Delirium is a common neuropsychiatric syndrome with severe consequences, especially for elderly patients with pre-existing cognitive impairment.
MethodologyDescriptive study of one retrospective cohort, with the aim of comparing risk factors and mortality between surgical treatment and non-surgical treatment in a group of hospitalised patients with delirium.
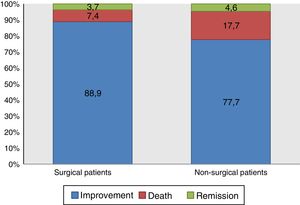
ResultsOf the 184 hospitalised patients with delirium analysed, 29.3% were for surgical causes and 70.7% for non-surgical causes. Just over half (50.5%) were women, and 50% of the patients were 74 years or less (interquartile range, 27 years), with statistical differences (P=.002). Prior cognitive impairment was observed in 42.9% of patients, with a greater proportion of non-surgical (50.8% vs 24.1%) with significant differences (P=.001). Anticholinergic medications were received by 89.7% of patients, and almost all of them (99.5%) received three or more medicines, with no significant differences. Half (50%) of the patients remained in hospital for 16.3 days or less (interquartile range, 23 days). Hospitalisation was significantly longer in the surgical group (P<.001). The hospital mortality was 14.7%, with no statistical differences between groups (P=.073).
DiscussionAlthough there were no significant differences in mortality between the groups, it was higher in the non-surgical (17.7% vs. 7.4%). Increased mortality was found in the older group (non-surgical) that also had significantly greater cognitive impairment, which coincides with that in the scientific literature.
El delirium es un síndrome neuropsiquiátrico frecuente y con graves consecuencias, especialmente para los pacientes ancianos y con deterioro cognitivo preexistente.
MétodosEstudio descriptivo de una única cohorte retrospectiva. El objetivo es comparar los factores de riesgo y la mortalidad según el tipo de tratamiento (quirúrgico y no quirúrgico) en un grupo de pacientes con delirium hospitalizados.
ResultadosSe analizó a 184 pacientes con delirium hospitalizados, por causas quirúrgicas el 29,3% y no quirúrgicas el 70,7%. El 50,5% eran mujeres; el 50% de los pacientes tenían 74 años o menos (intervalo intercuartílico, 27 años), con diferencias estadísticas, siendo mayores los no quirúrgicos (p = 0,002). El 42,9% de los pacientes presentaban deterioro cognitivo previo, con mayor proporción entre los no quirúrgicos (el 50,8 frente al 24,1%) y diferencias significativas (p = 0,001). El 89,7% recibía medicamentos anticolinérgicos y el 99,5%, más de 3 medicamentos, sin diferencias significativas. La mitad de los pacientes permanecieron en hospitalización 16,3 días o menos (intervalo intercuartílico, 23 días), y fue significativamente más larga la estancia en el grupo quirúrgico (p < 0,001); el 14,7% de los pacientes murieron en el hospital, sin diferencias estadísticas entre los grupos (p = 0,073).
DiscusiónNo hubo diferencias significativas en la mortalidad entre los grupos, si bien fue mayor en el no quirúrgico (el 17,7 frente al 7,4%). En cuanto a la edad, se encontró que el grupo de mayor mortalidad (el no quirúrgico) tenía una edad y un deterioro cognitivo significativamente mayores, lo cual coincide con la literatura científica.
Delirium is a common neuropsychiatric syndrome with serious consequences for hospitalised patients, especially older patients with pre-existing cognitive impairment.1,2 It has been conceptualised as an attention deficit problem that develops in hours to days and is the direct consequence of a general medical condition or intake of drugs and toxins.3,4 The prevalence of delirium varies in different clinical scenarios: in the emergency department, 10%; in hospital admission wards, 10–30%; in surgical wards, 15–53%; in non-ventilated patients in intensive care, 30–50%, and in patients with mechanical ventilation, 80%.5,6 Delirium can be preceded by a 2–3-day prodromal phase of poor concentration, anxiety, irritability and sleep disturbance.7
The sequelae of delirium can include prolonged hospitalisation, increased morbidity and mortality rates and a greater likelihood of needing residential care.8,9 A meta-analysis that included 2000 patients aged over 65 years found that the risk of death increased from 27.5% to 38% in patients with delirium, the risk of admission to a geriatric institution increased from 10.7% to 33.4% and the risk of dementia soared from 8.1% to 62.5%.10 The additional costs of treating a patient with delirium were estimated at 16,303 to 64,421 US dollars, which would be equivalent to 38 to 152 billion US dollars attributable to delirium for one year of treatment.11
Other negative outcomes associated with in-hospital delirium are: falls, pressure ulcers, urinary incontinence and removal of catheters and tubes12,13; prolonged hospital stay14,15; reduced mobilisation and worse performance in activities of daily living (ADL)16–18; and use of mechanical restraints.19
The aim of this research was to compare the incidence of hospital mortality in surgical and non-surgical patients diagnosed with delirium and associated sociodemographic and clinical factors.
