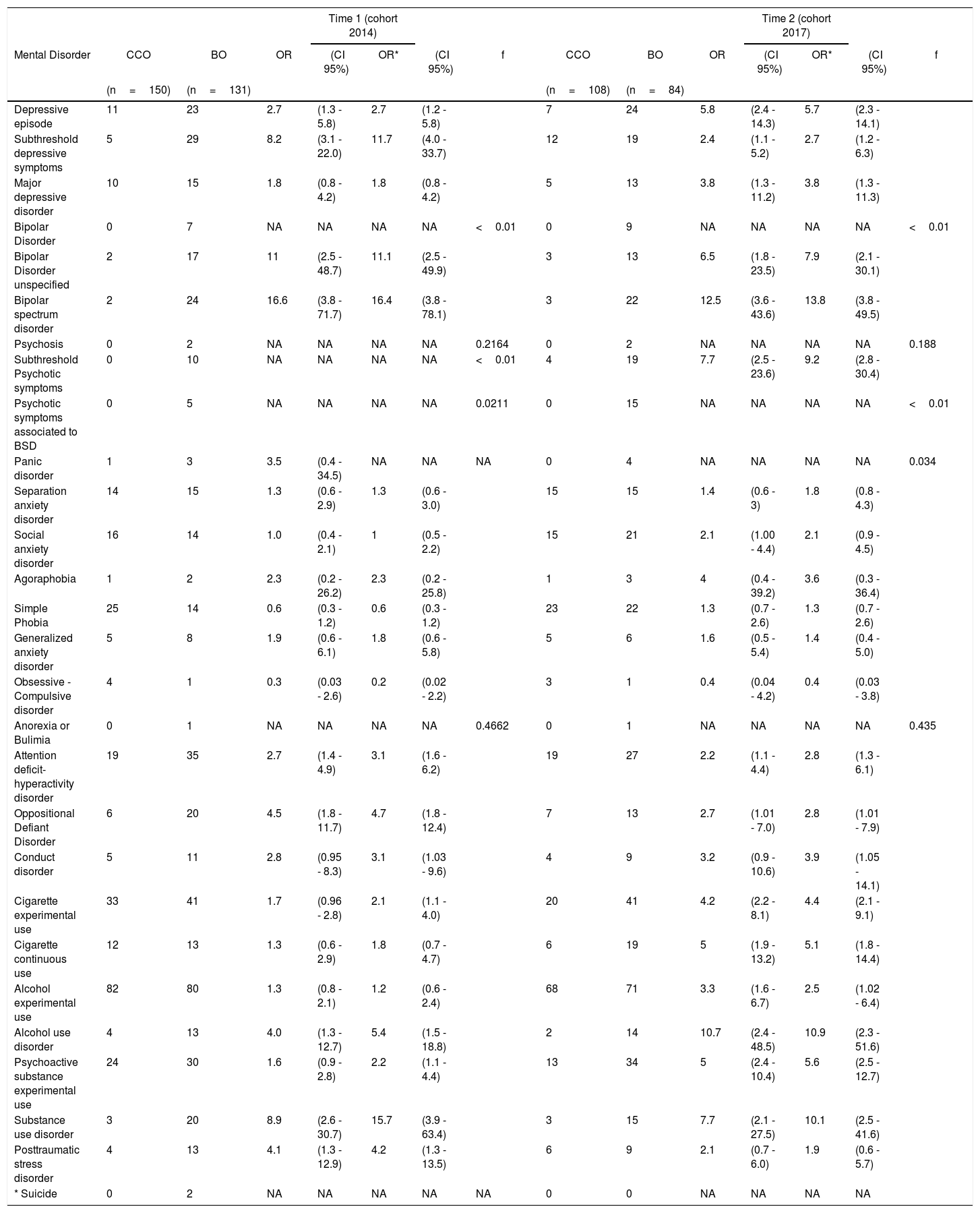
The associations observed in time 1 are maintained. Assessment at time 2 showed that there is an increased in the association magnitude. Significant OR were found mainly in MDD, BD, subthreshold psychotic symptoms, ADHD, ODD, SUD, and cigarette or alcohol use disorder. There was no statistically significant change after the adjusted analysis (see Table 2).
Mental disorders in CCO and BO during evaluation at time 1 and follow-up at time 2.
| Time 1 (cohort 2014) | Time 2 (cohort 2017) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mental Disorder | CCO | BO | OR | (CI 95%) | OR* | (CI 95%) | f | CCO | BO | OR | (CI 95%) | OR* | (CI 95%) | f |
| (n=150) | (n=131) | (n=108) | (n=84) | |||||||||||
| Depressive episode | 11 | 23 | 2.7 | (1.3 - 5.8) | 2.7 | (1.2 - 5.8) | 7 | 24 | 5.8 | (2.4 - 14.3) | 5.7 | (2.3 - 14.1) | ||
| Subthreshold depressive symptoms | 5 | 29 | 8.2 | (3.1 - 22.0) | 11.7 | (4.0 - 33.7) | 12 | 19 | 2.4 | (1.1 - 5.2) | 2.7 | (1.2 - 6.3) | ||
| Major depressive disorder | 10 | 15 | 1.8 | (0.8 - 4.2) | 1.8 | (0.8 - 4.2) | 5 | 13 | 3.8 | (1.3 - 11.2) | 3.8 | (1.3 - 11.3) | ||
| Bipolar Disorder | 0 | 7 | NA | NA | NA | NA | <0.01 | 0 | 9 | NA | NA | NA | NA | <0.01 |
| Bipolar Disorder unspecified | 2 | 17 | 11 | (2.5 - 48.7) | 11.1 | (2.5 - 49.9) | 3 | 13 | 6.5 | (1.8 - 23.5) | 7.9 | (2.1 - 30.1) | ||
| Bipolar spectrum disorder | 2 | 24 | 16.6 | (3.8 - 71.7) | 16.4 | (3.8 - 78.1) | 3 | 22 | 12.5 | (3.6 - 43.6) | 13.8 | (3.8 - 49.5) | ||
| Psychosis | 0 | 2 | NA | NA | NA | NA | 0.2164 | 0 | 2 | NA | NA | NA | NA | 0.188 |
| Subthreshold Psychotic symptoms | 0 | 10 | NA | NA | NA | NA | <0.01 | 4 | 19 | 7.7 | (2.5 - 23.6) | 9.2 | (2.8 - 30.4) | |
| Psychotic symptoms associated to BSD | 0 | 5 | NA | NA | NA | NA | 0.0211 | 0 | 15 | NA | NA | NA | NA | <0.01 |
| Panic disorder | 1 | 3 | 3.5 | (0.4 - 34.5) | NA | NA | NA | 0 | 4 | NA | NA | NA | NA | 0.034 |
| Separation anxiety disorder | 14 | 15 | 1.3 | (0.6 - 2.9) | 1.3 | (0.6 - 3.0) | 15 | 15 | 1.4 | (0.6 - 3) | 1.8 | (0.8 - 4.3) | ||
| Social anxiety disorder | 16 | 14 | 1.0 | (0.4 - 2.1) | 1 | (0.5 - 2.2) | 15 | 21 | 2.1 | (1.00 - 4.4) | 2.1 | (0.9 - 4.5) | ||
| Agoraphobia | 1 | 2 | 2.3 | (0.2 - 26.2) | 2.3 | (0.2 - 25.8) | 1 | 3 | 4 | (0.4 - 39.2) | 3.6 | (0.3 - 36.4) | ||
| Simple Phobia | 25 | 14 | 0.6 | (0.3 - 1.2) | 0.6 | (0.3 - 1.2) | 23 | 22 | 1.3 | (0.7 - 2.6) | 1.3 | (0.7 - 2.6) | ||
