The association of nervous system with skin is well documented. Many common psychiatric disorders can involve skin either directly or indirectly. We found an association of 13 primary psychiatric disorders leading to dermatological diseases, with association of 2 of 13 considered to be idiopathic. Association of the mind and body has long been studied. Several skin problems lead to psychological and psychiatric symptoms, however not all skin problems lead to psychiatric symptoms. On the contrary, many primary psychiatric illnesses appear to have associated skin disorders.
La asociación del sistema nervioso con la piel está bien documentada. Muchos trastornos psiquiátricos comunes pueden implicar a la piel directa o indirectamente. Se encontró asociación de 13 trastornos psiquiátricos primarios que llevan a enfermedades dermatológicas, y de las 13, asociación de 2 consideradas idiopáticas. La asociación entre la mente y el cuerpo se ha estudiado durante mucho tiempo. Varios problemas de la piel conducen a los síntomas psicológicos y psiquiátricos, pero no todos los problemas llevan a síntomas psiquiátricos de la piel. Por el contrario, parece que muchas enfermedades psiquiátricas primarias se asocian con trastornos de la piel.
Skin and nervous system develop alongside each other in the fetus and remain interconnected throughout life.1 Several mechanisms have been described concerning the possible mind and skin connections.2–5 Many dermatologic patients are treated effectively by including consideration of psychological factors.6 Moreover, psychiatric diseases have been found associated with dermatological problems and vice versa. However, whether psychiatric diseases cause dermatological diseases or dermatological diseases cause psychiatric diseases remains a dilemma and topic of study. Although it seems that psychiatric diseases are totally different from somatic diseases and have no connection with one another, a thorough study and modern research proves a deep association between psychiatry and dermatology.7–9
Skin disorders may be associated with certain psychotic disorders. In addition, 30 to 60% of patients with skin diseases have some type of psychiatric problem.10,11 Connection of dermatological problems with almost all major types of psychiatric and psychological disorders has also been documented.1 Some psychiatric diseases have less and some have more connection with dermatological disease. Percentages and rates of skin diseases in the psychiatric patients vary according to different authors, however all those authors agree that psychiatry and dermatology go hand in hand and this has resulted in the formation of the psycho-dermatology subspecialty.12–14
While there is no single universally accepted classification system of psychocutaneous disorders, the most widely accepted system classifies them as: a) psychophysiologic disorders; b) psychiatric disorders with dermatologic symptoms, and c) dermatologic disorders with psychiatric symptoms. Several other conditions of interest can be grouped under a heading of miscellaneous, and medication side effects of both psychotropic and dermatologic drugs should also be considered.15,16
Association of psychiatric disorders with dermatological diseases is well documented: depressive disorders including major depression, anxiety disorders including phobias, psychosis like schizophrenia, substance abuse disorders, personality disorders, bipolar disorders, dissociative personality disorders, obsessive compulsive disorders and other child psychiatric diseases are also found associated with many dermatological diseases. There is a prevalent belief that psychiatric diseases ultimately may lead to skin problems. The association is so amazing that various psychotropic medications lead to dermatological side effects.17
Various articles describe skin diseases caused by the psychiatric illnesses and significant associations have been found. Although both dermatological and psychiatric illnesses have been associated with one another, this article focuses on the theme of primary psychiatric diseases associated with and/or leading to dermatological problems.
The Association of Psychiatric Disorders with the Dermatological DiseasesAnxiety and StressAssociation of anxiety, acute or chronic, with skin has well been documented.18 Psychological states of anxiety, fear and shame have been indicated by blushing, hair-rising, growing pale, itching or hyperhidrosis.19 Anxiety has potential to impair the protective outer layer of the skin, causing the skin to be more sensitive and more easily penetrated. Moreover, it also is known to make an already existed skin problem worse. According to Seyhen et al.,20 at least 13% of dermatology patients have an anxiety disorder. Anxiety besides making the skin more sensitive and penetrative doesn’t cause any skin disease by itself but it actually worsens an already existed skin problem due to the stress.16,21 Therefore, anxiety indirectly triggers or exacerbates the skin disorder.
