Depression is the most common psychiatric morbidity in pregnancy, affecting more than 13% of pregnant women. Its diagnosis is based on the criteria established by the DSM-5 and the application of validated scales such as the Edinburgh Postnatal Depression Scale. However, there are still errors and shortcomings among healthcare professionals in the recognition, diagnosis and treatment of depression during pregnancy, with the resulting consequences and repercussions on the gestation itself or the foetus.
ObjectiveTo present a review of depression in pregnancy, its risk factors, clinical characteristics, complications and treatment.
MethodsThe PubMed and LILACS databases were used to search for manuscripts. Of the 223 articles found, 55 fulfilled the inclusion criteria.
ResultsThe prevalence of depression in pregnancy in South America is approximately 29% and the most significant risk factors are sexual abuse, pregnancy at an early age and intrafamily violence. Therefore, early diagnosis favours a reduction in risk behaviour, foetal neurodevelopmental disorders and obstetric outcomes.
ConclusionsDepression in pregnancy is common condition but is underreported as its symptoms are often attributed to the pregnancy itself. The use of selective serotonin reuptake inhibitor antidepressants, particularly fluoxetine, which has not been associated with teratogenicity, is recommended, in addition to the implementation of non-pharmacological treatment such as psychotherapy, mindfulness and aerobic exercise. Educating healthcare professionals will facilitate the correct diagnosis and treatment of this condition.
La depresión es la morbilidad psiquiátrica más común en el embarazo, y llega a afectar a más del 13% de las gestantes. Su diagnóstico se basa en los criterios establecidos por el DSM-V y la aplicación de escalas validadas como la Escala de Depresión Posnatal de Edimburgo; sin embargo, entre los profesionales de la salud aún existen errores y falencias en el reconocimiento, el diagnóstico y el tratamiento de la depresión durante el embarazo, lo que propicia las diferentes consecuencias y repercusiones para la gestación misma o el feto.
ObjetivoPresentar una revisión de tema acerca de la depresión en el embarazo, sus factores de riesgo, las características clínicas, las complicaciones y el tratamiento.
MétodosSe utilizaron las bases de datos PubMed y LILACS para la búsqueda de manuscritos; de 223 artículos, 55 cumplían los criterios de inclusión.
ResultadosEn Sudamérica se registra una prevalencia de aproximadamente el 29%. Los factores de riesgo con mayor significación son el abuso sexual, la edad temprana al embarazo y la violencia intrafamiliar. Por ello, el diagnóstico temprano favorece la disminución en las conductas de riesgo, los trastornos del neurodesarrollo foetal y los resultados obstétricos.
ConclusionesLa depresión en el embarazo es una afección frecuente; no obstante, se presenta subregistro por la atribución de los síntomas a la gestación misma. Se recomienda el uso de antidepresivos como los inhibidores de la recaptación de serotonina, especialmente la fluoxetina, que no sae ha relacionado con teratogenicidad, además de la implementación de tratamiento no farmacológico como psicoterapia, mindfulness y ejercicio aeróbico. La sensibilización del personal de salud permitirá el diagnóstico y el tratamiento adecuados de esta enfermedad.
Pregnancy is recognised as a period of profound change for both the pregnant woman and her family.1 It has been highlighted as a state of adequate mental and physical health, and proposed as a protective factor against mood disorders. However, for some women, the gestational period can increase their vulnerability to psychiatric diseases like depression. Prospective longitudinal studies have found that pregnancy is not a protective factor against new depressive episodes or relapses in cases of pre-existing depression.2,3
Antenatal depression affects 8–11% of women in developed countries,4 while general depression rates during pregnancy reach 13%,5 being the second cause of incapacity among women.6,7 The number of pregnant women prescribed antidepressants has increased drastically over the past two decades.8 Some studies have shown that anxiety and depression in pregnancy increase the risk of preterm labour, altered foetal neurodevelopment, a low Apgar score and a low birth weight.9 Moreover, increased rates of substance abuse and low participation in prenatal monitoring programmes during pregnancy have also been observed.10,11
Despite the risk of the pregnant patient suffering mental health problems, healthcare professionals still make mistakes and fail to recognise, diagnose and treat depression in pregnancy. Given the possible teratogenic effects of many drugs used to treat psychiatric disorders, it is important to be aware of and to prescribe safe tools for the treatment of depression in medical care.1 The objective of this review is to carry out a comprehensive approach to depression in pregnancy for early diagnosis and adequate clinical treatment.