| Generalized anxiety disorder | 5 | 8 | 1.9 | (0.6 - 6.1) | 1.8 | (0.6 - 5.8) | 5 | 6 | 1.6 | (0.5 - 5.4) | 1.4 | (0.4 - 5.0) | ||
| Obsessive - Compulsive disorder | 4 | 1 | 0.3 | (0.03 - 2.6) | 0.2 | (0.02 - 2.2) | 3 | 1 | 0.4 | (0.04 - 4.2) | 0.4 | (0.03 - 3.8) | ||
| Anorexia or Bulimia | 0 | 1 | NA | NA | NA | NA | 0.4662 | 0 | 1 | NA | NA | NA | NA | 0.435 |
| Attention deficit-hyperactivity disorder | 19 | 35 | 2.7 | (1.4 - 4.9) | 3.1 | (1.6 - 6.2) | 19 | 27 | 2.2 | (1.1 - 4.4) | 2.8 | (1.3 - 6.1) | ||
| Oppositional Defiant Disorder | 6 | 20 | 4.5 | (1.8 - 11.7) | 4.7 | (1.8 - 12.4) | 7 | 13 | 2.7 | (1.01 - 7.0) | 2.8 | (1.01 - 7.9) | ||
| Conduct disorder | 5 | 11 | 2.8 | (0.95 - 8.3) | 3.1 | (1.03 - 9.6) | 4 | 9 | 3.2 | (0.9 - 10.6) | 3.9 | (1.05 - 14.1) | ||
| Cigarette experimental use | 33 | 41 | 1.7 | (0.96 - 2.8) | 2.1 | (1.1 - 4.0) | 20 | 41 | 4.2 | (2.2 - 8.1) | 4.4 | (2.1 - 9.1) | ||
| Cigarette continuous use | 12 | 13 | 1.3 | (0.6 - 2.9) | 1.8 | (0.7 - 4.7) | 6 | 19 | 5 | (1.9 - 13.2) | 5.1 | (1.8 - 14.4) | ||
| Alcohol experimental use | 82 | 80 | 1.3 | (0.8 - 2.1) | 1.2 | (0.6 - 2.4) | 68 | 71 | 3.3 | (1.6 - 6.7) | 2.5 | (1.02 - 6.4) | ||
| Alcohol use disorder | 4 | 13 | 4.0 | (1.3 - 12.7) | 5.4 | (1.5 - 18.8) | 2 | 14 | 10.7 | (2.4 - 48.5) | 10.9 | (2.3 - 51.6) | ||
| Psychoactive substance experimental use | 24 | 30 | 1.6 | (0.9 - 2.8) | 2.2 | (1.1 - 4.4) | 13 | 34 | 5 | (2.4 - 10.4) | 5.6 | (2.5 - 12.7) | ||
| Substance use disorder | 3 | 20 | 8.9 | (2.6 - 30.7) | 15.7 | (3.9 - 63.4) | 3 | 15 | 7.7 | (2.1 - 27.5) | 10.1 | (2.5 - 41.6) | ||
| Posttraumatic stress disorder | 4 | 13 | 4.1 | (1.3 - 12.9) | 4.2 | (1.3 - 13.5) | 6 | 9 | 2.1 | (0.7 - 6.0) | 1.9 | (0.6 - 5.7) | ||
| * Suicide | 0 | 2 | NA | NA | NA | NA | NA | 0 | 0 | NA | NA | NA | NA | |
CCO: community controls offspring, BO: bipolar offspring, BSD: Bipolar spectrum disorder, n: number, OR: Odds ratio, OR*: adjusted Odds Ratio, NA: Not applicable, CI95%: confidence interval 95%, f: exact Fishers test, * suicide cases (not included for analysis).
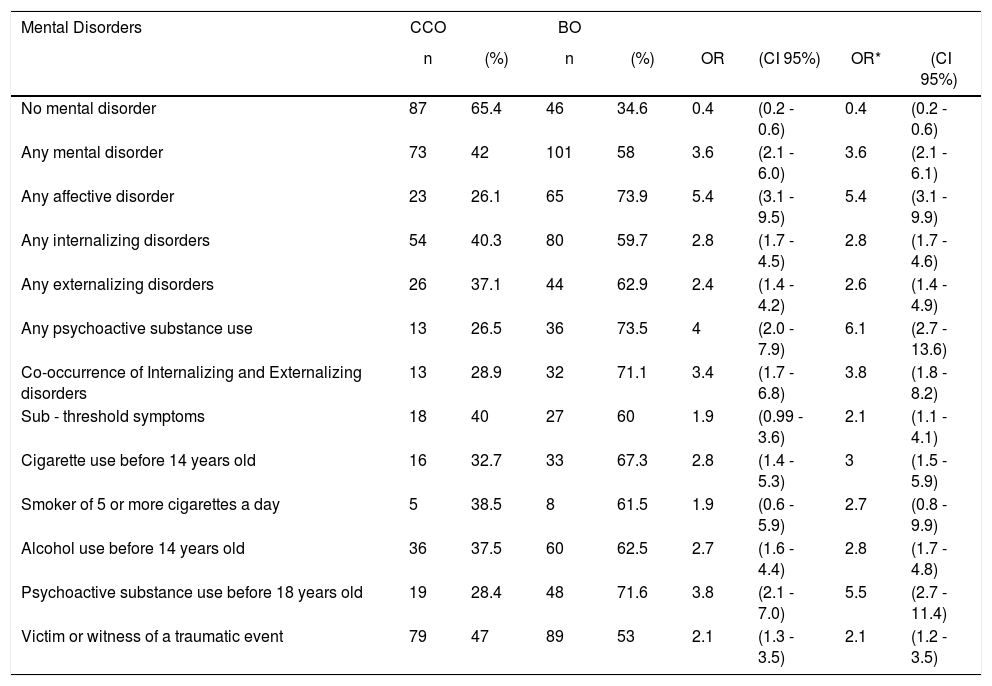
The new DSM-5 diagnostic proposals such as DMDD, NSSI, selective mutism, intermittent explosive disorder, limited prosocial emotions and avoidant food restrictive ingestion disorder were evaluated only at time 2. There were no significant differences between the groups. Only three cases of NSSI were found in the BO group versus zero in the CCO group (Fisher's exact test:0.008). Table 3 shows the differences between the groups (see Table 3).