Material and methodsThis was a descriptive study of a single retrospective cohort, taking as a unit of analysis the medical records of hospitalised patients who were diagnosed with delirium by a psychiatrist through an unstructured interview according to DSM-5 criteria, from August 2013 to December 2014, in a public hospital dealing with patients of high medical complexity in the city of Medellín, Colombia.
The inclusion criterion was the diagnosis of delirium by a psychiatrist during the study period. No exclusion criteria were applied. The endpoint was defined as hospital death or hospital discharge due to improvement. The variables considered were sociodemographic (age, gender and education) and clinical (principal diagnosis, comorbid diagnosis, admission to intensive care). The risk factors for delirium were: auditory and visual deficit, urinary catheter, surgical treatment, pharmacological and non-pharmacological treatment for delirium, use of benzodiazepines, use of anticholinergic drugs, polypharmacy (use of more than three drugs during hospitalisation); laboratory tests: haemoglobin, creatinine, blood glucose, fluid/electrolyte imbalance, vitamin B,12 folic acid; psychiatric history and cognitive impairment.
Patients were identified, and information compiled from the Hospital's Liaison Psychiatry Unit clinical database, a computerised database where the medical record numbers of patients diagnosed with delirium are recorded. These medical records were subsequently searched for in the electronic medical record of the hospital where the study was conducted, and the required information was extracted. Only one of the investigators carried out the search and recorded the information.
To keep information bias to a minimum, care was taken with the quality of the data collected. The information was analysed with the software SPSS 21.0®, licensed to Universidad CES.
To describe the sociodemographic characteristics of the study population, the median [interquartile range] was used because age did not have a normal distribution. For the qualitative variables, we used absolute values, ratios and proportions. For the bivariate analysis, significance tests such as the χ2 and the Fischer exact test, the Mann–Whitney U test and the McNemar test were used, and p values and 95% confidence intervals were reported (95% CI). The groups were compared by age, gender, education and type of treatment (surgical or non-surgical). The outcomes of improvement and death were compared in the groups studied. This project was approved by the Research Committee of the Universidad CES and the Hospital where the research was carried out.
ResultsSocial and demographic characteristics of patients according to study groupWe analysed 184 patients admitted to a hospital that treats high-complexity patients who were diagnosed with delirium by a psychiatrist; 29.3% came from a surgical intervention, while the remaining 70.7% were in hospital admissions for some other reason.
In general, there was a similar distribution by gender, with 50.5% of the patients being female. When discriminating according to the study group, no statistical differences were found (χ2 test of independence, p=0.675), although the distribution varied as more males were found among surgical patients (51.9%) and more females among those not coming from surgery (51.5%).
At the time of admission, 50% of the patients were aged ≤74 [27] years, with statistical differences according to the group; those who had not undergone surgery were older (Mann–Whitney U, p=0.002).
The educational level of 63.0% of patients was unknown. However, the majority of those for whom data were available had at most primary education (44.1%), followed by a group who were illiterate (25.0%), those who had completed secondary school (19.1%), professional studies (10.3%) and technical level (1.5%).
Although without statistical differences between the groups, 88.2% of the patients had a caregiver during their hospital stay (χ2 test of independence, p=0.329).
Clinical characterisation of the patients and the hospital carePrior to their admission to hospital, 42.9% of the patients already had cognitive impairment, with the proportion among non-surgical patients being significantly higher (50.8% vs 24.1%) (χ2 test of independence, p=0.001). In terms of the type of impairment, 53.2% had suspected dementia, 22.8% moderate dementia, 13.9% mild dementia and 10.1% severe dementia. A psychiatric history was documented in 63.3% of the cases (46.2% of the surgical patients and 66.7% of the non-surgical patients), without statistical differences (Fisher's exact test, p=0.211).
Visual deficit occurred in 7.7% of the surgical patients and 4.5% of the non-surgical patients, while 15.4% of the surgical patients had auditory deficit as opposed to 6.1% of the non-surgical patients, without statistical differences in the prevalences according to study group (Fisher's exact test, p>0.05 in both cases).