Anxiety → Stress → Inflammatory reactions in skinIt is possible to develop a skin rash from anxiety, it can also cause urticaria and other kinds of lesions and trigger a flare-up of herpes simplex. Several skin diseases have been reported to be exacerbated or triggered by stress, such as psoriasis, eczema, acne and herpes simplex. It also makes it harder for many skin diseases to heal. Mechanisms by which stress influences the skin is not entirely understood, however neuroimmune mechanisms have been described which relate the association of vasoactive neuropeptides, lymphokines and other chemical mediators.22,23,21,24,25 How stress aggravates skin damage has been previously studied. It is believed that the autonomic nervous system and hypothalamic-pituitary-adrenal (HPA) axis are activated in stressful conditions that cause helper T cells to release hormones and neuropeptides. Hence releasing neurotransmitters that ultimately lead to vascular instability in dermatitis patients.26
TSPO is studied in relation to body stress systems. These body stress systems (the hypothalamic-pituitary adrenal axis, the sympathetic nervous system, the renin-angiotensin axis, and the neuroendocrine-immune axis) are regulated by TSPO.27 TSPO is studied in human as well as animals.28 Any changes in TSPO expression could point towards an ongoing stress in the body.
STAI and translocator protein (18kDa) (TSPO), formerly known as the peripheral-type benzodiazepine receptor, are stress and anxiety biomarkers. The STAI and TSPO expression suggest that patients with Atopic dermatitis AD are under stress. How stress causes atopic dermatitis was studied by Kaga et al. Their study provides evidence on how stress and anxiety can lead to skin damage. In this particular study stress was studied in relation to atopic dermatitis. How stress can cause other dermatological problems is not well known, and the future studies will unmask this mechanism.
Kaga et al.29 studied TPSO in patients with atopic dermatitis in a recent study. The selected 52 patients with AD (30 male and 22 female) and 163 healthy volunteers (89 male and 74 female) for this purpose. The findings indicated that State-Trait Anxiety Inventory (STAI) scores remarkably increases AD male patients as compared to healthy participants. Moreover, the platelet TSPO expression was also remarkably augmented in the AD patients, supporting the notion that AD is stress responsive.
Furthermore, a single nucleotide polymorphism of the human TSPO gene at exon 4 (485G>A) (associated with stress sensitivity), showed significant reduced frequencies of GG and increased frequencies of GA in AD patients than healthy participants. This was done in genomic analysis using lymphocytes. The study concluded that variation in the TSPO gene affects susceptibility to AD.29
Furthermore, it has also been suggested that acute stress affecting atopic dermatitis patients can further aggravate the anxiety in these patients. This ultimately increases Th2-type responses due to dysregulation of the neuroimmune system, hence aggravating of allergic symptoms. The itching is relieved by anxiolytics and anti-depressants.30
In addition to the above mentioned alterations in skin, excessive hair growth is also caused by anxiety.31
PhobiasMany people have phobias about dirt, bacteria and cancer of skin. Therefore, repeated hand washing, cleaning hands and self-mutilation of skin due to an attempt to remove pigmented nevi that these patients assume to be a skin cancer is commonly observed in these patients. This can further lead to irritant dermatitis.32
DysmorphophobiaDysmorphophobia, or body dysmorphic disorder, is also known as dermatological non-disease. Patients perceive symptoms but lack signs of any disease. Face, scalp and genitals are three common areas of complaints and concern. Symptoms include feelings of excessive redness, scarring, large pores, blushing, facial hair and protruding or sunken parts of face. Hair loss, red scrotum, and herpes are other dermatological complains brought to the dermatological clinic by these patients.33,34