Global Analysis of mental disorders.
| Mental Disorders | CCO | BO | ||||||
|---|---|---|---|---|---|---|---|---|
| n | (%) | n | (%) | OR | (CI 95%) | OR* | (CI 95%) | |
| No mental disorder | 87 | 65.4 | 46 | 34.6 | 0.4 | (0.2 - 0.6) | 0.4 | (0.2 - 0.6) |
| Any mental disorder | 73 | 42 | 101 | 58 | 3.6 | (2.1 - 6.0) | 3.6 | (2.1 - 6.1) |
| Any affective disorder | 23 | 26.1 | 65 | 73.9 | 5.4 | (3.1 - 9.5) | 5.4 | (3.1 - 9.9) |
| Any internalizing disorders | 54 | 40.3 | 80 | 59.7 | 2.8 | (1.7 - 4.5) | 2.8 | (1.7 - 4.6) |
| Any externalizing disorders | 26 | 37.1 | 44 | 62.9 | 2.4 | (1.4 - 4.2) | 2.6 | (1.4 - 4.9) |
| Any psychoactive substance use | 13 | 26.5 | 36 | 73.5 | 4 | (2.0 - 7.9) | 6.1 | (2.7 - 13.6) |
| Co-occurrence of Internalizing and Externalizing disorders | 13 | 28.9 | 32 | 71.1 | 3.4 | (1.7 - 6.8) | 3.8 | (1.8 - 8.2) |
| Sub - threshold symptoms | 18 | 40 | 27 | 60 | 1.9 | (0.99 - 3.6) | 2.1 | (1.1 - 4.1) |
| Cigarette use before 14 years old | 16 | 32.7 | 33 | 67.3 | 2.8 | (1.4 - 5.3) | 3 | (1.5 - 5.9) |
| Smoker of 5 or more cigarettes a day | 5 | 38.5 | 8 | 61.5 | 1.9 | (0.6 - 5.9) | 2.7 | (0.8 - 9.9) |
| Alcohol use before 14 years old | 36 | 37.5 | 60 | 62.5 | 2.7 | (1.6 - 4.4) | 2.8 | (1.7 - 4.8) |
| Psychoactive substance use before 18 years old | 19 | 28.4 | 48 | 71.6 | 3.8 | (2.1 - 7.0) | 5.5 | (2.7 - 11.4) |
| Victim or witness of a traumatic event | 79 | 47 | 89 | 53 | 2.1 | (1.3 - 3.5) | 2.1 | (1.2 - 3.5) |
CCO: community controls offspring, BO: bipolar offspring, n: number, %: percentage, OR: Odds ratio, OR*: adjusted Odds Ratio, NA: Not applicable, CI95%: confidence interval 95%, Internalizing disorders: major depression disorder or any anxiety disorders, Externalizing disorders: attention deficit-hyperactivity disorder, oppositional defiant disorder or conduct disorder.
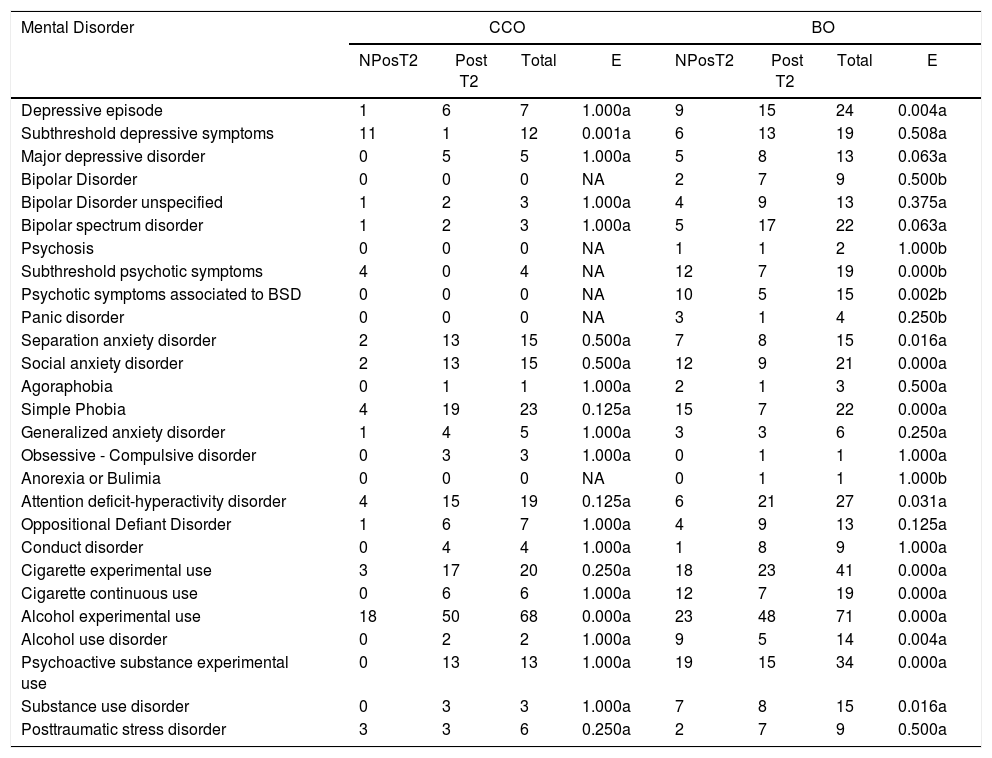
The BO group members had a statistically significant tendency to change their diagnosis from negative to positive. This was especially true for MDD, SAD, social anxiety disorder, simple phobias, ADHD, SUD and subthreshold psychotic symptoms. In addition, most of those who had a positive diagnosis condition at time 1 did not change at the time 2 assessment (see Table 4).