MethodsA literature search relating to depression in pregnancy was performed by consulting the PubMed and LILACS databases, using the following keywords “Depression AND Pregnancy” and “Unipolar major depression AND pregnant women”. The inclusion criteria were studies performed in humans, meta-analyses, original articles and systematic reviews, in English and Spanish, and keywords in the title. The exclusion criteria were articles for which the final version was not available and conclusions not related to the keywords. A total of 223 articles were obtained, of which 168 were excluded since they did not meet the inclusion criteria or had been accepted only to then meet the exclusion criteria. Eventually, 55 publications were selected, having been separately assessed by two authors and then compared. Variables such as aetiology, treatment and complications were assessed, the analysis and discussion of which are presented in the manuscript.
EpidemiologyDepression is the second cause of incapacity in women and the most common morbidity in pregnancy. A meta-analysis performed by Bennet et al.7 found that depressive symptoms mostly presented in the second (13%) and third (12%) trimesters of pregnancy, compared to the first trimester, in which only 7% of the study population presented symptoms. In Colombia, according to a study performed by Borda et al., the prevalence of depression in pregnancy is around 19%. However, in a study conducted by Bonilla-Sepúlveda with teenage mothers in a Colombian city, they found a greater prevalence of the condition, of up to 32.8%.12,13 In contrast, prevalence rates of 40.1% in Peru, 30.7% in Mexico and 29% in South America have been recorded, thereby confirming the importance of treating this disorder both in Colombia and worldwide.14,15 It should be noted that these studies were done on low-risk pregnant women who had not been attended for depressive symptoms.
However, the data published are not totally reliable due to the fact that only a small proportion of pregnant women are given a full diagnosis, since the symptoms of the disease, such as changes in appetite, sleeping patterns and tiredness, are normally attributed to pregnancy itself, with the possibility of a depressive episode being ignored.16,17
Risk factorsThe reason for which pregnancy is not protective against mood disorders like depression in some women remains unknown. However, it should be remembered that depression is a condition with a multifactorial aetiology, so hormonal and neuroendocrine changes in this phase, as well as psychosocial and environmental changes, should not be ruled out. An understanding of the different risk factors for this disease will enable different prevention and treatment strategies to be optimised in health care.7
In many cases, it is wrongly believed that during pregnancy women do not experience stressors or situations that put their mental health at risk or, conversely, that these stressors do not have an effect on the development of the unborn child. As a result, antenatal checks focus on preventing foetal complications and the mother's emotional state is neglected. According to the findings of a Washington University analysis by Woods et al., of a total of 1522 patients assessed in pregnancy, 78% reported some degree of stress and 6% reported a high level of stress.18
The risk factors for depression in pregnancy can be classified as biological or psychosocial and range from a background of depression and premenstrual dysphoric disorder to a history of sexual abuse, being young and pregnant, limited social support, psychoactive substance use and intra-family violence.19 Lancaster et al., through a systematic review of 57 studies (following an analysis of 1361 previously selected articles), established, with strong evidence, daily stress as a risk factor, which includes adverse life events, a lack of social support or weak support networks and intra-family violence.20,21 Moreover, a Peruvian study conducted by Lam et al. revealed the most influential risk factors in the sample studied to be a history of abortion, a lack of family planning, the low education level of the pregnant woman versus the higher education level of the partner and a history of violence, which has the greatest statistical significance.22
