The current SARS-CoV-2 pandemic has caused feelings of anxiety, confusion, and panic among the world population. Due to these psychological changes resulting from the stress produced by the disease, we sought to investigate the psychological impact of the pandemic on the university student community.
Material and methods1,283 students were surveyed, of which 1,149 students were selected. The majority of the subjects were female, and the overall average age was of 20 years. They were provided with an 82-question online questionnaire divided into four sections; looking for the prevalence of significant symptomatology of major depression and generalised anxiety using the PHQ-9 and GAD-7 scales; and factors that potentially affect the mental health of our university population.
ResultsWe found a high prevalence of significant depression (47.08%) and anxiety (27.06%) symptomatology, considering a score of 10 or more as cut-off point. There was no significant difference in depression and anxiety symptomatology between the health-care students and non-health-care students.
ConclusionsOur results, together with what is observed in the literature, allow us to conclude that the college student population has a high risk of mental illness, and these should be taken into consideration for the search of effective strategies for detection and control of mental health illnesses. Undoubtedly, the COVID-19 pandemic is a red flag that shows the need to upgrade mental health programmes in universities and to validate virtual instruments.
La actual pandemia de SARS-CoV-2ha causado sentimientos de ansiedad, confusión y pánico entre la población mundial. Debido a estos cambios psicológicos derivados del estrés que produce la enfermedad, se buscó investigar el impacto psicológico de la pandemia en la comunidad estudiantil universitaria.
Material y métodosSe encuestó a 1.283 estudiantes, de los que se seleccionó a 1.149. La mayoría eran mujeres y la media de edad fue 20 años. Se les proporcionó un cuestionario en línea de 82 preguntas divididas en 4 secciones para indagar la prevalencia de síntomas significativos de depresión mayor y ansiedad generalizada utilizando las escalas PHQ-9 y GAD-7, además factores que pueden afectar a la salud mental de nuestra población universitaria.
ResultadosSe halló una alta prevalencia de síntomas significativos de depresión (47,08%) y ansiedad (27,06%), considerando como umbral un total de 10 o más puntos. No hubo diferencias significativas entre los estudiantes relacionados con la salud y los no relacionados con la salud.
ConclusionesNuestros resultados, en conjunto con lo observado en la literatura, muestran que la comunidad universitaria es una población en riesgo de enfermedades mentales, por lo que el Gobierno debería considerar la creación de estrategias efectivas para la detección de problemas de salud mental; sin duda alguna, la actual pandemia de COVID-19 es un foco rojo sobre las necesidad de mejores programas de salud mental en universidades y validación de instrumentos virtuales.
On December 31, 2019, in China an alert on atypical pneumonia of viral origin unknown to date was emitted.1 On January 9, the causal agent, later called severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), belonging to the coronavirus family (Coronaviridae), was described as an RNA virus that have a high pandemic potential with the capacity to produce an important acute respiratory syndrome, classified as coronavirus disease of 2019 (COVID-19). In March 11, the World Health Organization (WHO) declared COVID-19 as a global pandemic. On February 28 the first case was confirmed in our country, on March 11 it was confirmed the first case in the state of the authors, and on March 15 an on-site and online classes suspension was emitted in the whole campus of the authors university.2–4 For today, Mexico is the #11 country in total cases and #3 in deaths, being one of the most affected ones.5
Some authors like Steven Taylor have described the most common reactions that can be found with the thought of loss, damage, and change that has been seen with other pandemics. He described that for the next great pandemic (the one we are currently experiencing) the reactions would be diverse, emotionally people react with fear, indifference and others as far as fatality. He also described that in those people that have been diagnosed with a mental health disorder there can be an exacerbation of symptoms. Other causes that can increase anxiety, stress or anger are the loss of a loved one due to illness and the measures the government stablishes to mitigate the effects of the pandemic such as confinement, social distancing, and the use of face mask, these measures are currently performed in our country.6
Chandratre7 shows in his study that the student population, specifically medical students, shows mental and emotional affections, as observed in 25% of the students from Changzhi University as well as 27% of the students from Sichuan University, both in China, who presented important psychological affection.8,9 A Pakistani University reported a frequency of 34% and 45% for moderate-severe anxiety and depression respectively.10 On a Spanish university, it was reported 21.34% and 34.19% of moderate-severe anxiety and depression.11 A Mexican study reported 31.92% prevalence of stress symptoms and just 4.9% prevalence of depression symptoms moderate-severe.12 These studies suggest that the pandemic may be a trigger for the worsening of the preexisting mental health conditions within the students, as well as burnout syndrome and substance abuse, because they are a vulnerable population due to their high rates of depression, suicidal thoughts and stigmatizing, as well as being the least likely to seek psychological help.7
At the same time, O’Byrne et al. mentioned that another triggering factor for increased student anxiety is that, as the cases increase, many colleges are in need of recent graduate students in an accelerated manner, putting them in a vulnerable situation to unnecessary risks to them, to patients and other professionals, because they do not have an appropriate preparation; this can turn them into vectors for the disease, use of extra personal protective equipment, exposing them to moral trauma, leading to a worsening of their mental health.13
Meo et al.14 showed how the pandemic has caused at least to a quarter of medical students an increase in stress and discouragement, in addition to a feeling of emotional unattachment from their family and friends, causing a low work performance and affecting their study time, so the prolongation of quarantine can increase the psychological and learning disorders of medical students, as well as an increase in mental health problems. Ferrell et al.15 have theorized the significant impact that medical students will have on students from other degrees, due to the cancellation of clinical practice due to the need of protection of the student population and the flattening of the contagion curve, the cancellation of conferences of experts and classes. In addition, the students who cannot adapt to webinar lectures and online classes will be the most affected (considering the economic implications in developing countries where not all the population have internet access).
Medina et al.16 reported in 2005 with a general population national survey that university students have equal or more probability to suffer a psychological disorder; the general risk factors of this population includes being young, transition from adolescence to adulthood, the rising rates of suicide deaths among young population in the country of the authors, social conditionals such as educational attainment, workforce entrance, participation and productivity, interpersonal relations; as cited and described by Benjet et al.17 at least in first year students. In a systematic review carried out by January et al.18, it would be settled down the prevalence of anxiety and depression among low-middle income countries, meanwhile; they found a prevalence above 35% for each disorder.