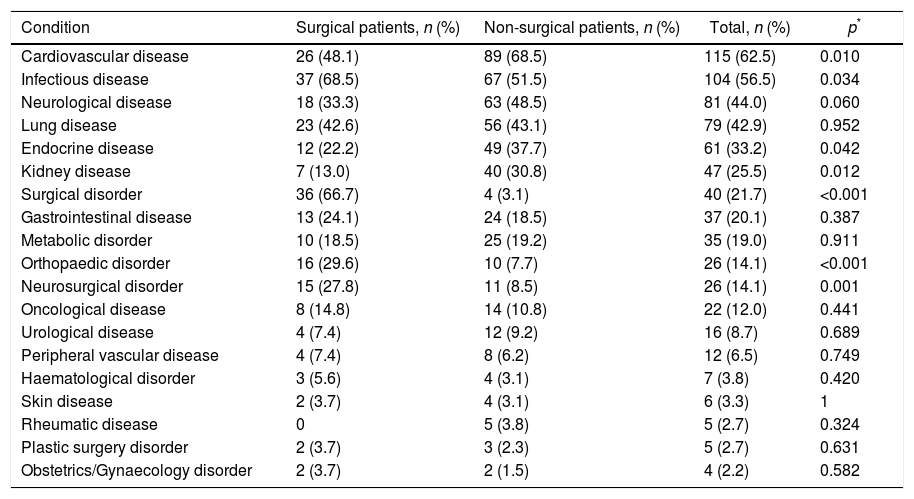
The patients’ comorbidities were also assessed, with cardiovascular diseases being the most prevalent, followed by infectious and neurological diseases. As shown in Table 1, statistical differences were found in the occurrence of some comorbidities according to the group: the proportion of cardiovascular, endocrine and renal diseases was higher among the non-surgical patients, while infectious diseases and surgical, neurosurgical and orthopaedic disorders were more prevalent among the surgical patients.
Medical comorbidities of patients with delirium.
| Condition | Surgical patients, n (%) | Non-surgical patients, n (%) | Total, n (%) | p* |
|---|---|---|---|---|
| Cardiovascular disease | 26 (48.1) | 89 (68.5) | 115 (62.5) | 0.010 |
| Infectious disease | 37 (68.5) | 67 (51.5) | 104 (56.5) | 0.034 |
| Neurological disease | 18 (33.3) | 63 (48.5) | 81 (44.0) | 0.060 |
| Lung disease | 23 (42.6) | 56 (43.1) | 79 (42.9) | 0.952 |
| Endocrine disease | 12 (22.2) | 49 (37.7) | 61 (33.2) | 0.042 |
| Kidney disease | 7 (13.0) | 40 (30.8) | 47 (25.5) | 0.012 |
| Surgical disorder | 36 (66.7) | 4 (3.1) | 40 (21.7) | <0.001 |
| Gastrointestinal disease | 13 (24.1) | 24 (18.5) | 37 (20.1) | 0.387 |
| Metabolic disorder | 10 (18.5) | 25 (19.2) | 35 (19.0) | 0.911 |
| Orthopaedic disorder | 16 (29.6) | 10 (7.7) | 26 (14.1) | <0.001 |
| Neurosurgical disorder | 15 (27.8) | 11 (8.5) | 26 (14.1) | 0.001 |
| Oncological disease | 8 (14.8) | 14 (10.8) | 22 (12.0) | 0.441 |
| Urological disease | 4 (7.4) | 12 (9.2) | 16 (8.7) | 0.689 |
| Peripheral vascular disease | 4 (7.4) | 8 (6.2) | 12 (6.5) | 0.749 |
| Haematological disorder | 3 (5.6) | 4 (3.1) | 7 (3.8) | 0.420 |
| Skin disease | 2 (3.7) | 4 (3.1) | 6 (3.3) | 1 |
| Rheumatic disease | 0 | 5 (3.8) | 5 (2.7) | 0.324 |
| Plastic surgery disorder | 2 (3.7) | 3 (2.3) | 5 (2.7) | 0.631 |
| Obstetrics/Gynaecology disorder | 2 (3.7) | 2 (1.5) | 4 (2.2) | 0.582 |
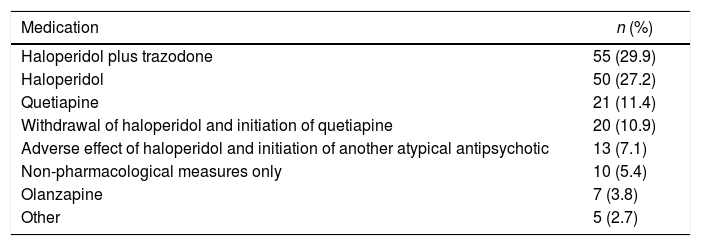
Apart from one surgical patient, all received treatment for delirium; the type of psychotropic drugs provided is shown in Table 2.