New positive cases in time 2 from negative cases in time 1, and cases that persisted positive.
| Mental Disorder | CCO | BO | ||||||
|---|---|---|---|---|---|---|---|---|
| NPosT2 | Post T2 | Total | E | NPosT2 | Post T2 | Total | E | |
| Depressive episode | 1 | 6 | 7 | 1.000a | 9 | 15 | 24 | 0.004a |
| Subthreshold depressive symptoms | 11 | 1 | 12 | 0.001a | 6 | 13 | 19 | 0.508a |
| Major depressive disorder | 0 | 5 | 5 | 1.000a | 5 | 8 | 13 | 0.063a |
| Bipolar Disorder | 0 | 0 | 0 | NA | 2 | 7 | 9 | 0.500b |
| Bipolar Disorder unspecified | 1 | 2 | 3 | 1.000a | 4 | 9 | 13 | 0.375a |
| Bipolar spectrum disorder | 1 | 2 | 3 | 1.000a | 5 | 17 | 22 | 0.063a |
| Psychosis | 0 | 0 | 0 | NA | 1 | 1 | 2 | 1.000b |
| Subthreshold psychotic symptoms | 4 | 0 | 4 | NA | 12 | 7 | 19 | 0.000b |
| Psychotic symptoms associated to BSD | 0 | 0 | 0 | NA | 10 | 5 | 15 | 0.002b |
| Panic disorder | 0 | 0 | 0 | NA | 3 | 1 | 4 | 0.250b |
| Separation anxiety disorder | 2 | 13 | 15 | 0.500a | 7 | 8 | 15 | 0.016a |
| Social anxiety disorder | 2 | 13 | 15 | 0.500a | 12 | 9 | 21 | 0.000a |
| Agoraphobia | 0 | 1 | 1 | 1.000a | 2 | 1 | 3 | 0.500a |
| Simple Phobia | 4 | 19 | 23 | 0.125a | 15 | 7 | 22 | 0.000a |
| Generalized anxiety disorder | 1 | 4 | 5 | 1.000a | 3 | 3 | 6 | 0.250a |
| Obsessive - Compulsive disorder | 0 | 3 | 3 | 1.000a | 0 | 1 | 1 | 1.000a |
| Anorexia or Bulimia | 0 | 0 | 0 | NA | 0 | 1 | 1 | 1.000b |
| Attention deficit-hyperactivity disorder | 4 | 15 | 19 | 0.125a | 6 | 21 | 27 | 0.031a |
| Oppositional Defiant Disorder | 1 | 6 | 7 | 1.000a | 4 | 9 | 13 | 0.125a |