All these emotional reactions can lead the population to search for alternative treatments to prevent the disease and help their families, the search for drugs that has not proven effectiveness, as steroids, can damage the health of those who try it. The rumors, which are circulated by the people and the media are also common during the pandemic scenario, these include conspiracy theories, believing that some ritual would prevent their infection, or that they can get infected if they have contact with certain substances as reported by Khan et al.19
It is important to know the role that the current pandemic situation has in the mental health of the college students and the influence of family and friends. The aim of this study is to know how much college students from the authors university know about the COVID-19, the current prevalence of significative symptomatology of major depression and generalized anxiety and if there is a significative difference between health-care-related and non-health-related students. Also, to look for protective or triggering social factors, therefore it is expected to compare data on anxiety and depression prevalence prior to the pandemic in the college students population in the country of the authors, college population is considered vulnerable to presenting psychological disorder because they are young adults, in constant search to prevail, learn and compete with peers to earn their place in a highly competitive field and finally because they are losing professional practices due the global pandemic. In one of the most affected countries, it is expected to find an increased prevalence of anxiety and depression that can be related to their social circumstances, their ideas about the pandemic and the frustration of losing personal projects.
MethodsStudy design and participantsThis work is a cross-sectional study, and consists of data recollection in a single moment and time. Its purpose is to describe variables and analyze their incidence and interaction at a given moment, and an online survey was carried away. The studied sample were students of any semester of any career in a single university. In this university there are almost 85 000 ungraduated college students. The inclusion criteria were to be students at this public university and be studying in first to twelfth semester. The exclusion criteria were to be students of any career who were studying their year of Social Service or who belong to the university high-school or postgraduate system, and finally, students who do not complete the survey. The sample size was determined using the STATS® (2020)20 program through randomized numbers. The minimum sample size obtained was 661-students with confidence level of 95.5%, error margin of 5% and population heterogeneity of 50%.
MeasurementsOnline questionnaireA questionnaire was elaborated with 82 questions divided into four factors:
- 1.
COVID-19 knowledge and perception and social determinants.
- 2.
Subjective mental state.
- 3.
Emotional state depression (symptoms).
- 4.
Emotional state anxiety (symptoms).
This scale was used to screen subjects for generalized anxiety disorder, which includes 7 questions that are based on symptoms presence and severity and the need for treatment. The responses are Likert type (any day, some days, more than a half of the days, almost every day) with a 0, 1, 2, 3 scoring per question.21 The cutoff point is ≥10 points for significative anxiety symptoms (moderate-severe) and expose the need for active treatment. The scale has a sensibility and specificity of 89%, internal consistency (Cronbach α=.92) and test-retest reliability (interclass correlation, 0.83).22 GAD-7 is a screening, not a diagnostic test.
PHQ-9This scale was used to screen subjects for the major depressive disorder, used to determine the symptoms presence, severity and the need for treatment. It has 9 questions that are based on the presence of symptoms; the responses are Likert type (any day, some days, more than a half of the days, almost every day) with a 0-3 scoring range. A score ≥10 is a cutoff point to be considered a significative presence of symptoms (moderate-severe) and expose the need for active treatment.23 It has a sensitivity and specificity of 88%, internal consistency (Cronbach α, .86-.89) and test-retest reliability (interclass correlation, 0.84).24 PHQ-9 is a screening, not a diagnostic test.