Medications for delirium given to hospitalised patients.
| Medication | n (%) |
|---|---|
| Haloperidol plus trazodone | 55 (29.9) |
| Haloperidol | 50 (27.2) |
| Quetiapine | 21 (11.4) |
| Withdrawal of haloperidol and initiation of quetiapine | 20 (10.9) |
| Adverse effect of haloperidol and initiation of another atypical antipsychotic | 13 (7.1) |
| Non-pharmacological measures only | 10 (5.4) |
| Olanzapine | 7 (3.8) |
| Other | 5 (2.7) |
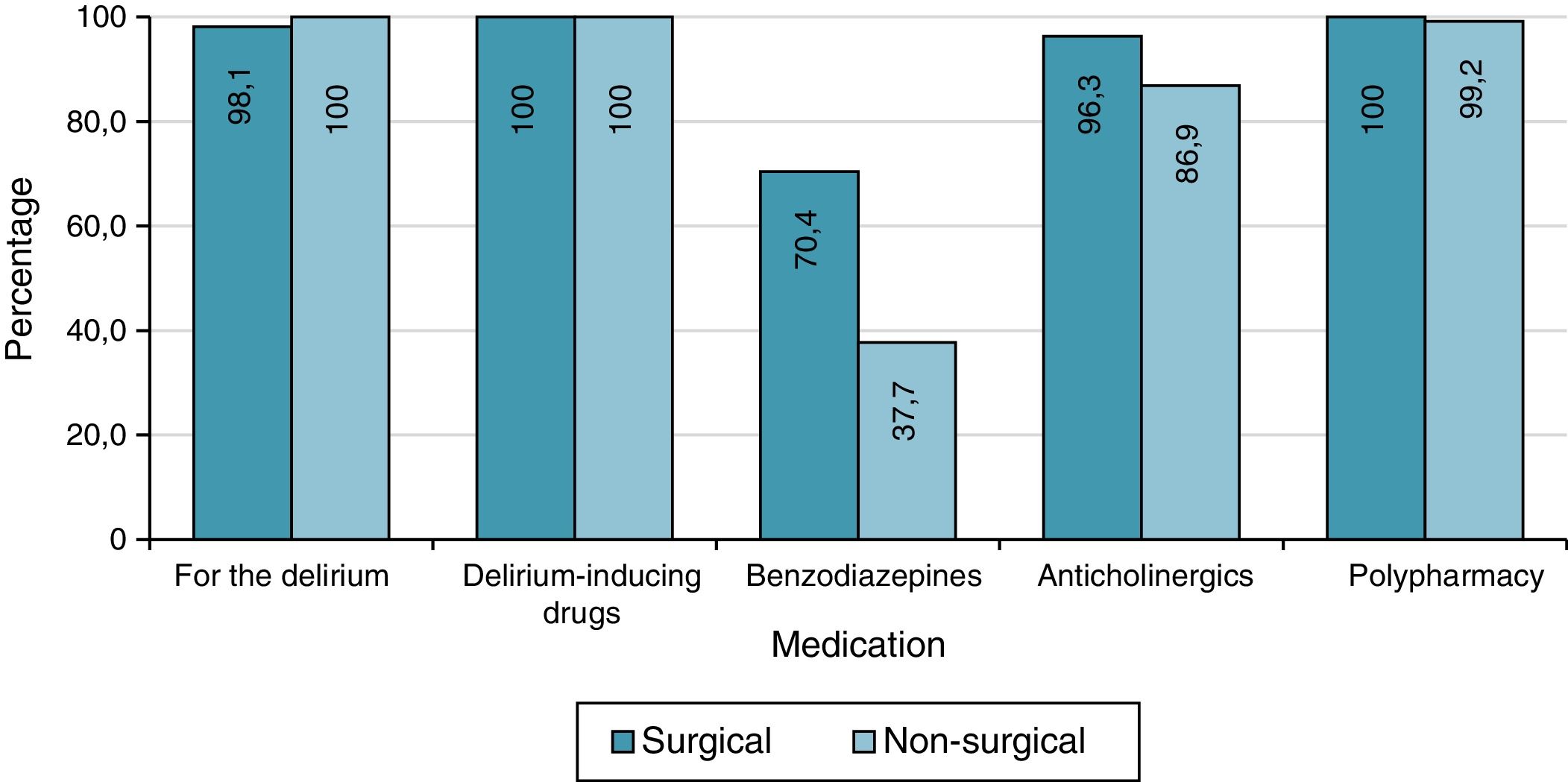
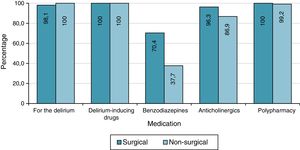
All patients received delirium-inducing drugs, while benzodiazepines were used during hospitalisation in 47.3% of cases, with statistical differences (χ2 test of independence, p<0.001) between the two groups (70.4% in the surgery group vs 37.7% in the non-surgery group (Fig. 1).