| Conduct disorder | 0 | 4 | 4 | 1.000a | 1 | 8 | 9 | 1.000a |
| Cigarette experimental use | 3 | 17 | 20 | 0.250a | 18 | 23 | 41 | 0.000a |
| Cigarette continuous use | 0 | 6 | 6 | 1.000a | 12 | 7 | 19 | 0.000a |
| Alcohol experimental use | 18 | 50 | 68 | 0.000a | 23 | 48 | 71 | 0.000a |
| Alcohol use disorder | 0 | 2 | 2 | 1.000a | 9 | 5 | 14 | 0.004a |
| Psychoactive substance experimental use | 0 | 13 | 13 | 1.000a | 19 | 15 | 34 | 0.000a |
| Substance use disorder | 0 | 3 | 3 | 1.000a | 7 | 8 | 15 | 0.016a |
| Posttraumatic stress disorder | 3 | 3 | 6 | 0.250a | 2 | 7 | 9 | 0.500a |
CCO: community controls offspring, BO: bipolar offspring, BSD: Bipolar spectrum disorder, NPos T2: New positive cases in time 2 from negative cases in time 1, PosT2: cases that persisted positive from time 1, E: statistical significance according to the McNear test p<0.05, a: binominal distribution McNemar test, b: Binominal distribution McNemar-Bowker test.
At the time 2 assessment, we found out 11 subjects with a new diagnosis of unspecified BD. These subjects presented other diagnosis during the time 1 assessment: two had subthreshold depressive symptoms, two had SAD, two had ADHD, four had ODD, six had CD, and two had cases presented SUD.
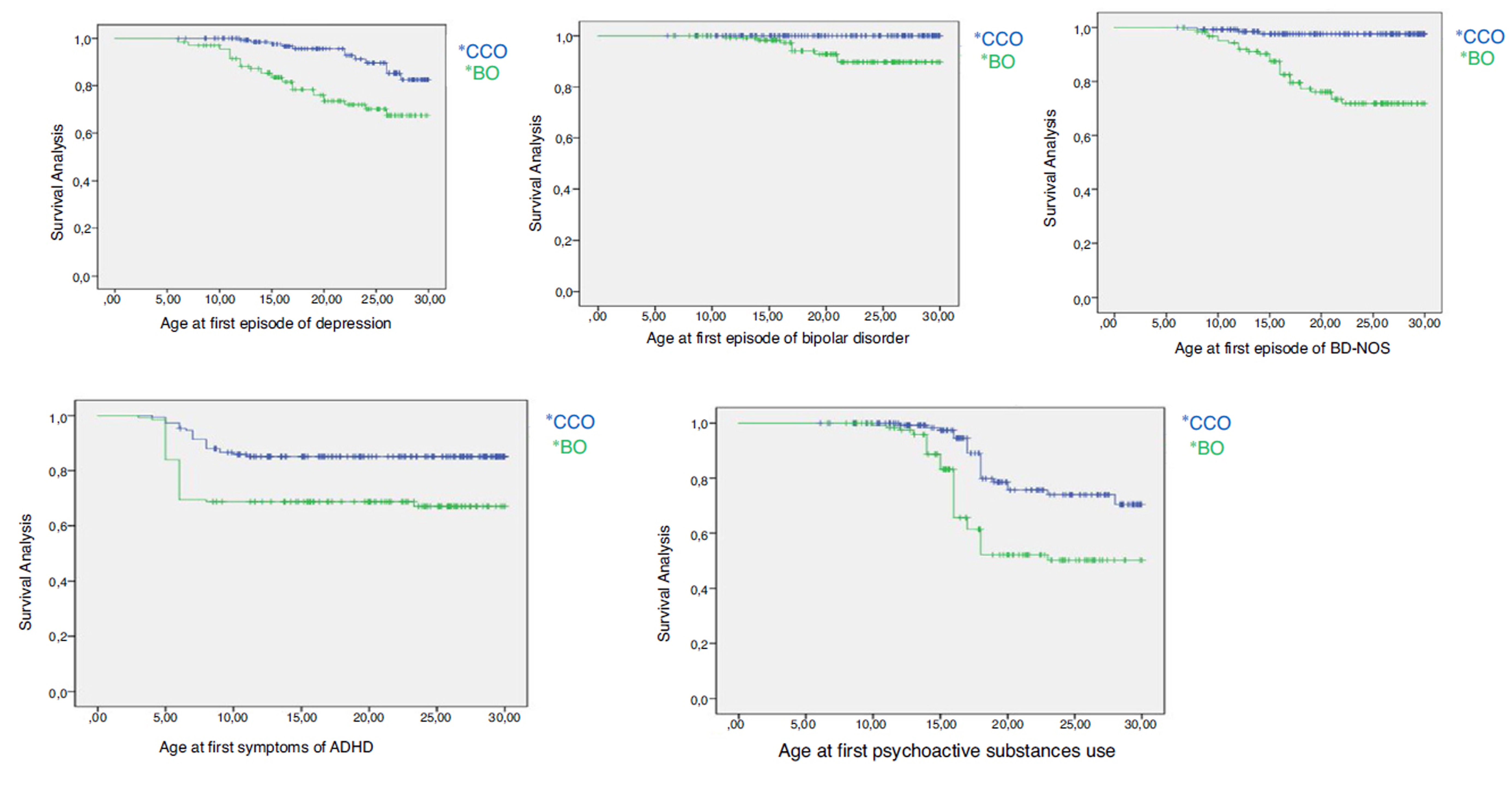
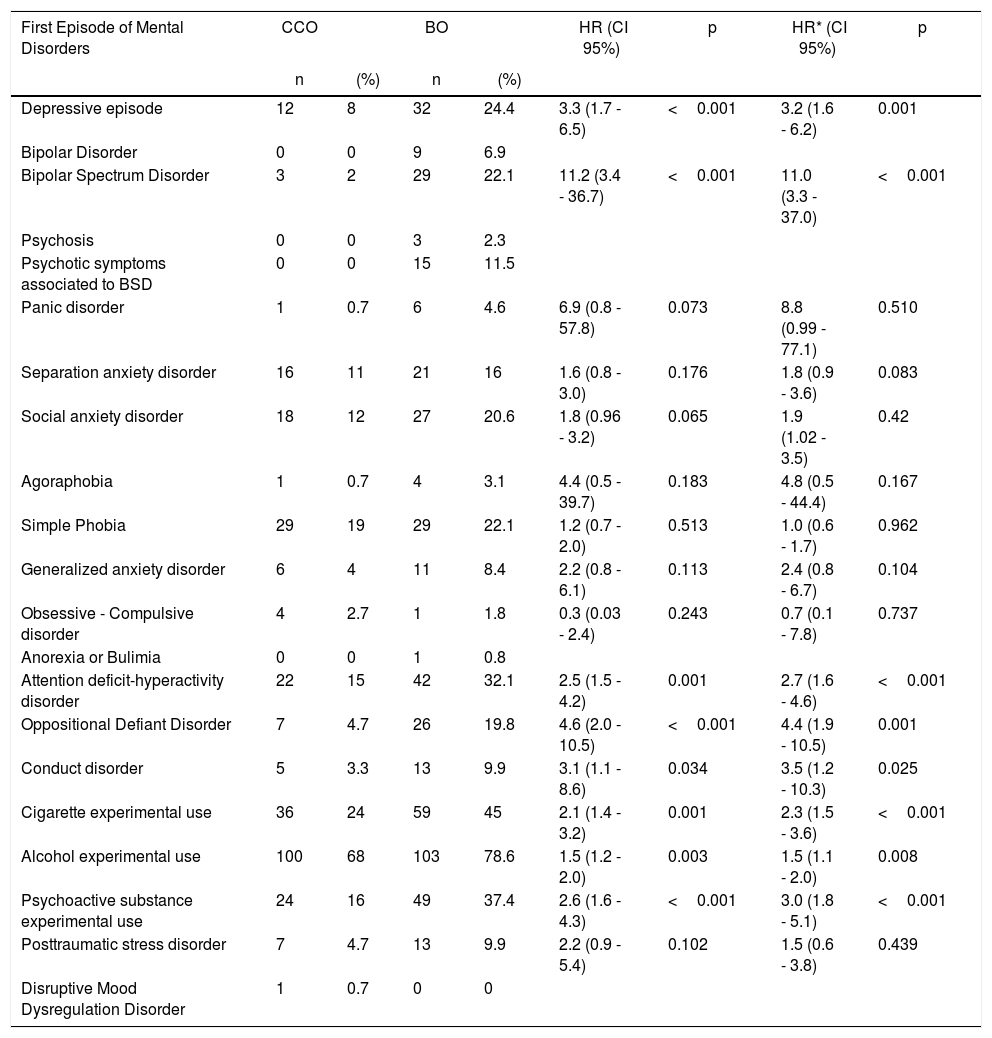
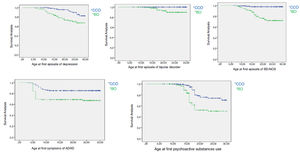
When analyzing the cases of psychiatric disorders over time, we founded out that the probability of having MDD, bipolar spectrum, ADHD, ODD, CD and starting consumption of PS was significantly higher in the BO group. (See Table 5 and Figure 1).