ProcedureFirst, it was performed a literature search about socio-psychological changes that are expected during the pandemic, then, permission was requested from the corresponding academic authorities of the university (ethical and research commitments, permission P120-00238), where they ask to the need of online informed consent and permission to share date, at the same time they suggested the option to ask for electronic email in case the students had any doubt, for students with suicidal ideation, they suggesting contacting them. After this, it was decided to start the placement of questions and their dissemination through Microsoft Office Teams platform. 1500 students were randomly chosen through the same platform, and the link was sent to answer the survey. Finally, students were invited to participate voluntarily, signing the corresponding virtual informed consent. Respondents received no economic, material, or academic compensation for participating in this study.
Statistical analysisThe studied sample was divided into 2 groups to address anxiety and depression, mild and significative symptoms (instead of using the classic grades of none, mild, moderate, moderate-severe, and severe), using a score of 10 as cut point. Continuous variables were represented by mean±standard deviation and median [interquartile range], and the categorical variables were presented as percentages. To identify the variable distribution type, they were analyzed using the Kolmogorov-Smirnov test. The differences between the non-parametric quantitative variables were evaluated with the Mann-Whitney U statistical test and the qualitative variables were evaluated using with the χ2 test or Fisher's exact test. Spearman's correlation was used to evaluate the correlation between variables and a significative staging of depression and anxiety. A binary logistic regression was done to identify the association between the variables and the significative staging of depression and anxiety using the variables that previously had a correlation with a P-value <.01. Statistical analysis was conducted in IBM-Statistical Package for Social Sciences version 23 (IBM Corp., USA)25, and the figure was produced using R version 4.0.2 (R Core Team, Austria)26 with the package ggplot2 version 3.3.2 (Wickham, USA).27
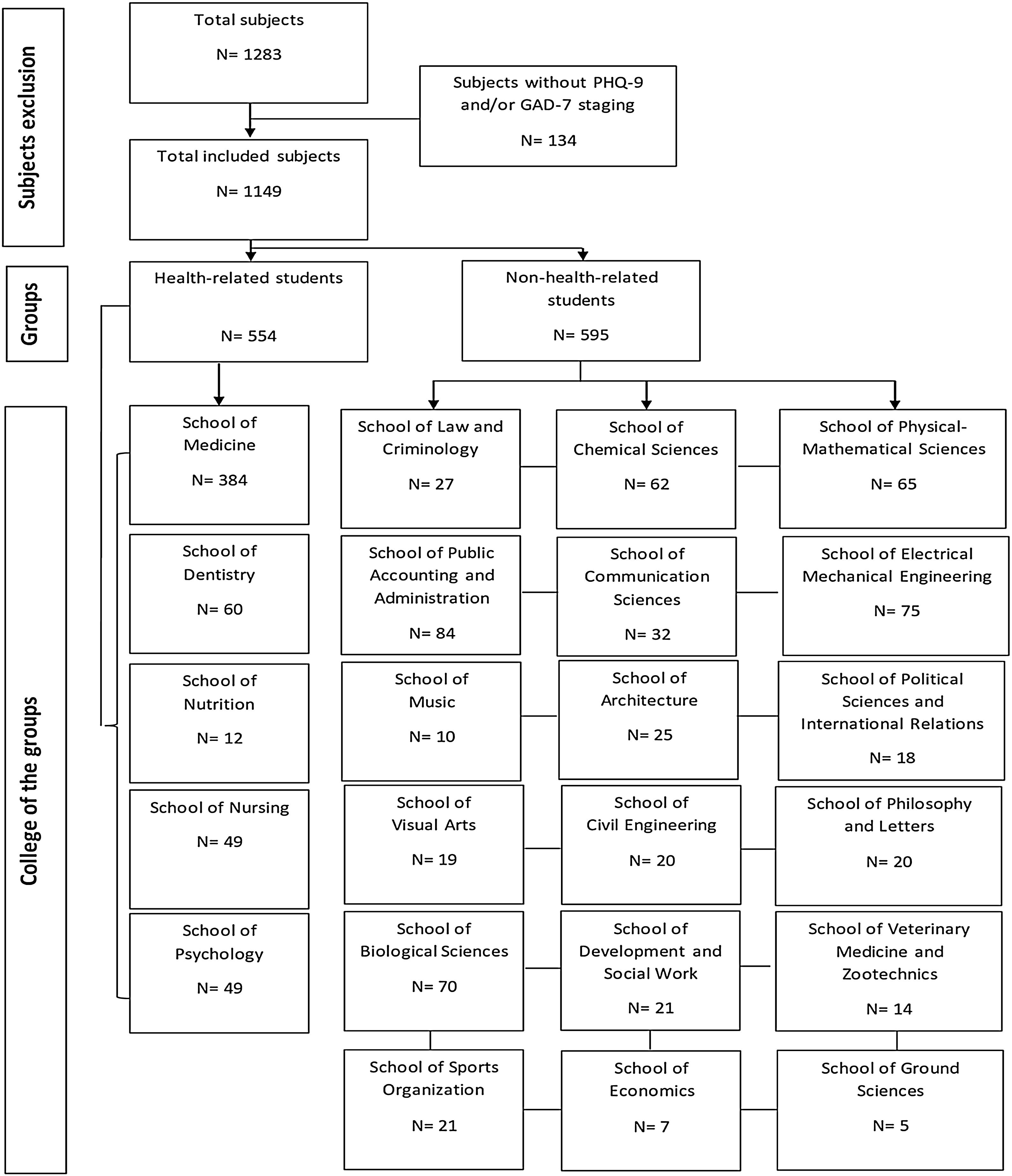
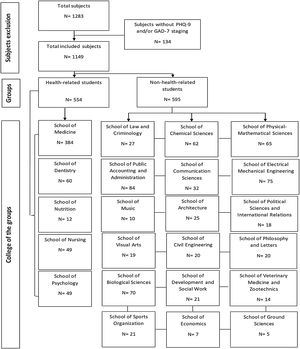
ResultsThe total of online questionnaires answered were 1283 (85.53% of the 1500 randomly chosen students); 134 students did not complete the survey, and they were excluded, leaving a final 1149 (89.55%) student sample. The average age was 20 years old and 745 were women (64.8%); 554 (48.2%) belong to health-area (figure 1).
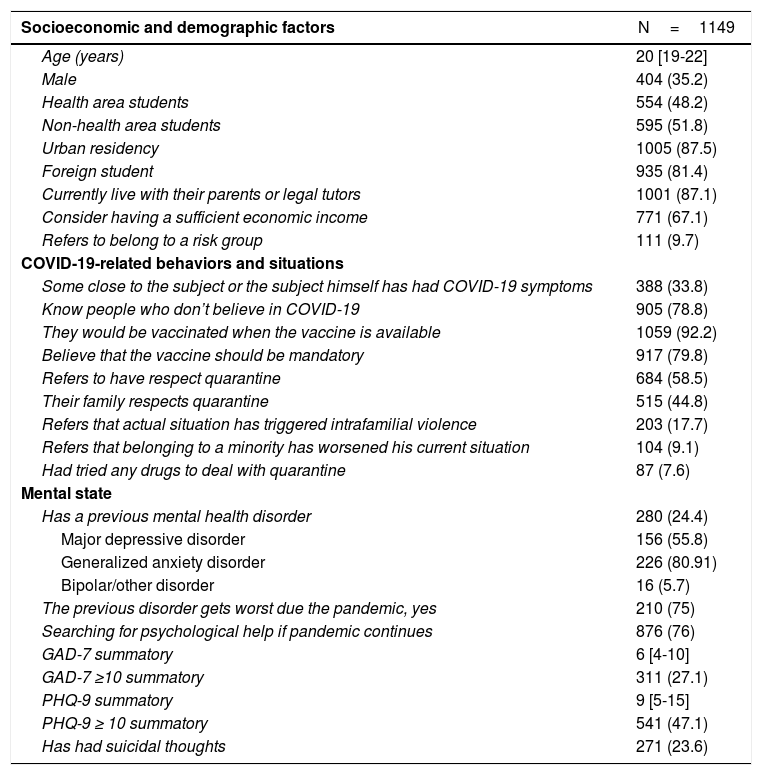
COVID-19 knowledge and perception and social determinantsThe results show that the majority of the students in the university, 1059 (92.2%), would get vaccine as soon as available, also a high percentage (79.8%) believes that the vaccinate should be mandatory for all people. 684 (58.5%) of the students referred that they had respected the quarantine and 515 (44.8%) referred that their family had respected it; 388 referred that close friends or family have had COVID-19 symptoms (33.8%), the 17.7% referred that the quarantine had triggered intrafamilial violence; 9.1% states that they are part of a minority and in the same time this make worst their situation during the pandemic; 7.6% state that they had tried drugs in the lapse of this quarantine to deal with it (being marijuana the most common), 88% believes that more diffusion about psychological health is necessary from the authorities (Table 1).
Characteristics of the population.
| Socioeconomic and demographic factors | N=1149 |
|---|---|
| Age (years) | 20 [19-22] |
| Male | 404 (35.2) |
| Health area students | 554 (48.2) |
| Non-health area students | 595 (51.8) |
| Urban residency | 1005 (87.5) |
| Foreign student | 935 (81.4) |
| Currently live with their parents or legal tutors | 1001 (87.1) |
| Consider having a sufficient economic income | 771 (67.1) |
| Refers to belong to a risk group | 111 (9.7) |
| COVID-19-related behaviors and situations | |
| Some close to the subject or the subject himself has had COVID-19 symptoms | 388 (33.8) |
| Know people who don’t believe in COVID-19 | 905 (78.8) |
| They would be vaccinated when the vaccine is available | 1059 (92.2) |
| Believe that the vaccine should be mandatory | 917 (79.8) |
| Refers to have respect quarantine | 684 (58.5) |
| Their family respects quarantine | 515 (44.8) |
| Refers that actual situation has triggered intrafamilial violence | 203 (17.7) |
| Refers that belonging to a minority has worsened his current situation | 104 (9.1) |
| Had tried any drugs to deal with quarantine | 87 (7.6) |
| Mental state | |
| Has a previous mental health disorder | 280 (24.4) |
| Major depressive disorder | 156 (55.8) |
| Generalized anxiety disorder | 226 (80.91) |
| Bipolar/other disorder | 16 (5.7) |
| The previous disorder gets worst due the pandemic, yes | 210 (75) |
| Searching for psychological help if pandemic continues | 876 (76) |
| GAD-7 summatory | 6 [4-10] |
| GAD-7 ≥10 summatory | 311 (27.1) |
| PHQ-9 summatory | 9 [5-15] |
| PHQ-9 ≥ 10 summatory | 541 (47.1) |
| Has had suicidal thoughts | 271 (23.6) |
Data shown as n (%) or median [interquartile range].