Psychosis and Psychotic DisordersPatients with some psychotic disorders may complain of itch in various body parts. Tactile hallucinations can be felt in schizophrenia and present as burning, tingling or itchy sensation or feelings of being touched.35
Moreover the association of skin with psychosis could be understood in depth by some useful studies regarding skin, psychosis and niacin also known as nicotinic acid (the niacin skin phenomenon indicates an edema reaction and prostaglandin [PG] mediated flush; because the PG metabolism is associated with the breakdown of membrane lipids, reduced niacin sensitivity shows disturbance in membrane phospholipid-arachidonic acid-PG pathways). These studies indicated that 23% up to 90% of schizophrenic patients have a reduced flush reaction as compared to the non-schizophrenic people.36–41 Moreover, niacin sensitivity reduced in the first-episode than in multi-episode schizophrenia patients.42
In another study, Berger et al.43 studied the nicotinic acid skin sensitivity (marker of disturbed prostaglandin metabolism), in the first episode psychosis and ultra-high risk (UHR) patients for psychosis. Niacin sensitivity was remarkably augmented in UHR group as compared to the healthy control group, while there was no difference between the UHR-T and UHR-NT groups. Niacin sensitivity was reduced in comparison to HC group. Niacin sensitivity was found to be inversely correlated with omega-6 and -9 fatty acids (FA) in UHR group. However, positively with phospholipase A2 (inPLA2) activity which is a membrane lipid repair/remodeling. High sensitivity of nicotinic acid in UHR group points towards an imbalance of omega-6/9 FA and eicosanoids at a membrane level. Overall findings of the study indicated that UHR group has increased niacin sensitivity (which could be considered as a pro-inflammatory state) as compared to the patients actually suffering from schizophrenia. It is also a reflection of higher demand for omega-6- and omega-9 FA and of an up-regulated membrane turnover of FA.43
The association of skin with psychosis needs more understanding, considering the above mentioned studies and the results. More so in other kinds of skin problems such as dermatitis artefacta and which has been described as a symptom of schizophrenia44 and major self-mutilation which has been described as the first symptom of the first psychotic episode.45 Furthermore, temperature sensitivity is also decreased in schizophrenia.46
Delusional DisorderAccording to DSM-V, any kind of bizarre or non-bizarre false belief concludes the diagnosis of delusional disorder. Many delusional patients have delusions about skin diseases. Previous classification of psycho dermatological problems classifies delusions of parasitosis as a primary psychiatric disorder causing dermatological problems. This delusion of parasitosis is a form of monosymptomatic hypochondrial psychosis. Patients experience formication (derived from the Latin word formica, meaning “ant”), a sensation of insect crawling over or under the skin.47 These patients firmly believe that some kind of parasite is the cause. It is sometimes associated with other psychiatric or medical disorders48 or due to the usage of some drugs.49 Complaints of itch and scratch and the classic “match box sign” or “baggie sign”, in which patients bring bits of skin and assumed parasites and pathogens in small containers as evidence of parasites are fairly common.50 Types of delusions observed in dermatology patients include delusions of parasitosis, olfactory reference syndrome (delusion of body odor which may be associated with olfactory hallucinations), delusions of fibers in skin (Morgellons), hypochondriacal delusions and delusional dysmorphophobia. However, delusion of parasitosis is the most frequent delusional disorder that is presented to dermatologists.51 Previously, delusions of bizarre nature used to raise concerns about the possibility of schizophrenia, however the emergence of DSM-V in May 2013 states a new criteria for the diagnosis of delusional disorder, therefore any kind of delusion, bizarre or non-bizarre, suggests a diagnoses of delusional disorder.