Survival analysis, mental disorders onset.
| First Episode of Mental Disorders | CCO | BO | HR (CI 95%) | p | HR* (CI 95%) | p | ||
|---|---|---|---|---|---|---|---|---|
| n | (%) | n | (%) | |||||
| Depressive episode | 12 | 8 | 32 | 24.4 | 3.3 (1.7 - 6.5) | <0.001 | 3.2 (1.6 - 6.2) | 0.001 |
| Bipolar Disorder | 0 | 0 | 9 | 6.9 | ||||
| Bipolar Spectrum Disorder | 3 | 2 | 29 | 22.1 | 11.2 (3.4 - 36.7) | <0.001 | 11.0 (3.3 - 37.0) | <0.001 |
| Psychosis | 0 | 0 | 3 | 2.3 | ||||
| Psychotic symptoms associated to BSD | 0 | 0 | 15 | 11.5 | ||||
| Panic disorder | 1 | 0.7 | 6 | 4.6 | 6.9 (0.8 - 57.8) | 0.073 | 8.8 (0.99 - 77.1) | 0.510 |
| Separation anxiety disorder | 16 | 11 | 21 | 16 | 1.6 (0.8 - 3.0) | 0.176 | 1.8 (0.9 - 3.6) | 0.083 |
| Social anxiety disorder | 18 | 12 | 27 | 20.6 | 1.8 (0.96 - 3.2) | 0.065 | 1.9 (1.02 - 3.5) | 0.42 |
| Agoraphobia | 1 | 0.7 | 4 | 3.1 | 4.4 (0.5 - 39.7) | 0.183 | 4.8 (0.5 - 44.4) | 0.167 |
| Simple Phobia | 29 | 19 | 29 | 22.1 | 1.2 (0.7 - 2.0) | 0.513 | 1.0 (0.6 - 1.7) | 0.962 |
| Generalized anxiety disorder | 6 | 4 | 11 | 8.4 | 2.2 (0.8 - 6.1) | 0.113 | 2.4 (0.8 - 6.7) | 0.104 |
| Obsessive - Compulsive disorder | 4 | 2.7 | 1 | 1.8 | 0.3 (0.03 - 2.4) | 0.243 | 0.7 (0.1 - 7.8) | 0.737 |
| Anorexia or Bulimia | 0 | 0 | 1 | 0.8 | ||||
| Attention deficit-hyperactivity disorder | 22 | 15 | 42 | 32.1 | 2.5 (1.5 - 4.2) | 0.001 | 2.7 (1.6 - 4.6) | <0.001 |
| Oppositional Defiant Disorder | 7 | 4.7 | 26 | 19.8 | 4.6 (2.0 - 10.5) | <0.001 | 4.4 (1.9 - 10.5) | 0.001 |
| Conduct disorder | 5 | 3.3 | 13 | 9.9 | 3.1 (1.1 - 8.6) | 0.034 | 3.5 (1.2 - 10.3) | 0.025 |
| Cigarette experimental use | 36 | 24 | 59 | 45 | 2.1 (1.4 - 3.2) | 0.001 | 2.3 (1.5 - 3.6) | <0.001 |
| Alcohol experimental use | 100 | 68 | 103 | 78.6 | 1.5 (1.2 - 2.0) | 0.003 | 1.5 (1.1 - 2.0) | 0.008 |
| Psychoactive substance experimental use | 24 | 16 | 49 | 37.4 | 2.6 (1.6 - 4.3) | <0.001 | 3.0 (1.8 - 5.1) | <0.001 |
| Posttraumatic stress disorder | 7 | 4.7 | 13 | 9.9 | 2.2 (0.9 - 5.4) | 0.102 | 1.5 (0.6 - 3.8) | 0.439 |
| Disruptive Mood Dysregulation Disorder | 1 | 0.7 | 0 | 0 |
CCO: community controls offspring, BO: bipolar offspring, n: number, %: percentage, HR: hazard ratio, CI95%: confidence interval 95%,*: adjusted by demographic variables (sex, age, socioeconomic status, schooling, housing area, traumatic events), BSD: Bipolar Spectrum Disorder
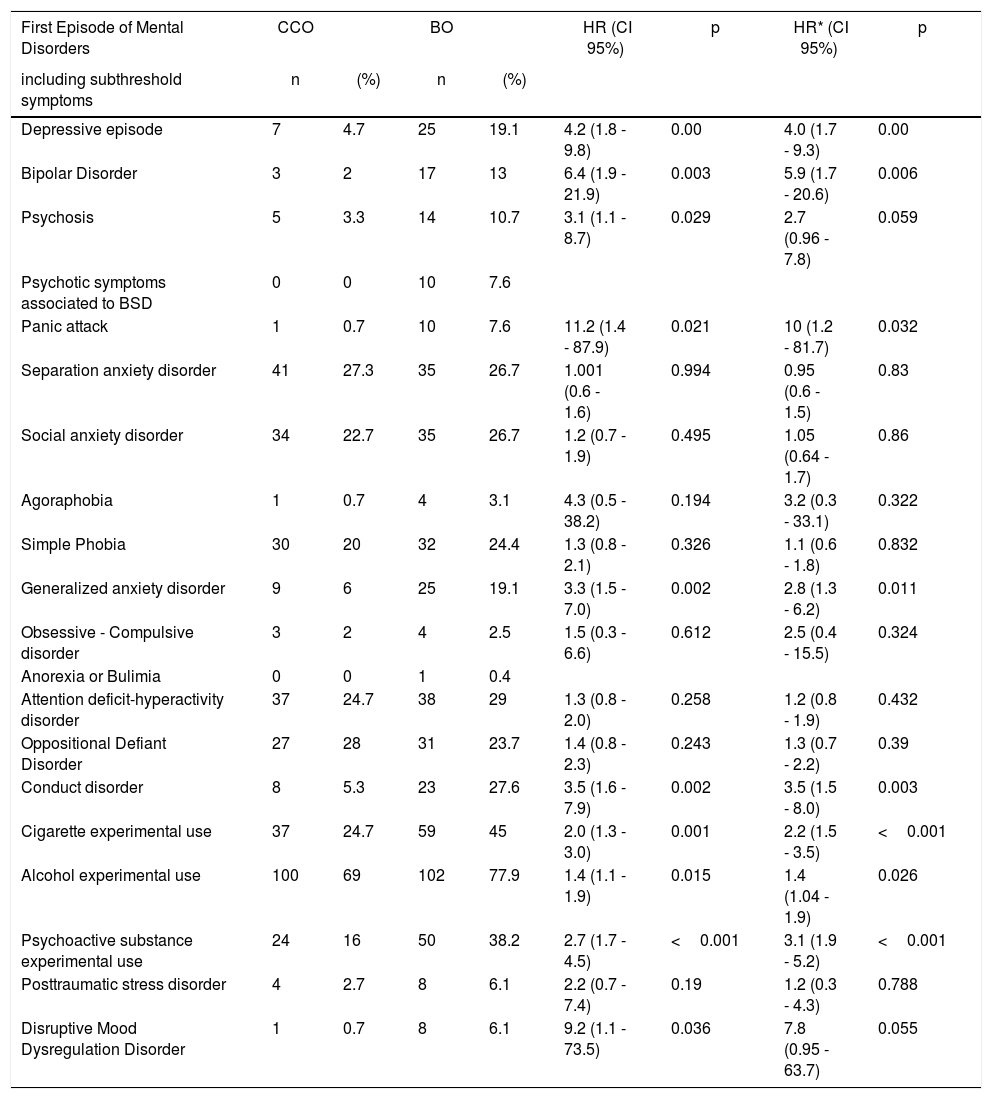
The BO group had a higher risk of subthreshold symptoms of affective disorders, psychosis, panic, GAD, CD and DMDD (see Table 6), although some of them lost statistical significance after adjusting for demographic variables, like subthreshold psychotic symptoms and DMDD.