69.62% reported a moderate to exaggerated increase in anxiety state prior to the start of the pandemic, 280 students (24.4%) reported to have a previous mental health disorder (156 had major depressive disorder, 226 had generalized anxiety disorder, and 16 had bipolar disorder or other), only 70 (25%) reported not having a deterioration of their symptoms. 876 (76.3%) mentioned that if the pandemic continues and their symptoms continue, they would seek psychological professional help. 271 (23.6%) reported to have suicidal thoughts at least once a week (Table 1).
Depression symptomsA total of 245 (44.22%) health-related students and 296 (49.74%) non-health-related students presented a significative classification for depression symptomatology, without finding a statistically significant difference between them (P=.061), although there was a higher and significant prevalence of suicidal thoughts (39.86% vs 38.36%) in the non-health-related student group with (P=<.001). From the comparison between health-related vs. non-health-related students with significative symptomatology of depression classification, there was find a significative difference in the search for information about COVID-19: 90.61% of the health-related students did it. Among other significative differences found between these groups, it was found that the health-related students had more relatives who do not believe in the disease caused by SARS-CoV-2, believe that vaccination must be mandatory, know a medical health provider that had been discriminated, considered quarantine necessary, more reported living with their parents, also felt more that belonging to a minority group makes them vulnerable during crisis time, and would like to receive help for their symptomatology. There was no significative difference in the use of drugs to deal with the quarantine (Table 2).
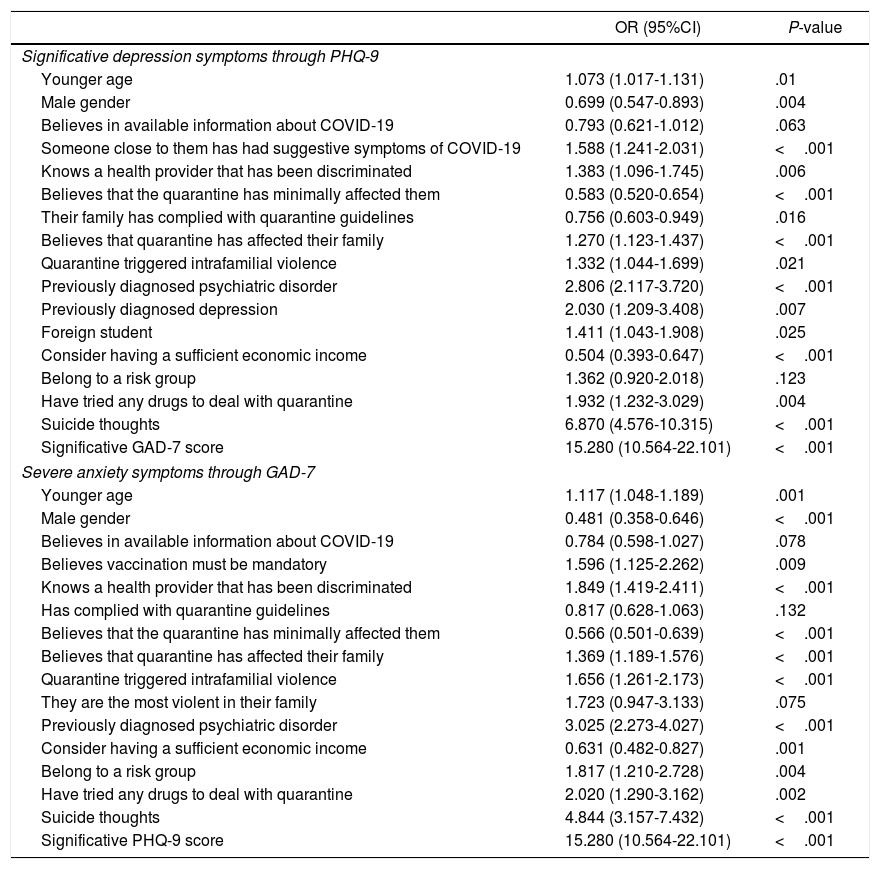
Odds ratio of variables as predictors of severe depression and/or anxiety staging in all college students.
| OR (95%CI) | P-value | |
|---|---|---|
| Significative depression symptoms through PHQ-9 | ||
| Younger age | 1.073 (1.017-1.131) | .01 |
| Male gender | 0.699 (0.547-0.893) | .004 |
| Believes in available information about COVID-19 | 0.793 (0.621-1.012) | .063 |
| Someone close to them has had suggestive symptoms of COVID-19 | 1.588 (1.241-2.031) | <.001 |
| Knows a health provider that has been discriminated | 1.383 (1.096-1.745) | .006 |
| Believes that the quarantine has minimally affected them | 0.583 (0.520-0.654) | <.001 |
| Their family has complied with quarantine guidelines | 0.756 (0.603-0.949) | .016 |
| Believes that quarantine has affected their family | 1.270 (1.123-1.437) | <.001 |
| Quarantine triggered intrafamilial violence | 1.332 (1.044-1.699) | .021 |
| Previously diagnosed psychiatric disorder | 2.806 (2.117-3.720) | <.001 |
| Previously diagnosed depression | 2.030 (1.209-3.408) | .007 |
| Foreign student | 1.411 (1.043-1.908) | .025 |
| Consider having a sufficient economic income | 0.504 (0.393-0.647) | <.001 |
| Belong to a risk group | 1.362 (0.920-2.018) | .123 |
| Have tried any drugs to deal with quarantine | 1.932 (1.232-3.029) | .004 |
| Suicide thoughts | 6.870 (4.576-10.315) | <.001 |
| Significative GAD-7 score | 15.280 (10.564-22.101) | <.001 |
| Severe anxiety symptoms through GAD-7 | ||
| Younger age | 1.117 (1.048-1.189) | .001 |
| Male gender | 0.481 (0.358-0.646) | <.001 |
| Believes in available information about COVID-19 | 0.784 (0.598-1.027) | .078 |
| Believes vaccination must be mandatory | 1.596 (1.125-2.262) | .009 |
| Knows a health provider that has been discriminated | 1.849 (1.419-2.411) | <.001 |
| Has complied with quarantine guidelines | 0.817 (0.628-1.063) | .132 |
| Believes that the quarantine has minimally affected them | 0.566 (0.501-0.639) | <.001 |
| Believes that quarantine has affected their family | 1.369 (1.189-1.576) | <.001 |
| Quarantine triggered intrafamilial violence | 1.656 (1.261-2.173) | <.001 |
| They are the most violent in their family | 1.723 (0.947-3.133) | .075 |
| Previously diagnosed psychiatric disorder | 3.025 (2.273-4.027) | <.001 |
| Consider having a sufficient economic income | 0.631 (0.482-0.827) | .001 |
| Belong to a risk group | 1.817 (1.210-2.728) | .004 |
| Have tried any drugs to deal with quarantine | 2.020 (1.290-3.162) | .002 |
| Suicide thoughts | 4.844 (3.157-7.432) | <.001 |
| Significative PHQ-9 score | 15.280 (10.564-22.101) | <.001 |
GAD-7: General Anxiety Disorder-7; PHQ-9: Patient Health Questionnarie-9.