The least influential risk factors included unemployment and a low income, indicating that, although socioeconomic class does not have a major statistical impact, it may influence the onset of depression during and after pregnancy.23 The presence of two or more factors increases the risk of the pregnant woman suffering a major depressive episode and her symptoms having a major impact on her daily life. Nonetheless, factors such as a history of abortion, violence and a lack of social support are independent factors which, alone, should alert healthcare professionals to a probable case of antenatal depression.22
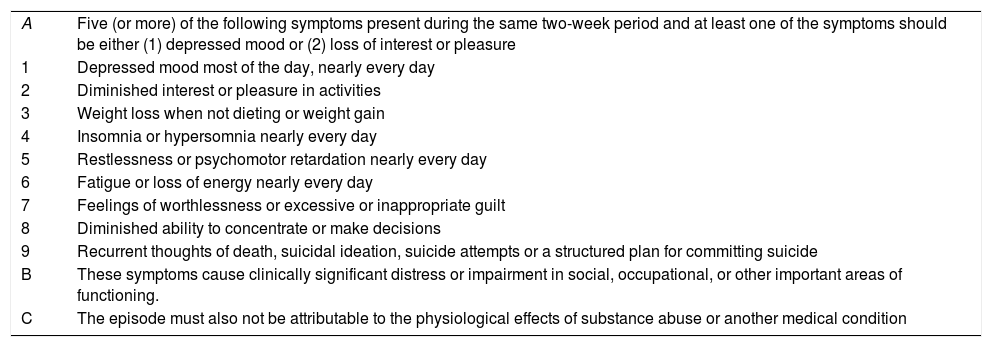
Clinical manifestations and diagnosisThe diagnosis of a major depressive episode, in both the general population and pregnant women, is usually based on the clinical signs and symptoms defined in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) (Table 1).24 In order to identify the most common symptoms during depression in pregnancy, the Edinburgh Postnatal Depression Scale and Beck Depression Inventory have been validated and used, both of which seek to divide the population in question into two groups (patients at risk for depression and patients with no risk for depression), assessing dichotomous variables, and, despite overestimations, the results show great specificity and clinical significance.9,14
Diagnosis of a major depressive episode according to DSM-5 criteria.
| A | Five (or more) of the following symptoms present during the same two-week period and at least one of the symptoms should be either (1) depressed mood or (2) loss of interest or pleasure |
| 1 | Depressed mood most of the day, nearly every day |
| 2 | Diminished interest or pleasure in activities |
| 3 | Weight loss when not dieting or weight gain |
| 4 | Insomnia or hypersomnia nearly every day |
| 5 | Restlessness or psychomotor retardation nearly every day |
| 6 | Fatigue or loss of energy nearly every day |
| 7 | Feelings of worthlessness or excessive or inappropriate guilt |
| 8 | Diminished ability to concentrate or make decisions |
| 9 | Recurrent thoughts of death, suicidal ideation, suicide attempts or a structured plan for committing suicide |
| B | These symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning. |
| C | The episode must also not be attributable to the physiological effects of substance abuse or another medical condition |
Source: American Psychiatric Association (2013).
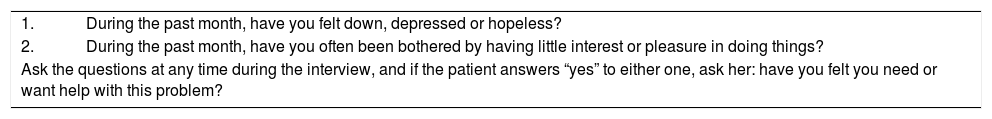
International institutions such as the United Kingdom's National Institute for Health and Care Excellence (NICE) have recommended, based on the aforementioned scales, that two questions be asked as part of an investigation that enables the identification, diagnosis and timely treatment of the condition (Table 2).5,25 Women who score positively on this quick depression test should be referred for a full mental health assessment in order to determine the duration and intensity of symptoms, their repercussion on the patient's functionality and to investigate the possibility of thoughts regarding self-harm or suicide. Questions must be asked on the patient's psychiatric history and the presence of any other symptoms related to episodes of mania or hypomania, since these could indicate the presence of bipolar affective disorder, which implies a greater risk of post-partum depression or psychosis.26
Questions recommended for investigating depression in pregnancy.