Anticholinergic drugs were prescribed to 89.7% of patients, while 99.5% were receiving more than three drugs at the same time, with no differences between the study groups in either case (χ2 test of independence, p=0.057; Fisher's exact test, p=1).
Overall, 22.8% of the patients were admitted to the intensive care unit (ICU), with the proportion higher among surgical than non-surgical patients (53.7% vs 10.0%, χ2 test of independence, p<0.001). The proportion of surgical patients with uncontrolled pain was also higher (25.9% vs 7.7%; χ2 test of independence, p=0.001). During their stay in hospital, 3.3% of patients suffered falls, this time without differences between the study groups (Fisher's exact test, p=1).
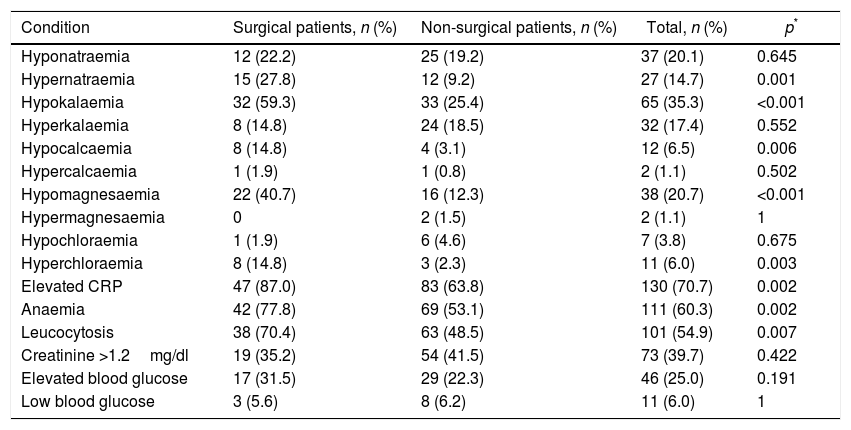
Differences were found in the presence of comorbidities during hospitalisation; among surgical patients, there was a higher rate of occurrence of hypernatraemia, hypokalaemia, hypocalcaemia, hypomagnesaemia, hyperchloraemia, elevated C-reactive protein, anaemia and leucocytosis (Table 3).
Comorbidities of hospitalised patients with delirium.
| Condition | Surgical patients, n (%) | Non-surgical patients, n (%) | Total, n (%) | p* |
|---|---|---|---|---|
| Hyponatraemia | 12 (22.2) | 25 (19.2) | 37 (20.1) | 0.645 |
| Hypernatraemia | 15 (27.8) | 12 (9.2) | 27 (14.7) | 0.001 |
| Hypokalaemia | 32 (59.3) | 33 (25.4) | 65 (35.3) | <0.001 |
| Hyperkalaemia | 8 (14.8) | 24 (18.5) | 32 (17.4) | 0.552 |
| Hypocalcaemia | 8 (14.8) | 4 (3.1) | 12 (6.5) | 0.006 |
| Hypercalcaemia | 1 (1.9) | 1 (0.8) | 2 (1.1) | 0.502 |
| Hypomagnesaemia | 22 (40.7) | 16 (12.3) | 38 (20.7) | <0.001 |
| Hypermagnesaemia | 0 | 2 (1.5) | 2 (1.1) | 1 |
| Hypochloraemia | 1 (1.9) | 6 (4.6) | 7 (3.8) | 0.675 |
| Hyperchloraemia | 8 (14.8) | 3 (2.3) | 11 (6.0) | 0.003 |
| Elevated CRP | 47 (87.0) | 83 (63.8) | 130 (70.7) | 0.002 |
| Anaemia | 42 (77.8) | 69 (53.1) | 111 (60.3) | 0.002 |
| Leucocytosis | 38 (70.4) | 63 (48.5) | 101 (54.9) | 0.007 |
| Creatinine >1.2mg/dl | 19 (35.2) | 54 (41.5) | 73 (39.7) | 0.422 |
| Elevated blood glucose | 17 (31.5) | 29 (22.3) | 46 (25.0) | 0.191 |
| Low blood glucose | 3 (5.6) | 8 (6.2) | 11 (6.0) | 1 |
Vitamin B12 deficiency was found in 14.7% of the patients and abnormal thyrotropin in 17.9%, but these parameters were not measured in roughly half of the patients (54.3% of surgical and 42.9% of non-surgical).