A logistic binary regression has been performed to assess variables that have a correlation with a P-value <.1. An odds ratio that won’t cross the 1 and a P-value <.05 has interpreted like significative.
It was also reported that non-health-related students had seek for alternative medicine more often, their families also complied more with the quarantine guidelines, considered that quarantine had affected them more, reported more domestic violence, more worsening of the previous mental health disorders and increase in suicidal thoughts.
Many of the risk or protective factors for present or not a significative symptomatology of depression was shared between both groups (Table 2). Among the not shared factors, health-related students; knowing that someone close to them had symptoms suggestive of COVID-19, believing that vaccination should be mandatory, and have used drugs were risk factors for this group in particular. On the other hand, the fact that their family complied with the health recommendations and that their siblings were the most violent in their family circle were protective factors for this group. Likewise, among the non-health-related students; believing that the quarantine had affected their family, that the quarantine had caused domestic violence, and that their previously diagnosed mental health disorder get worst were risk factors for this group. For the overall students, being a foreign student and knowing a health provider that was discriminated were risk factors (Table 1 of the supplementary material).
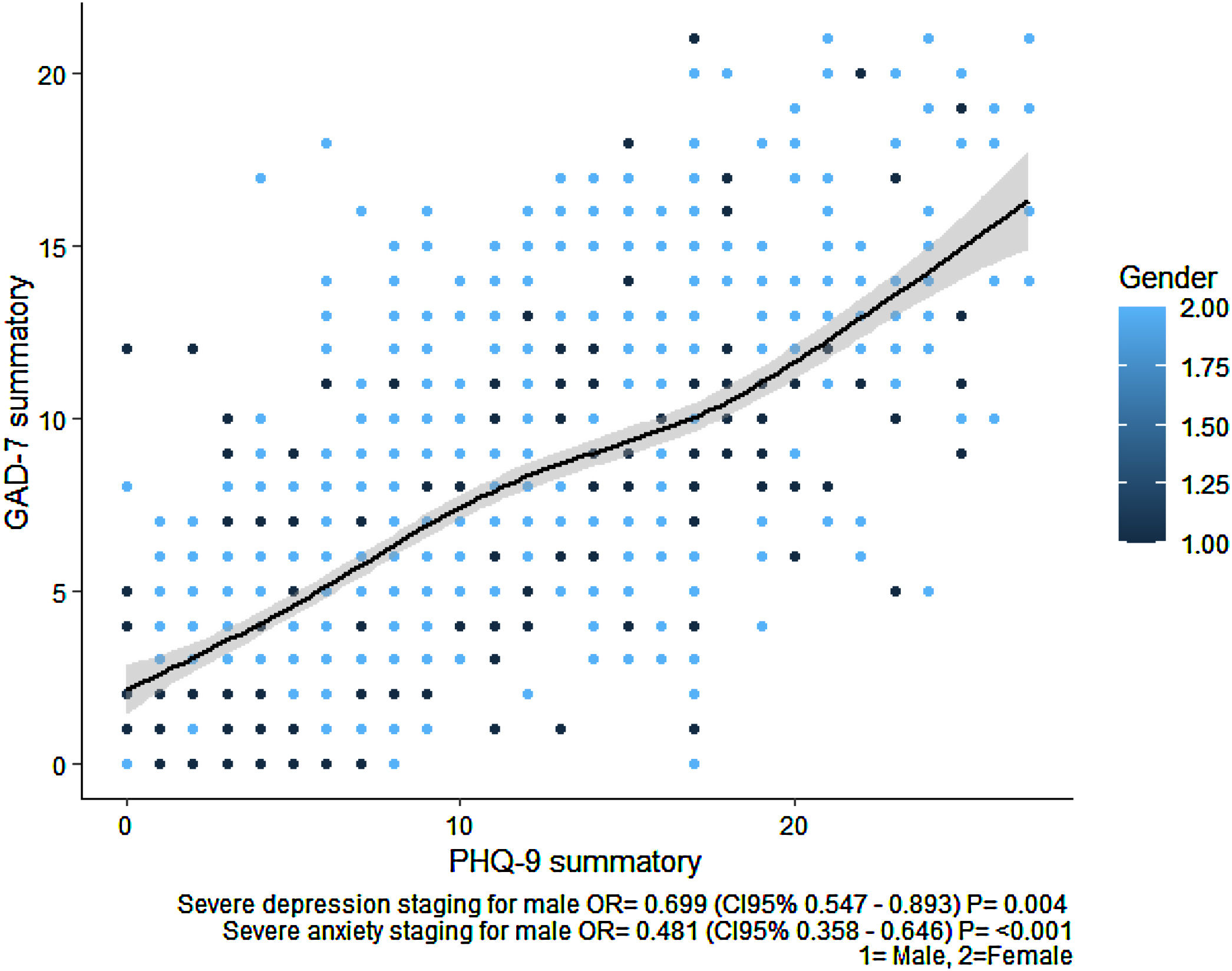
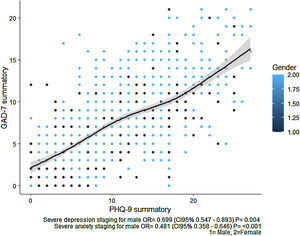
Anxiety symptomsA total of 311 students (27.07%) of the sample were classified in the significative group of generalized anxiety disorder symptoms using the GAD-7 scale. 141 (25.45%) health-related students and 170 (28.57%) non-health-related students presented a significative stage for anxiety symptoms, without finding a statistically significant difference between them (P=.234), although there is a significant difference in the prevalence of suicidal thoughts (43.26% vs. 47.05% in health-related and non-health-related groups respectively; P=<.001). It seems that the female subjects belonging either the health or non-health related careers had more prevalence on significative anxiety symptoms (figure 2).