Major DepressionCurrently, modern recognized classification classifies trichotillomania and neurotic excoriations as primary psychiatric disorders causing dermatological problems. However, our review suggests that primary depression leads to acts of self-harm to the skin like scratching, picking (neurotic excoriations), digging, bumping, cutting, pulling, tearing or harming skin, hair (trichotillomania) or nails.52–54 The majority of patients who have self-inflicted dermatoses such as neurotic excoriations suffer from depression with somatization.55 Seyhan et al.20 (2006) also showed that 32% of dermatology patients had depression. Moreover, excessive hair growth is also found to be linked with major depression.31
Depression is also found to be associated with an increased risk of psoriasis. In fact depression may be independently associated with the risk of psoriasis.56 An interesting fact about depression and psoriasis is that the both complement each other. Depression can lead to psoriasis and psoriasis can lead to depression as well through an inflammatory mechanism.57,58
Depression has symptoms such as low mood, easy fatigability, anhedonia, sleep disturbance, excessive guilt, psychomotor agitation or retardation and recurrent thoughts of death with or without suicide ideation. Some of these can have adverse impact on existing dermatological problems. For example, sleep difficulties may complicate symptoms like pruritus. Psychomotor agitation experienced by some patients can be associated with rubbing, scratching or picking of the skin.59 However, this review suggests that there is still some evidence that depression can lead to skin damage through inflammation. The inflammatory cytokines such as tumor necrosis factor alpha (TNFα), interleukin (IL) 1, IL-2, IL-10, interferon gamma (IFNγ), IL-1ß, prostaglandin E2 (PGE2), C-reactive protein (CRP), IL-6, and IL-8 are involved in the pathogenesis of psoriasis as well as major depression. This suggests a possible connection between the two conditions.60 Moreover, genetic variations of the serotonergic system have been studied that play an integral role in the pathophysiological mechanism in depressed psoriatic patients.60
Somatic Symptoms and Related DisordersAccording to DSM-V, somatoform disorder is now called somatic symptoms and related disorders. It is defined as somatic symptoms that are either very distressing or result in significant disruption of functioning, as well as excessive abnormal thoughts, feelings and behaviors regarding those symptoms.61 Dermatological symptoms that can also be seen in patients of somatic symptoms and related disorders are localized or generalized somatoform itching, cutaneous dyestheisas in the form of trichodynia or glossodynia and hyperhidrosis.62
Impulse Control DisorderPatients of impulse control disorder are frequently seen in dermatology clinics. These patients come with acne excoriee (picking acne), neurodermatitis, dermatophagia and trichotillomania. Measures like cognitive behavioral therapy, hypnosis, and self-hypnosis have been shown useful. Current common classification of psycho dermatology doesn’t place impulse control disorder as the primary psychiatric condition causing dermatological problems. However, we suggest categorizing these dermatological problems under impulse control disorder and dermatophagia in OCD and impulse control disorder.63–78
Obsessive Compulsive DisorderOCD can be considered as a primary psychiatric condition which causes dermatological problems. Approximately 5% of dermatology patients have been found to be diagnosed with OCD.21 Acne excoriee and trichotillomania, behaviors of impulse control disorder, can also be classified under OCD because some patients who pick their acne are primarily obsessive compulsive in their picking.63 Another condition, onychotillomania (compulsive self-induced damage to nails) may also be a form of OCD.79 Similarly, neurodermatitis may also be a form of OCD,55 and several patients become victims of stigmatization.80,81 Other common symptoms of OCD causing skin damage are compulsive pulling of scalp, eyebrow, or eyelash hair; biting of the nails and lips, tongue, and cheeks; and excessive hand washing. However, the most common sites involved were face, back, and neck.82 Success of SSRI and cognitive behavioral therapy against these kinds of skin damaging behaviors points towards OCD being the primary cause of these dermatological conditions.83