Length of hospital stay until discharge due to improvement or in-hospital deathIn general, for half of the patients the hospital stay was ≤16.3 [3.23] days. It was significantly longer for the surgical patients (median 32 [36.0] days), than for the non-surgical patients (median ≤13 [2.14] days) (Mann–Whitney U, p<0.001).
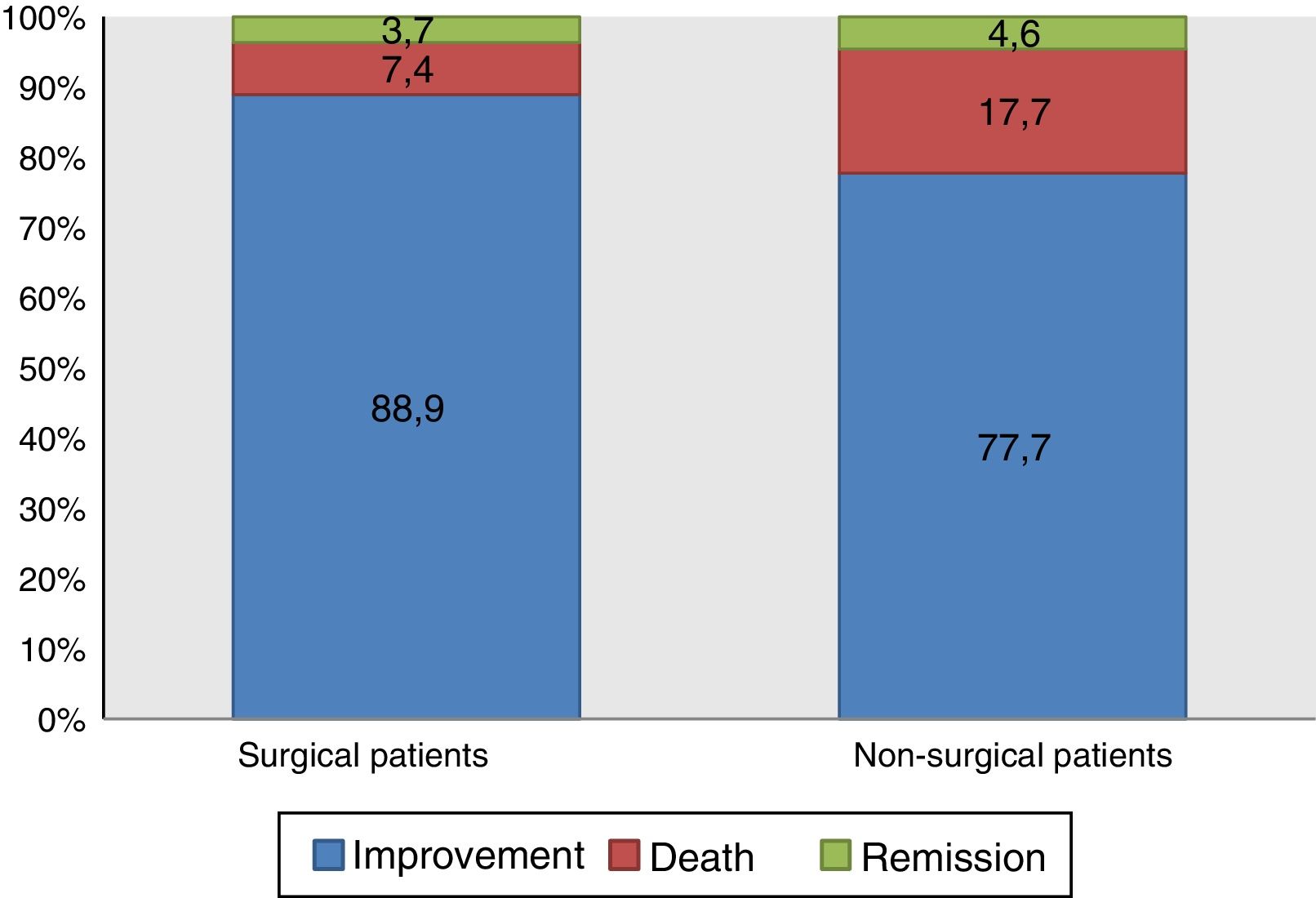
As shown in Fig. 2, although the health status of most of the patients who suffered delirium during their hospital stay improved and they were discharged, 14.7% died. Although no statistical differences were found, mortality was higher among those who had not undergone surgery (χ2 test of independence, p=0.073).