Anxiety and depression staging summatory in male and female genders. It can be seen that the sum of one of the scales is proportional to the sum of the other. Likewise, it can be seen that most of the subjects of the male gender are within a smaller sum of both scales. GAD-7 is the staging scale for anxiety. PHQ-9 is the staging scale for depression. Gender no. 1 represents a male subject, and gender no. 2 represents a female subject.
The health-related students had better awareness about the pandemic than the non-health related students and had sought fewer alternative therapies against the disease. It was observed that the health-related students knew more medical health providers that had been discriminated and agree that the quarantine was necessary than the non-related health students. It was also seen that the quarantine affected both sides in a similar way. Triggering factors, including aggravation of previous mental health disorders, increasing of illegal substances (marijuana and others) and suicidal thoughts were remarkable present in the group of non-health-related students and it correlates that there were less percentages of this group that lived with their parents, also it was seen that a higher number of this group identify themselves as a minority group (Table 3 and Table 4).
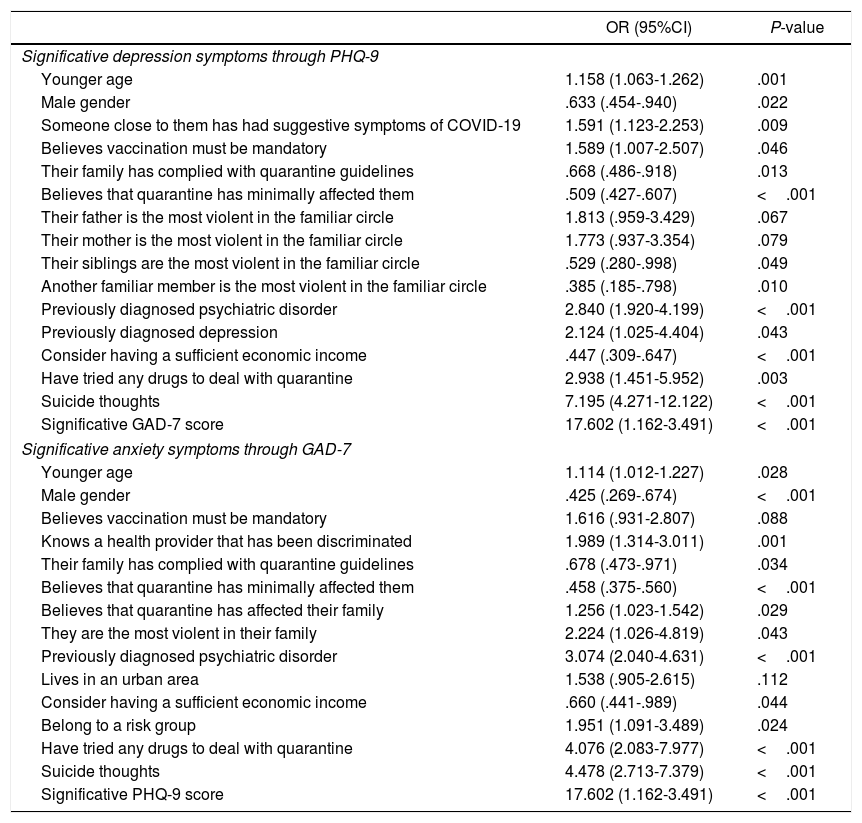
Odds ratio of variables as predictors of severe depression and/or anxiety staging in health-related college students.
| OR (95%CI) | P-value | |
|---|---|---|
| Significative depression symptoms through PHQ-9 | ||
| Younger age | 1.158 (1.063-1.262) | .001 |
| Male gender | .633 (.454-.940) | .022 |
| Someone close to them has had suggestive symptoms of COVID-19 | 1.591 (1.123-2.253) | .009 |
| Believes vaccination must be mandatory | 1.589 (1.007-2.507) | .046 |
| Their family has complied with quarantine guidelines | .668 (.486-.918) | .013 |
| Believes that quarantine has minimally affected them | .509 (.427-.607) | <.001 |
| Their father is the most violent in the familiar circle | 1.813 (.959-3.429) | .067 |
| Their mother is the most violent in the familiar circle | 1.773 (.937-3.354) | .079 |
| Their siblings are the most violent in the familiar circle | .529 (.280-.998) | .049 |
| Another familiar member is the most violent in the familiar circle | .385 (.185-.798) | .010 |
| Previously diagnosed psychiatric disorder | 2.840 (1.920-4.199) | <.001 |
| Previously diagnosed depression | 2.124 (1.025-4.404) | .043 |
| Consider having a sufficient economic income | .447 (.309-.647) | <.001 |
| Have tried any drugs to deal with quarantine | 2.938 (1.451-5.952) | .003 |
| Suicide thoughts | 7.195 (4.271-12.122) | <.001 |
| Significative GAD-7 score | 17.602 (1.162-3.491) | <.001 |
| Significative anxiety symptoms through GAD-7 | ||
| Younger age | 1.114 (1.012-1.227) | .028 |
| Male gender | .425 (.269-.674) | <.001 |
| Believes vaccination must be mandatory | 1.616 (.931-2.807) | .088 |
| Knows a health provider that has been discriminated | 1.989 (1.314-3.011) | .001 |
| Their family has complied with quarantine guidelines | .678 (.473-.971) | .034 |
| Believes that quarantine has minimally affected them | .458 (.375-.560) | <.001 |
| Believes that quarantine has affected their family | 1.256 (1.023-1.542) | .029 |
| They are the most violent in their family | 2.224 (1.026-4.819) | .043 |
| Previously diagnosed psychiatric disorder | 3.074 (2.040-4.631) | <.001 |
| Lives in an urban area | 1.538 (.905-2.615) | .112 |
| Consider having a sufficient economic income | .660 (.441-.989) | .044 |
| Belong to a risk group | 1.951 (1.091-3.489) | .024 |
| Have tried any drugs to deal with quarantine | 4.076 (2.083-7.977) | <.001 |
| Suicide thoughts | 4.478 (2.713-7.379) | <.001 |
| Significative PHQ-9 score | 17.602 (1.162-3.491) | <.001 |
GAD-7: General Anxiety Disorder-7; PHQ-9: Patient Health Questionnarie-9.
A logistic binary regression has been performed to assess variables that have a correlation with a P-value <.1. An odds ratio that won’t cross the 1 and a P-value <.05 has interpreted like significative.