| 1. | During the past month, have you felt down, depressed or hopeless? |
| 2. | During the past month, have you often been bothered by having little interest or pleasure in doing things? |
| Ask the questions at any time during the interview, and if the patient answers “yes” to either one, ask her: have you felt you need or want help with this problem? | |
Source: Authors.
Depression in pregnancy has been documented as the most common cause of incapacity for work and also includes aspects such as deteriorating self-care and increased high-risk behaviours such as alcohol and tobacco use, as well as attempted suicide.10,27 The risk of preeclampsia is also increased, alongside a rise in the presentation of newborn complications, such as preterm labour, impaired foetal neurodevelopment, a low Apgar score and small for gestational age newborns.9,28,29
According to a study carried out by Michigan University, both women who had depression in pregnancy and their newborns had elevated corticotrophin, irregular sleeping patterns, greater irritability, reduced facial expressions and a greater risk of insecure attachment.30 Moreover, elevated levels of angiotensin II, vasopressin and oxytocin have been recorded, which are linked to a greater probability of preterm labour.10
In a study conducted by Field et al. in 2004, significantly raised cortisol levels were found in the group of pregnant women with a major depressive episode compared to the control group (343.7 versus 263.7nmol/l, respectively). The cortisol levels of newborns to women with the condition were also studied, and elevated concentrations were found in the exposed group (549.7 versus 408.8nmol/l), which can be explained by the fact that 40% of the hormone crosses the placental barrier. It should be noted that raised cortisol is associated with a greater risk of prematurity.31
The secretion of substances that may enhance vasoconstriction elevates the risk of hypertension and, with it, vascular changes that may induce preeclampsia.32 In a study performed on 623 healthy pregnant women, depression was associated with the onset of preeclampsia (odds ratio [OR]=2.5) in patients with a Beck Depression Inventory score of 3–17.33
According to Lartigue et al.,34 children of depressed mothers who did not form an adequate bond had a greater probability of excessive crying and irritability. School-age children of mothers who suffered depression in pregnancy have a greater tendency towards aggressive behaviour and learning difficulties. Early diagnosis and adequate treatment of depression in pregnancy will enable the newborn's adequate development and a secure bond to be formed.
TreatmentThere are two possible treatments for depression in pregnancy: psychotherapy and pharmacotherapy with antidepressants. In case of mild depression, psychotherapy is the first-line treatment, although it should be noted that this will be of little benefit for moderate or severe symptoms. Pharmacotherapy, on the other hand, is indicated as first-line treatment for moderate to severe major depressive disorder in pregnancy, but a number of weeks to months of ongoing pharmacological treatment are needed in order to counteract depressive symptoms.35
Psychotherapy and alternative therapiesReducing perinatal stress is a vital objective in public health promotion and prevention. Maternal anxiety, depression and stress lead to the aforementioned complications for foetal and maternal well-being, so treatment for the disease must be effective.1,9
Psychological interventions by healthcare personnel, such as psychotherapy, have demonstrated significant efficacy in treating depression in pregnancy in low- and middle-income countries.9 The importance of psychotherapy interventions has been described, given their positive impact on foetal and maternal well-being and the family environment. During work sessions, social problems such as intra-family violence, substance abuse by the pregnant woman or her family, and venereal diseases like HIV should be addressed, always with a view to achieving greater female empowerment in this regard. Moreover, two pillars of work have been proposed: providing the patient and family with comprehensive information and building new skills.36
Interventions that include ‘mindfulness’ for the prevention and treatment of mental health problems such as this are novel. Kabat-Zinn37 defines mindfulness as “the awareness that arises from paying attention, on purpose, in the present moment and non-judgmentally”. Among participants, it encourages the identification of negative moments so they can become better at tolerating them; mindfulness promotes a cognitive change in relation to each thought and provides cognitive experiences that enable the development and course of ideas that come to mind to be understood.