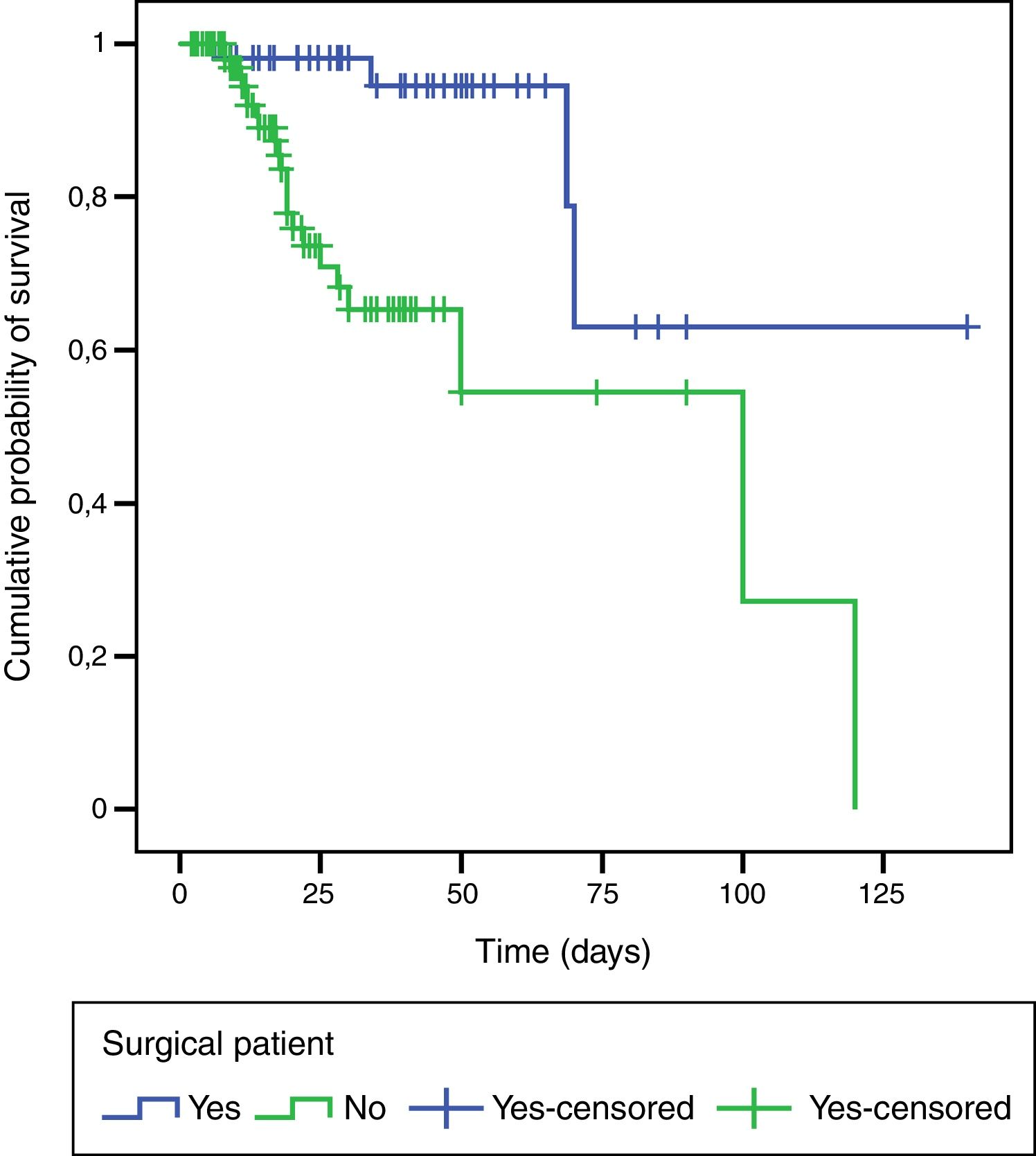
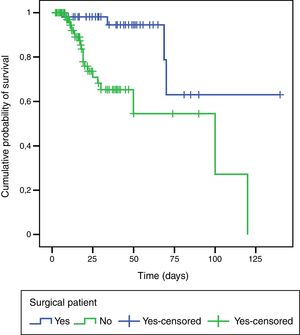
An exploratory survival analysis was performed to compare the time spent in hospital until death. Fig. 3 shows the survival curves for the groups estimated by Kaplan–Meier (log-rank test, p=0.001); the likelihood of patients with delirium surviving was higher among those who had undergone surgery.