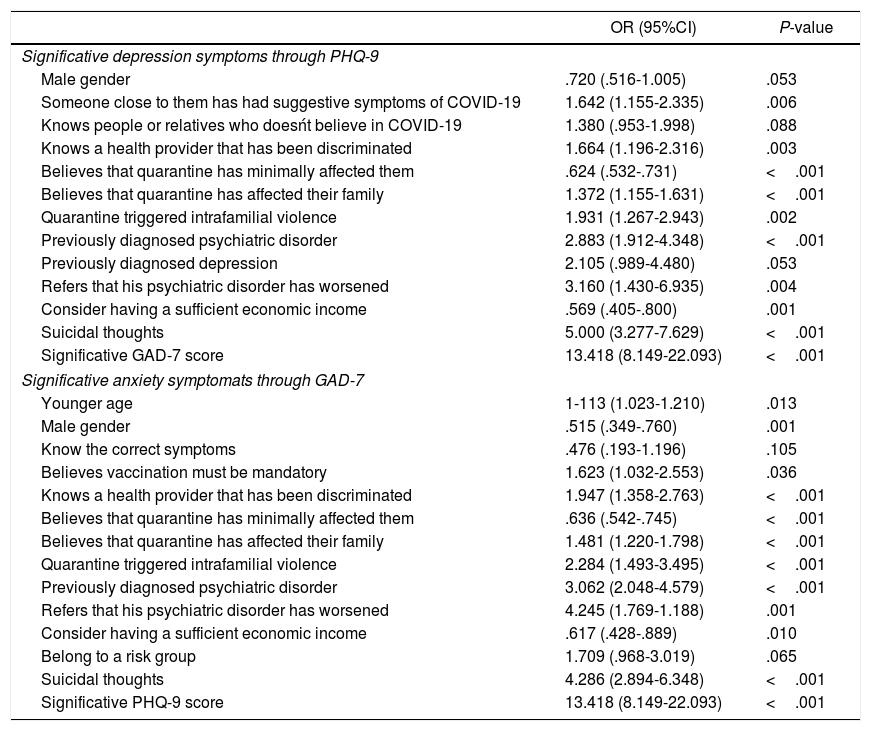
Odds ratio of variables as predictors of severe depression and/or anxiety staging in non-health-related college students.
| OR (95%CI) | P-value | |
|---|---|---|
| Significative depression symptoms through PHQ-9 | ||
| Male gender | .720 (.516-1.005) | .053 |
| Someone close to them has had suggestive symptoms of COVID-19 | 1.642 (1.155-2.335) | .006 |
| Knows people or relatives who doesńt believe in COVID-19 | 1.380 (.953-1.998) | .088 |
| Knows a health provider that has been discriminated | 1.664 (1.196-2.316) | .003 |
| Believes that quarantine has minimally affected them | .624 (.532-.731) | <.001 |
| Believes that quarantine has affected their family | 1.372 (1.155-1.631) | <.001 |
| Quarantine triggered intrafamilial violence | 1.931 (1.267-2.943) | .002 |
| Previously diagnosed psychiatric disorder | 2.883 (1.912-4.348) | <.001 |
| Previously diagnosed depression | 2.105 (.989-4.480) | .053 |
| Refers that his psychiatric disorder has worsened | 3.160 (1.430-6.935) | .004 |
| Consider having a sufficient economic income | .569 (.405-.800) | .001 |
| Suicidal thoughts | 5.000 (3.277-7.629) | <.001 |
| Significative GAD-7 score | 13.418 (8.149-22.093) | <.001 |
| Significative anxiety symptomats through GAD-7 | ||
| Younger age | 1-113 (1.023-1.210) | .013 |
| Male gender | .515 (.349-.760) | .001 |
| Know the correct symptoms | .476 (.193-1.196) | .105 |
| Believes vaccination must be mandatory | 1.623 (1.032-2.553) | .036 |
| Knows a health provider that has been discriminated | 1.947 (1.358-2.763) | <.001 |
| Believes that quarantine has minimally affected them | .636 (.542-.745) | <.001 |
| Believes that quarantine has affected their family | 1.481 (1.220-1.798) | <.001 |
| Quarantine triggered intrafamilial violence | 2.284 (1.493-3.495) | <.001 |
| Previously diagnosed psychiatric disorder | 3.062 (2.048-4.579) | <.001 |
| Refers that his psychiatric disorder has worsened | 4.245 (1.769-1.188) | .001 |
| Consider having a sufficient economic income | .617 (.428-.889) | .010 |
| Belong to a risk group | 1.709 (.968-3.019) | .065 |
| Suicidal thoughts | 4.286 (2.894-6.348) | <.001 |
| Significative PHQ-9 score | 13.418 (8.149-22.093) | <.001 |
GAD-7: General Anxiety Disorder-7; PHQ-9: Patient Health Questionnarie-9.
A logistic binary regression has been performed to assess variables that have a correlation with a P-value <.1. An odds ratio that won’t cross the 1 and a P-value <.05 has interpreted like significative.
Variables with positive association with significative anxiety symptomatology were: the age, believing the vaccination as mandatory, believing that quarantine had affected their family, knowing a health provider that had been discriminated, quarantine as a trigger for intrafamilial violence, previously being diagnosed with a mental health disorder, and belonging to a minority group. The negative association variables were identifying themselves as male, believing that quarantine affected minimally on them, and considering to have sufficient economic income. On the other hand, variables with positive association with significative anxiety symptoms on health-related students were: the age, knowing health providers that had been discriminated, believing that the quarantine had affected their family, being themselves violent, having a previous mental health disorder, being part of a minority or risk group, having tried drugs on quarantine, having suicidal thoughts with, and also having significative depression symptoms classification. The negative OR were identifying themselves as male, their family complied with quarantine, believing that it affected minimally on them, and considering to have sufficient economic income (Table 2 of the supplementary material).
As in significative depression symptomatology, the risk or protective factors for significative anxiety symptomatology were shared between both groups, however it is worth mentioning the factors they did not share. Among the health-related students, reporting that they are the most violent in their family and having used drugs to deal with the quarantine were risk factors for this group and that their families comply with the quarantine was a protective factor. On the other hand, the non-health-related students, knowing the COVID-19 symptoms and referring that their psychiatric disorder had get worst were risk factors for this group (Table 3 of the supplementary material and Table 4).
DiscussionTalking about the prevalence of anxiety disorders and depressive symptoms in medical students in the authors country, it had been found that anxiety significative symptomatology is present in 21.9%,28 and significative depression symptomatology in 23% in 2016,29 a notorious difference between what was found for the authors: health-related group presented 27.1% of significative anxiety symptoms and 47.1% significative depression symptoms. These findings are related with the general population thought that anxiety and depression disorders are greater in the medical student population than in the general population, as found in a study carried out in the United Arab Emirates by Saddik et al.,30 where an increase in pre-pandemic anxiety levels was reported to be 50% on university students in general. Although Salari et al.31 found a prevalence of 31.95% of anxiety symptoms and 33.7% of depression symptoms in their meta-analysis on general population during COVID-19, not only in significative levels; and even so the significative levels of the student sample were close, and the significative depression percentage were greater.