Survival analysis, subthreshold symptoms onset.
| First Episode of Mental Disorders | CCO | BO | HR (CI 95%) | p | HR* (CI 95%) | p | ||
|---|---|---|---|---|---|---|---|---|
| including subthreshold symptoms | n | (%) | n | (%) | ||||
| Depressive episode | 7 | 4.7 | 25 | 19.1 | 4.2 (1.8 - 9.8) | 0.00 | 4.0 (1.7 - 9.3) | 0.00 |
| Bipolar Disorder | 3 | 2 | 17 | 13 | 6.4 (1.9 - 21.9) | 0.003 | 5.9 (1.7 - 20.6) | 0.006 |
| Psychosis | 5 | 3.3 | 14 | 10.7 | 3.1 (1.1 - 8.7) | 0.029 | 2.7 (0.96 - 7.8) | 0.059 |
| Psychotic symptoms associated to BSD | 0 | 0 | 10 | 7.6 | ||||
| Panic attack | 1 | 0.7 | 10 | 7.6 | 11.2 (1.4 - 87.9) | 0.021 | 10 (1.2 - 81.7) | 0.032 |
| Separation anxiety disorder | 41 | 27.3 | 35 | 26.7 | 1.001 (0.6 - 1.6) | 0.994 | 0.95 (0.6 - 1.5) | 0.83 |
| Social anxiety disorder | 34 | 22.7 | 35 | 26.7 | 1.2 (0.7 - 1.9) | 0.495 | 1.05 (0.64 - 1.7) | 0.86 |
| Agoraphobia | 1 | 0.7 | 4 | 3.1 | 4.3 (0.5 - 38.2) | 0.194 | 3.2 (0.3 - 33.1) | 0.322 |
| Simple Phobia | 30 | 20 | 32 | 24.4 | 1.3 (0.8 - 2.1) | 0.326 | 1.1 (0.6 - 1.8) | 0.832 |
| Generalized anxiety disorder | 9 | 6 | 25 | 19.1 | 3.3 (1.5 - 7.0) | 0.002 | 2.8 (1.3 - 6.2) | 0.011 |
| Obsessive - Compulsive disorder | 3 | 2 | 4 | 2.5 | 1.5 (0.3 - 6.6) | 0.612 | 2.5 (0.4 - 15.5) | 0.324 |
| Anorexia or Bulimia | 0 | 0 | 1 | 0.4 | ||||
| Attention deficit-hyperactivity disorder | 37 | 24.7 | 38 | 29 | 1.3 (0.8 - 2.0) | 0.258 | 1.2 (0.8 - 1.9) | 0.432 |
| Oppositional Defiant Disorder | 27 | 28 | 31 | 23.7 | 1.4 (0.8 - 2.3) | 0.243 | 1.3 (0.7 - 2.2) | 0.39 |
| Conduct disorder | 8 | 5.3 | 23 | 27.6 | 3.5 (1.6 - 7.9) | 0.002 | 3.5 (1.5 - 8.0) | 0.003 |
| Cigarette experimental use | 37 | 24.7 | 59 | 45 | 2.0 (1.3 - 3.0) | 0.001 | 2.2 (1.5 - 3.5) | <0.001 |
| Alcohol experimental use | 100 | 69 | 102 | 77.9 | 1.4 (1.1 - 1.9) | 0.015 | 1.4 (1.04 - 1.9) | 0.026 |
| Psychoactive substance experimental use | 24 | 16 | 50 | 38.2 | 2.7 (1.7 - 4.5) | <0.001 | 3.1 (1.9 - 5.2) | <0.001 |
| Posttraumatic stress disorder | 4 | 2.7 | 8 | 6.1 | 2.2 (0.7 - 7.4) | 0.19 | 1.2 (0.3 - 4.3) | 0.788 |
| Disruptive Mood Dysregulation Disorder | 1 | 0.7 | 8 | 6.1 | 9.2 (1.1 - 73.5) | 0.036 | 7.8 (0.95 - 63.7) | 0.055 |
CCO: community controls offspring, BO: bipolar offspring, n: number, %: percentage, HR: hazard ratio, CI95%: confidence interval 95%,*: adjusted by demographic variables (sex, age, socioeconomic status, schooling, housing area, traumatic events), BSD: Bipolar Spectrum Disorder
The BO group had a significantly a younger age of onset for tobacco use (14 vs 15 years, p 0.046), alcohol use (14 vs 15 years, p<0.001) and use of any PS (16 vs 18 years, p<0.001).
DiscussionThis longitudinal follow-up study found out that the BO compared to CCO had a higher risk of presenting depressive, bipolar, psychotic, substances use or externalizing disorders. During follow-up the BO group had a greater risk of presenting either new cases of psychiatric disorders or subthreshold disorders. The age of onset of psychiatric disorders, subthreshold disorder symptoms, and for PS consumption was younger in the BO group. Similarly, it was clearly observed that the high-risk group had a lower functionality compared to the control group.