DiscussionThis study assessed the risk factors and in-hospital mortality rate of surgical and non-surgical patients with delirium. The results indicate that, although the mortality rate was higher in the non-surgical group (17.7% vs 7.4%), this difference was not statistically significant. The group with greater mortality (non-surgical group) was significantly older and with a significantly higher degree of cognitive impairment, in line with the findings of other studies that show that advanced age and cognitive impairment are independent risk factors for higher delirium-associated mortality rates.20–22 In one study, Sampson et al.23 found that the risk of death increased significantly with the degree of cognitive impairment prior to hospital admission (hazard ratio [HR]=4.02; 95% confidence interval [95% CI], 2.24–7.36, p<0.001).
Advanced age is a factor constantly associated with delirium,2,20 but when attempting to clarify the relationship between delirium, dementia and higher mortality rates, some studies have found delirium alone to be an independent risk factor,24,25 while others report that, unlike cognitive impairment and the severity of the disease, delirium is not a factor associated with higher mortality rates.26–29
A systematic review conducted by Jackson et al.30 looking for prognostic factors in patients with in-hospital delirium found 18 predictors of poor prognosis. Of these predictors, the duration of the delirium, the hypoactive subtype and comorbidity with depression and dementia showed the strongest association. Our study found that the majority of patients received anticholinergic drugs, benzodiazepines and polypharmacy. Inouye et al. found double the risk of delirium in patients with polypharmacy (odds ratio [OR]=2.9; 95% CI, 1.6–5.4).31 Pisani et al. reported that the use of benzodiazepines was an independent risk factor for delirium for patients in intensive care.32
With regard to sensory deprivation, visual and auditory deficits have been associated with a higher prevalence of delirium.33 Our study found no statistical differences in the prevalences of these deficits. Medical comorbidities that indicate disease severity have been associated with delirium.34,35 Our study found significant differences in the prevalences of cardiovascular and endocrine disease in non-surgical patients and infectious disease in surgical patients.
In their meta-analysis, Ahmet et al. identified 29 delirium risk factors such as low haematocrit and abnormal urea, leucocytes and albumin.36 Our study found high prevalences of laboratory-test abnormalities, without significant differences between the study groups.
A study by McCusker et al.37 found that in-hospital incident delirium was associated with an increase in hospital stay of approximately eight days. Our results show that the patients in the surgical group had a significantly longer hospital stay than the non-surgical group and longer than the average (12 days) for the hospital where the study population was obtained.
This study had the following limitations: (a) because it is a retrospective study, complete information was not available for all study variables; (b) delirium and dementia were not diagnosed with validated instruments, although psychiatrists highly trained in delirium performed all the diagnoses; (c) due to the methodology used, caution is advised when interpreting the results and considering possible causality; (d) the reported mortality rate was derived from incident and prevalent cases of delirium; (e) although most of the patients in the two groups experienced clinical improvement, no neuropsychological scale was applied which might have detected the subtle neurocognitive alterations that frequently persist after discharge; and (f) there was no delirium-free control group, so we cannot guarantee that the differences found are fully attributable to the delirium. Despite these limitations, our study provides valuable information on the comparison of surgical and non-surgical patients with delirium.
Lastly, advanced age and cognitive impairment were determining factors of the higher mortality rate in the non-surgical patient group in this study. The appropriate recognition and treatment of a number of potentially modifiable risk factors (including polypharmacy, use of benzodiazepines, fluid/electrolyte imbalance and anaemia) would help reduce the onset and duration of delirium and perhaps improve the prognosis and survival of these patients.
Ethical disclosuresProtection of human and animal subjectsThe authors state that the procedures followed conformed to the ethical standards of the responsible human experimentation committee and to the World Medical Association and the Declaration of Helsinki.
Confidentiality of dataThe authors declare that they have followed the protocols implemented in their place of work regarding the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
We would like to thank our patients, Universidad CES and Hospital General de Medellín.
Please cite this article as: Restrepo D, Duque M, Montoya L, Berrouet MC, Rojas M, Lopera G, et al. Factores de riesgo y mortalidad hospitalaria de los pacientes quirúrgicos y no quirúrgicos con delirium. Rev Colomb Psiquiat. 2018;47:148–154.