This study clearly shows the impact that COVID-19 pandemic has had within the college student population in the authors university as observed with the significative depression and anxiety levels that at the same should be monitored to observe how it will affect the performance of the student population in the near, medium term and distant future. According to The Global Burden of Diseases, Injuries, and Risk Factors Study 2017,32 the major depressive disorder had affected more than 264 million people worldwide; it is one of the main causes of work, school and family neglecting and is one of the leading causes to commit suicide with almost 800 000 people per year. Depression and anxiety appear as one of the main causes of disability producing disability and general limitation on daily life. The effect of COVID19 on communities had been significant, causing physical and psychosocial affections such as social distancing, the proper COVID-19 disease, fear, depression, economic recession, loss of college knowledge acquisition and professional practice (this is also real for any school degree), caused by the fear of obtaining the disease and its consequences or also by the government decisions to mitigate the impact. This is especially relevant in the student population, specifically health area students, most likely by the nature of their educational career, the interdisciplinary nature of their clinic practice, and the potential risk of presenting the disease themselves and infecting their family, demonstrated by Rastegar et al.33 The clinical practice on health area students have a special predisposition because is related with human health care; the existence of asymptomatic population may cause stress specially in dentist due to the proximity to the upper respiratory tract in their professional practice, something that can even have moral and ethical considerations, as referred by Coulthard.34 Although there was not found any special difference between our studied groups to develop depression or anxiety disorder; this could be approach in the future by separating the health area student group or by separating the first semester students against the clinical students (last years of the college, also called Interns). In any case, the student population at the authors university showed satisfactory knowledge about COVID-19 and declared that they mostly sought information from official media (although some did not fully trust it); this was demonstrated as a protective attitude by Saddik et al.30 with special emphasis on medical students in their studied group, demonstrating that greater knowledge about the pandemic was a protective factor that students from other careers did not showed. In our results we did not found this variable to be a protector factor, and also student that were not related to health-area that showed important knowledge presents more anxiety symptomatology. As the days move onward, in the country of the authors it had been seen how the number of cases do not decrease and the number of deaths continue growing, the number of cases never went lower than a plateau level; personal restrictions seems to increase and the population that seems to disregard the situation is precisely the young population (who, for the most part, are from the author's age group). Social restrictions and the government's effort to stop the pandemic seems to have no effect on this group, as they fall in the belief of feeling unsusceptible, a thought that was found in the student sample and also described by Zettler et al.35 It was showed that near half of the student sample do not fully respect the government measurements even when this was something expected for college students that referred to be informed about COVID-19 and its consequences; it is suggest that this could be because the mental health impact of social distancing and the change in daily life because, even half of our significative depression and anxiety symptomatology group referred to want to get back to normal activities before August 2020. The results of our study showed that the levels of anxiety and depression in university students are specially high, being women the most affected ones; this is similar to what is described by Liu et al.,36 that this clinical entities during COVID-19 pandemic were more common in female population, also referred by Pieh et al.;37 in the González et al. study, they found different results in Mexican students, were men seems to be the most affected.12
What makes our study unique is that we paid attention to the university population; group that have been suggested as one of the most affected ones during COVID-19 pandemic. It would be interesting to observe what would happen when the students return to their daily practice. College students are considered highly competitive and it should be taken into account; the demanding degree, the high stress levels that they are exposed to, combined with the pandemic are some of the factor to considering them as a risk group to develop mental health disorders during this time, as well as social distancing, the fear to get infected and affect their loved ones. According to what has been found in the literature, this is one of the first studies of this kind carried out in our state or country. More than 77% of the studied student sample showed anxiety symptomatology above the minimum referred by themselves; only 8.5% reported to not being affected in any way for the pandemic, and only 3.5% referred no anxiety symptoms on GAD-7 scale. Regarding depression, 2.52% reported no symptoms on PHQ-9; this differs from Gonzalez et al.12 results, where significative depression symptomatology was only present in 4.9% of students and anxiety symptomatology in 40.3% this could be explained because the sample size of our study (almost the double); COVID-19 is a red flag to the need to upgrade the actual college system but also an opportunity to improve opportunity areas. The limitations of this study are the lack of a follow-up, and the methodology nature carried out to obtain the answers (online); this is why it would be interesting to observe what happen with the same sample in a controlled clinical environment where these screening tests are validated.
ConclusionsWith the results combined and the information observed in literature, can be concluded that college students are a risk population for mental health illnesses being health-area students or not. This should be taken into account when authorities design strategies to develop effective online screening strategies for diagnosis and control for students with anxious, depressive or both symptoms, and offer services for them through online consults to improve the mental health and encourage resilience of the student population, a topic that continues to be a taboo.
These results were presented on the “VIII encuentro de Jóvenes Investigadores” of the authors university, where they were evaluated by the authors university authorities, and was also awarded for the second place on the category “Ciencias Sociales.” The meeting represents an opportunity to manifest worries, growth opportunities, among others; in this case the authorities of university exported their recognition of the work, and decided to start working on validation of online screening instruments, and ask for a follow-up study from us and do themselves a survey including all the student body (from high-school to postgraduate); for the students with anxiety and depression significative symptomatology it was decided to restart the program PASSWORD where students from the university can ask for a consultation with a psychiatry or psychology from the University Hospital via online; and to promote different strategies to improve mental health through social media, anyways, these are first steps on an important topic addressing mental health on university students.38,39
Conflict of interestsThe authors acknowledge the search was made in the absence of any financial or commercial interest that might be considered as a conflict of interest.
To the student body of the university that participated in this study; to the BSc Valeria Flores Tamez that helped us with statistical analyses.
Gian Marcelo Maciel-Barrientos, Luis Saucedo-Charles, Rebeca Polina-Lugo, Jorge Elizalde-Ojeda, Christian Martínez-Rodríguez, Marcela López-Ayala, Jorge Zamayoa-Torres, Celica González-Galván, Alexis Sosa-Colunga, Emanuel Navarrete-Juárez, Humberto Gómez-López, Paula De La Garza-Manrique, Ángel Delgado-Banda, Ricardo Galicia-Carriles, Clarissa Cavazos-Guerrero, Diego Ortega-Moreno, Ricardo Tello-Mendoza, Raymundo Chávez-Gamboa, Cecilia Xolalpa-Rosales.