Eating DisordersEating disorders like bulimia and anorexia nervosa can cause skin changes. Starvation, malnutrition, self-induced vomiting and use of drugs are usually the cause of skin problems in the patients of eating disorders. Some skin signs and symptoms seen in eating disorders are acrocyanosis, gingivitis, lanugo-like body hair, hard calluses, onychophagia, generalized pruritis, hyperpigmentation, poor wound healing, cheilitis, seborrhic dermatitis, acquired pili torti, alopecia, Russell's sign, carotenoderma, Sjögren syndrome like changes, brittle nails and hair, periungal erythema, melasma, steatotic skin, hypertrichosis, striae distesae, and dry scalp hair.84–90
Factitious DisorderDermatitis artefacta is a form of factitious disorder, in which the patient deliberately damages the skin but denies doing it. This condition is more prevalent in woman (3:1 to 20:1).91 Usually theses skin lesions are bilaterally symmetrical with sharp or angular borders. They may also present as burn scars blisters, ulcers and purpura, with or without erythema. Rubbing, picking, scratching, cutting, punching, sucking, biting, applying heat and chemicals can lead to this type of peculiar skin damage. Injecting feces, blood, or other substances is also rarely done. Associated conditions are borderline personality disorder, OCD, depression, and psychosis.92,93 Treatment is psychiatric in nature.94,95
Psychogenic PruritusPruritus in the absence of any skin pathology or an underlying medical disease can be classified as psychogenic pruritus.96,97 It is found associated with impulse control disorder, obsessive compulsive disorder or delusional disorder (delusions of parasitosis).98,99 It is sometimes difficult to tell if itching provokes the patient to scratch or whether the pruritus is a consequence of a compulsive scratching. Psychiatric medications have been proven to be useful against psychogenic pruritus.100,101
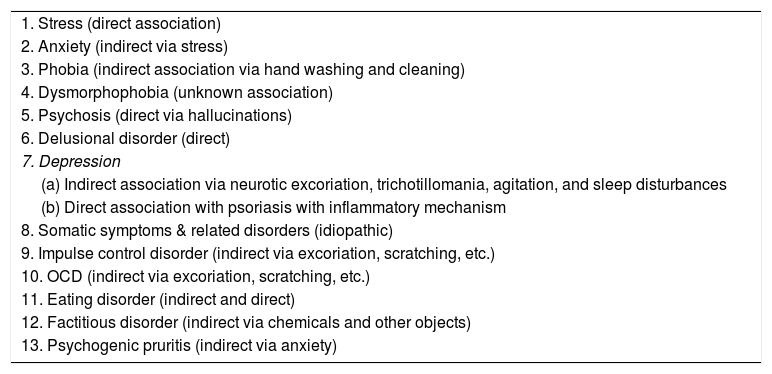
Current widely accepted classification includes psychogenic pruritus as a primary psychiatric disorder leading to dermatological problems. However, its association with anxiety has been reported.102 See Table 1 for the list of primary psychiatric disorders leading to dermatological problems.
Primary psychiatric disorders leading to dermatological problems.
| 1. Stress (direct association) |
| 2. Anxiety (indirect via stress) |
| 3. Phobia (indirect association via hand washing and cleaning) |
| 4. Dysmorphophobia (unknown association) |
| 5. Psychosis (direct via hallucinations) |
| 6. Delusional disorder (direct) |
| 7. Depression |
| (a) Indirect association via neurotic excoriation, trichotillomania, agitation, and sleep disturbances |
| (b) Direct association with psoriasis with inflammatory mechanism |
| 8. Somatic symptoms & related disorders (idiopathic) |
| 9. Impulse control disorder (indirect via excoriation, scratching, etc.) |
| 10. OCD (indirect via excoriation, scratching, etc.) |
| 11. Eating disorder (indirect and direct) |
| 12. Factitious disorder (indirect via chemicals and other objects) |
| 13. Psychogenic pruritis (indirect via anxiety) |
Interactions of the central nervous system occur with all human organs. Skin, being the largest organ of the body, is deeply linked with the brain. Various neurological diseases like neurofibromatosis express their signs on skin. In addition to neurological disorders, various psychiatric and psychological problems also cause some kind of dermatological symptoms. All major psychiatric diseases somehow either cause or are related to skin disorders or dermatological signs and symptoms. Some result from direct exacerbation like stress and some cause indirect like OCD. How these psychiatric disorders cause dermatological problems is a topic of debate and study. Much research has been going on to describe the exact mechanisms behind this association. Most patients in the dermatology clinic consider their problem as purely dermatologic in nature and many times refuse psychiatric evaluation. Many new clinicians are also unaware of the deep association of dermatologic disorders with psychiatric conditions.
Therefore, it is essential to educate patients and the doctors, psychiatrists and psychologists about the deep association of these two fields. Our study indicates that almost all common psychiatric diseases lead to dermatological problems. It is a common belief that diseases like dermatitis artefacta, delusions of parasitosis, trichotillomania and neurotic excoriations are primary dermatological diseases. However, our study reveals that these conditions are the result of certain preexisting psychiatric conditions like depression, anxiety, impulse control disorder, and OCD. Our findings are mentioned in Table 1.
The results of this comprehensive overview comprising of over more than 10 000 articles and research papers conclude that as of March 2016, there are 13 primary psychiatric conditions which lead to dermatological problems.