The difference in BSD prevalence between the groups was clearly significant. Most of the cases of BSD in the BO group were BD unspecified type, which indicates that BD presentation starts with a non-specific affective symptomatology and progresses to a clearer manic episode. The mean age of onset for BSD is approximately 16 years, and that for the first manic episode was close to 20 years. This is consistent with the concept that considers, the BD unspecified as a clinical precursor for BD.12,44 A reasonable approach would be to evaluate early interventions in this high-risk population, especially in those that reach the mentioned age and also present an early manifestation of BD. Two reasonable proposals can arise from this information, the first is to carry out early evaluations in this children, specifically in those who reach the age of 15 years old and who present suggestive elements of the BSD in order to calculate the risk of BD development.45 The second, is to use screening measures such as the Parent version General Behavior Inventory in this population, in order to actively identify affective symptoms in these subjects at risk.46
This sample of parents with BD were recruited in a medical center for complex cases and also come from a high social vulnerability population. That could be a reason for this group to showed severe forms of BD, which in part could be reflected in the high prevalence of psychiatric disorders found in their offspring. Nevertheless, our findings are similar to other studies with parents with BD collected through advertisements 26or in mood disorders clinics.14,19,30,31
As mentioned above, three deaths were found in the BO group during the follow-up. One subject who committed suicide, had BD and was already in treatment during the time 1 assessment. Another subject, who had only social phobia in the first assessment (time 1), and who during the evolution presented an episode of MDD, followed by several suicide attempts, and the final outcome of suicide. One subject who presented ODD and CD at time 1, and who during the evolution presented mania induced by PS consumption, who died two weeks after his first psychiatric hospitalization by homicide. Although it is beyond the study objective, these deaths were described here, because they correspond to a serious consequence of mental disorder in the risk group. In other similarly at-risk populations, it has been documented that suicidal ideation prevalence is higher than controls, and that the presence of mood disorders, hostility, sexual abuse and family discord are strongly associated with the emergence of suicidal ideation.47
As a secondary finding, it was found that compared to the CCO group, the BO group have twice the risk of being exposed to the traumatic events listed in the K-SADS-PL: PTSD section. Other studies have found a risk up to three times higher for offspring of parents with BD, when exposed to any stressful event48; these events predispose to the onset of mood disorders in this high-risk population.49 Although we evaluated the influence of this stressful events on the age of onset of symptoms over time, and we did not observed differences when demographic variables are included in the adjusted analysis. Our findings suggest that traumatic events should be consider, however they are not a component that determines which psychopathology presents the BO group.
Our follow-up study showed that the BO group had more cases of mood disorders, subthreshold psychotic symptoms and SUD, which otherwise suggests a complex relationship among these mental disorders. Affective symptoms could be associated with PS use, and at the same time early substance use could be associated with the onset of affective and psychotic symptoms. As other authors, we propose that primary prevention of PS consumption is a fundamental part of the early strategy in this high-risk population, in conjunction with psychotherapy, family therapy, self-help programs.17,32,50,51
The subjects with new diagnosis of BSD had previous diagnosis at time 1 such as: subthreshold depressive symptoms, ADHD, ODD, and CD, and consumption of PS. Our data is according to other authors’ conceptualization on premorbid trajectories, highlighting anxiety disorders, mood disorders and substance use as a marker of the BD onset.15
Our analysis included subthreshold symptoms and the age of onset for different psychiatric disorders. This follow-up study showed that BO group presented an increased risk of subthreshold symptoms, mainly: depressive, bipolar and psychotic, which all seem to be precursors of the BD episodes. In addition, there is a greater risk for PS consumption and also at a younger age, which is a well-recognized trigger agent of BD episodes. All this information raises the question: what is the role of an early treatment in subthreshold symptoms or an experimental consumption of PS, in the prognosis of this population?
Similar to other studies around the world, this study gathers evidence that bipolar spectrum symptoms indicate an increased risk of BD conversion.12,15,27,32,50–59 Contrary to other reports, our findings do not indicate a significant presence of anxiety disorders associated with the BD prodrome. However, it should be mentioned that in this follow-up there was a significant difference in the incidence of SAD, social anxiety and phobias in the risk group, which could indicate a certain tendency for BD development.
LimitationsThis proband sample collection in a specialized center, could represent a selection bias of the risk cases. Besides that, the percentage of losses was greater than expected, in this way a limited sample size made our findings less accurate, which could have affected our results. On the other hand, we excluded subjects over 30 years-old who could provide information on psychopathology during middle adulthood. Finally, the possible influence of the treatment of some psychiatric disorders during follow-up was not accounted.
It should be considered that the losses during this follow-up study may influence our results. In the first place, half of the losses were due to exceeded the age limit of 30 years, but this was proportional for each group. Second, there is a trend that indicates that parents with greater psychopathology tend to report more symptoms in their children 60and participate more in this kind of studies. In this sense, subjects who did not continue the follow-up could be part of the healthiest fraction of the risk cohort, and thus made have increased the differences found.
A strength of this study was our analysis of the age of onset for the psychiatric disorders, as well as the assessment of subthreshold symptoms which showed a similar tendency to the “full-syndrome” psychiatric disorders. Therefore, for future studies, we propose to determine the onset subthreshold symptoms to evaluated the risk of presenting BD during the follow-up.
This study was conducted in a genetically isolated population, and this implies the possibility of finding cases of great morbidity and less genetic variability. Although this is relevant for future genetic studies, the data obtained from a genetically isolated population should be taken with caution, since it is not entirely extrapolated to other populations.
ConclusionWe found out that the BO group compared with the CCO group in the genetic isolate “paisa” have higher frequency of affective, psychotic, externalizing and substances use disorders, and also a lower functionality. The magnitude of the difference in the prevalence of psychiatric disorders tends to increase in our four years follow-up, and it is not influenced by demographic variables. It is worthy to study subthreshold symptoms and their stability over time. For their part, mental health professionals must recognize the risks of the BO group in order to make an early identification of disorders, timely treatment and prevent the outcomes of an untreated BD.
Authors’ participationAuthor JDPO designed the study and wrote the protocol. Authors JJEO, CPQC, SEJ, RAC, SGC and JV conducted psychiatric interviews with participants. Authors PADR, CALJ and JDPO performed the best estimate procedure. Author DCAA conducted statistical analyses. Authors JJEO, JGV and JPDO contributed to the data analysis and wrote the manuscript. All authors contributed to and have approved the final manuscript.
FundingThis work was supported by COLCIENCIAS grant 1115 7114 9700, el Proyecto PRISMA Colciencias grant 99059634, la facultad de Medicina de la Universidad de Antioquia, and the Comité para el Desarrollo de la Investigación de la Universidad de Antioquia (CODI),
Conflict of interestsThe authors have no conflicts of interest to disclose.
The work was supported in part by COLCIENCIAS grant 1115 7114 9700 (P.I. Juan D. Palacio), Proyecto PRISMA Colciencias grant 99059634 (P.I. Carlos Lopez) and Faculty of Medicine from the Universidad de Antioquia. We thank the families who participated in this research. We thank Maria Cecilia Lopez, Aurora Gallo and all members of de Grupo de Investigación en Psiquiatría (GIPSI) for their help and support contacting participating families. We also thank the Committee for the Development of Research of the U. of A., CODI, and the Sustainability Strategy of the Universidad de Antioquia. Vice-Rector's Office of Research.
This article was written and approved by all its authors and it has not been published in another journal or scientific publication.