Although this tool is still unknown by many, one complete and published study by the Royal Women's Hospital (Australia) enrolled 52 pregnant women and introduced a mindfulness programme called “MindBabyBody”, where group sessions, both in-person and through independent work done at home, served as a treatment option for pregnant women with high levels of stress, anxiety or depression in any stage of pregnancy. The patients found motivations based on learning the new tool, actively taking part in their treatment and teaching and sharing the technique with their families. A high degree of acceptance was observed regarding the technique, with improvements to the quality of life, interpersonal relationships and confidence of the study participants.38
Various studies have also highlighted the role of exercise in the treatment of depression in pregnancy, since it helps to both lower cardiovascular risk and improve mood. Although the mechanisms of this anti-depressive effect are unknown, it is believed to positively alter neuroendocrine functions and the production of neurotransmitters.39 Likewise, among the recommendations made by the American College of Obstetricians and Gynaecologists for treating depression, all pregnant women with no medical contraindications impeding it should perform regular aerobic exercise during the perinatal period.26 Practising aerobic exercise has been proven to significantly reduce the severity of depressive symptoms, so it is therefore recommended for as long as it is practicable.40 Studies that assess the impact of other meditation techniques such as yoga or performing massages have revealed that these practices could prove beneficial for patients with this disease. However, the evidence is not as strong, so more studies are needed.39–42
Pharmacological treatment with antidepressantsThe number of pregnant women prescribed antidepressants has increased drastically over the past two decades.8 Thus, choosing a quick and effective treatment with no adverse effects for the mother or baby is a priority in the context of medical care. There are no randomised controlled clinical trials which shed light on the safety or efficacy of antidepressant use in pregnancy. However, through retrospective and prospective cohort or case–control studies, evidence has been uncovered regarding pharmacological treatment.43,44
Included in the possible arsenal of drugs used to treat depression in pregnancy are tricyclic antidepressants, selective serotonin reuptake inhibitors (SSRIs) and norepinephrine reuptake inhibitors (NRIs), also known as dual serotonin and norepinephrine reuptake inhibitors (SNRIs). Unfortunately, since there is no treatment option for depression in pregnancy without a risk of teratogenicity, the family of antidepressants with the most evidence is the most recommended: SSRIs.2,41
Tricyclic antidepressants have been available since 1950, when this family of psychotropics was the first-line treatment. Today, however, they are used less, having been replaced by more tolerable drugs such as SSRIs and SNRIs.45 Due to their lipophilic characteristics, up to 60% of the tricyclic antidepressant dose given to the mother has been shown to cross the placenta and they have been linked to heart malformations such as septal defects,5,45 although these have also been seen with exposure to sertraline.46
As regards SSRIs, while the population risk of major congenital malformations stands at around 2–4%, different meta-analyses have found a strong link between the use of SSRIs such as paroxetine and congenital heart defects (hence it not being recommended in pregnancy),47 as well as between citalopram and increased urinary and digestive anomalies. An increased risk of central nervous system abnormalities has also been described for neonates exposed to tricyclic antidepressants and SSRIs simultaneously.46–48 Nevertheless, Wichman et al. reported in 2009 that, in light of treatment with SSRIs or SNRIs such as venlafaxine, no significant increase in heart defects occurs.49 In multiple studies with representative samples, fluoxetine has been shown not to be associated with defects of the heart or other systems; it is therefore recommended as the first-choice drug for treating depression in pregnancy.50
Bearing in mind the importance of serotonin's role as a modulator in respiratory control, its inhibitory effect on the latter and vasoconstrictive action, it has been suggested that the various studies and case reports published on clinical pictures consisting of respiratory acidosis, cyanosis, tachypnoea, work of breathing and pulmonary hypertension secondary to SSRI exposure in pregnancy could be related to this family of drugs due to their pharmacodynamics.51,52 In a meta-analysis conducted by Grigoriadis et al.53 in Canada, it was identified that the risk of the neonate suffering pulmonary hypertension following the use of SSRIs only occurs when these medicines are administered in the third trimester of pregnancy, and not during the first few months.