The psychiatric disorders which affect skin indirectly (which means that some psychiatric disorders lead to some symptoms/disorders which lead to skin damage. For example, anxiety first causes stress then stress ultimately damages skin. Anxiety itself doesn’t directly damage skin. Similarly, in OCD patients no neurochemical mechanism causes skin damage. In fact it is the manual skin picking which causes the dermatological symptoms. Psychiatric disorders that lead to skin damage indirectly are anxiety, phobia of dirt, depressive disorders, impulse control disorder, OCD, eating disorder by starvation and malnutrition, factitious disorder and psychogenic pruritus.
How depression is associated with psoriasis and somatic symptoms and related disorders association with skin remains idiopathic with its mechanisms poorly understood. However some evidence point toward an inflammatory mechanism in depression that leads to psoriasis.56 Moreover, how skin is affected in dysmorphobia is also not clearly understood. Whereas, 4 psychiatric disorders (stress, psychosis, major depression via inflammation, delusion, and few aspects of eating disorder with skin) are directly associated, where the psychiatric disorder itself causes skin damage. Thus, depression and eating disorders so far are the only psychiatric disorders that can damage the skin either directly or in directly.
ConclusionsIt is quite clear from the discussion above that the brain and skin are associated with each other. Skin and the human brain have common origin in the pre-embryonic life. Therefore, there is an association of dermatology with neurology, neurosciences and psychiatry. In this article, we focus solely on psychiatric disorders leading to dermatological diseases. This review describes the names of the psychiatric disorders linked with skin problems. Pathophysiology of many of these associations are clear, however association of some have not been known and remain a subject of debate amongst the scientists and the clinicians. Our comprehensive review suggests that the associations of 13 primary psychiatric diseases with dermatological diseases have been found. Five of 13 primary psychiatric disorders have direct association with skin disorders. By direct we mean that the psychiatric disorder causes dermatological disorder by itself, without any secondary cause. For example, stress causes skin problems by some neurochemical mechanisms. Similarly psychosis which has a symptom of hallucination produces tactile hallucinations. These symptoms are purely psychiatric in nature because cannot be visible to a clinician by a naked eye, therefore, we call this kind of association as direct association.
However, had there been a real physically visible skin damage due to scratching because of the hallucinations of itching, then we would have called it an indirect association of dermatological problems with psychiatric disorders. Likewise delusion of parasitosis itself is a primary psychiatric disorder with no secondary association; therefore, we attempt to call this as direct association. Furthermore, another group of psychiatric disorders classified as eating disorders can also cause skin damage. When malnutrition and starvation is the cause of skin symptoms, we attempt to relate this kind of dermatological association as Indirect (because anorexia/bulimia are itself psychiatric disorders in which patients attempt to vomit what they eat), as a result of these vomiting and avoidance of food the patients acquire skin problems probably due to protein/vitamin and other kinds of organic deficiencies. However, sometimes this vomiting can directly damage the skin near the mouth areas probably due to the acidity in the vomit. Therefore, we consider the association of eating disorders with skin damage as direct and indirect both.
We found that 8 psychiatric disorders have an indirect association with skin symptoms. For example, anxiety disorders can damage skin, however this damage is caused because first anxiety causes stress and then stress ultimately leads to skin problems. Likewise, phobia of dirt itself doesn’t generate a neurochemical mechanism to affect skin, it actually causes the person to wash and clean his hands again and again. Therefore, it's the hand washing which leads to skin damage, as we can see in the cases of major depression, where a depressed patient scratch or pick their own skin. It's not any neurochemical mechanism which damages the skin, in fact it is manual skin picking which damages the human skin. The same phenomenon of indirect skin damage is seen in OCD, psychogenic pruritus and impulse control disorder.
Somatic symptoms and related disorders, and dysmorphophobia affect skin, however their association is idiopathic. Therefore, we suggest further studies to strengthen our review findings and also to explore the mechanisms behind the disorder whose association with skin disorders is considered idiopathic or unknown.
Conflict of InterestsNone.
The authors are grateful for the help and support by Dr. Howard I. Maibach (UCSF).
Relevance of psychiatry in dermatology: Present concepts