“Poor neonatal adaptation syndrome” has also been discussed, which is described in around 10–30% of newborns to mothers treated with SSRIs during pregnancy, manifesting approximately two weeks after birth. This syndrome is characterised by irritability, a weak or absent cry, hypoglycaemia, tachypnoea and, on some occasions, seizures; among the physiopathological mechanisms of this syndrome, the possibility of it owing to the effects of abstinence, drug toxicity and changes in brain function has been considered.26
With respect to SNRIs, although few studies have been published, an association has been found between the use of venlafaxine in the first trimester of pregnancy and the presence of malformations such as anencephaly, gastroschisis and cleft palate. A link has also been found between the use of bupropion and some foetal malformations, such as septal heart defects, coarctation of the aorta and hypoplastic left heart syndrome. However, based on the benefit–risk assessment, using bupropion to treat nicotine dependence is beneficial if it prevents serious nicotine-derived complications in the unborn child.10,50
Electroconvulsive therapyElectroconvulsive therapy has been used in patients with serious conditions, treatment resistance, catatonia, high suicide risk and a tendency towards undernutrition. However, according to the trimester in which it is used, there are different chances of certain complications, such as foetal bradycardia, vaginal bleeding and pyloric stenosis in the first trimester. In a study where electroconvulsive therapy was used on 169 pregnant women, 53% had it in the second trimester, which is the most common gestational age for said treatment, although a total of 67 complications were noted, including preterm labour. It should be taken into account that electroconvulsive therapy is the last treatment to be chosen, although in cases of severe refractory depression it is used as the primary treatment.54–56
In recent years, the technique has been documented as safe and effective in the third trimester for both mother and baby; risks are avoided by monitoring hypoxia during the procedure. Electroconvulsive therapy has been used for approximately 50 years due to the need for an effective treatment and to reduce psychotropic drugs.56
ConclusionsDepression in pregnancy is a common disorder in our field, but it is underreported due to similarities between symptoms of pregnancy—such as tiredness, fatigue, irritability and changes in appetite and sleeping patterns—and the manifestations of a depressive disorder. Said underreporting means it is not treated promptly and foetal and maternal well-being is put at risk. Knowing the diagnostic criteria for depression and implementing the quick investigation methods recommended by international bodies are fundamental for early detection and the implementation of appropriate treatment.
Quick and effective treatment allows the main consequences of depression on the course of the pregnancy and obstetric and perinatal outcomes, such as preterm labour, impaired foetal neurodevelopment, a low Apgar score and low birth weight, among others, to be prevented. With respect to the non-pharmacological treatment of depression, it is important to highlight the efficacy of psychotherapy in mild cases of the disease. Mindfulness is considered a valuable tool among the therapeutic possibilities for pregnant women experiencing problems related to stress, anxiety or depression.
As regards treating depression in pregnancy, it is imperative to adhere to treatment options that are the safest and most in line with the mother's clinical picture. The recommendation of general measures should be borne in mind, using lower-risk antidepressants and applying electroconvulsive therapy when merited by the mother's condition, especially in more severe cases. Timely diagnosis and adequate treatment may reduce the impact depression has on the course of the pregnancy and foetal neurodevelopment, as well as on perinatal outcomes in general.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Martínez-Paredes JF, Jácome-Pérez N. Depresión en el embarazo. Rev Colomb Psiquiat. 2019;48:58–65.