The purpose of the present paper was to investigate the utilization of the Frontal Assessment Battery (FAB) as a selection tool for an effective evaluation of executive functions among human immunodeficiency virus (HIV)-positive patients. Data were collected from a group sample consisting of random HIV-positive patients being under treatment with combination antiretroviral therapy (cART) and a comparison group sample comprised by random healthy individuals to evaluate executive function via Frontal Assessment Battery (FAB), Montreal Cognitive Assessment (MoCA) and Mini-Mental State Examination (MMSE). MoCA served as a predictor for the FAB examination scores, while FAB exhibited the highest levels among three.
Since the discovery of the HIV, significant clinical and social progress has taken place. HIV prevention and treatment have progressed to a great extent, as the understanding of the structure and functions of the virus is still evolving. The introduction of cART has transformed HIV from a lethal disease into a chronic condition, but HIV-positive individuals are nevertheless affected, despite effective virus suppression, through HIV-Associated Neurocognitive Disorder (HAND).1 Neurocognitive impairment is one of the most common findings in HIV patients, sadly leading to high mortality rates.2 The incidence of HAND in HIV-1 infected individuals sadly remains a major problem still challenging the health and life quality of the corresponding patients, while the causation of brain dysfunction and cognitive impairment still remains unclear.
The clinical profile of HAND patients is mainly characterized by disorders in executive functions, memory, attention, reading and understanding, which resembles that of frontal lobe lesions.3 A relevant study by Dawes et al. in 2008 detected impairment in all executive-function models, thus indicating an association of HIV dementia with frontal lobe pathology.4 Furthermore, the executive functions that were found to be mostly affected by HAND were associated with the organization of the appropriate sequence of actions necessary for problem solving.5,6 The wide range of HIV-associated deficits and their assessment poses a challenge for modern neuropsychologists.7
HIV dementia was originally reported in 1986 by Navia et al., who identified a wide range of neuropsychological deficits as “the AIDS dementia complex” in 46 of 70 autopsied HIV patients.8 Thenceforth, several research studies, including longitudinal studies, have identified the existence of deficits in HIV patients.6,9,10 Criteria defined by the American National Institute of Health, known as the “Frascati Criteria,” are extensively utilized in clinical practice to classify the range of HIV-related dementia into 3 major subcategories: a) asymptomatic neurological damage (ANI); b) mild neurological disorder (MND), and c) HIV-associated hepatitis.11
Many disorders and lifestyle patterns have been linked to increased incidence of cognitive impairment among HIV patients. Cardiovascular disorders and diabetes in patients infected with the human immunodeficiency virus are among the strongest prognostic factors with regard to the impairment of cognitive function.12,13 Lifestyle factors such as smoking, drug abuse and alcohol consumption have also been reported to be widespread in HIV disease, as well as depressive symptoms, which may further exacerbate cognitive dysfunction.14 It can be, therefore, comprehended that clinical risk factors may affect cognitive functions both directly and indirectly by contributing to the onset of other medical conditions that can lead to cognitive decline (e.g., cardiovascular diseases contributing to vascular dementia).
In Greece, HAND patient evaluation is customarily conducted using the following tests: Montreal Cognitive Assessment (MoCA), HIV dementia scale, and Mini-Mental State Examination (MMSE). MoCA has been found to be a valuable clinical test to assess cognitive deficits in people with symptoms of dementia, while MMSE was argued not to be sensitive enough in the detection of such deficits.15,16 Since HAND presents with a cognitive profile similar to frontal lobe impairment, the authors aimed to investigate the utilization of the FAB as a selection tool for an effective evaluation of executive functions among HIV-positive patients.
Within the present study, the performance in the array of 3 examinations (MMSE, MoCA, and FAB) was evaluated in the following groups: a group sample consisted of random HIV patients being under treatment with cART and a comparison group sample comprised by random healthy individuals. The option of the aforementioned neuropsychological was based on their good psychometric properties and short amount of time required for their administration and evaluation.
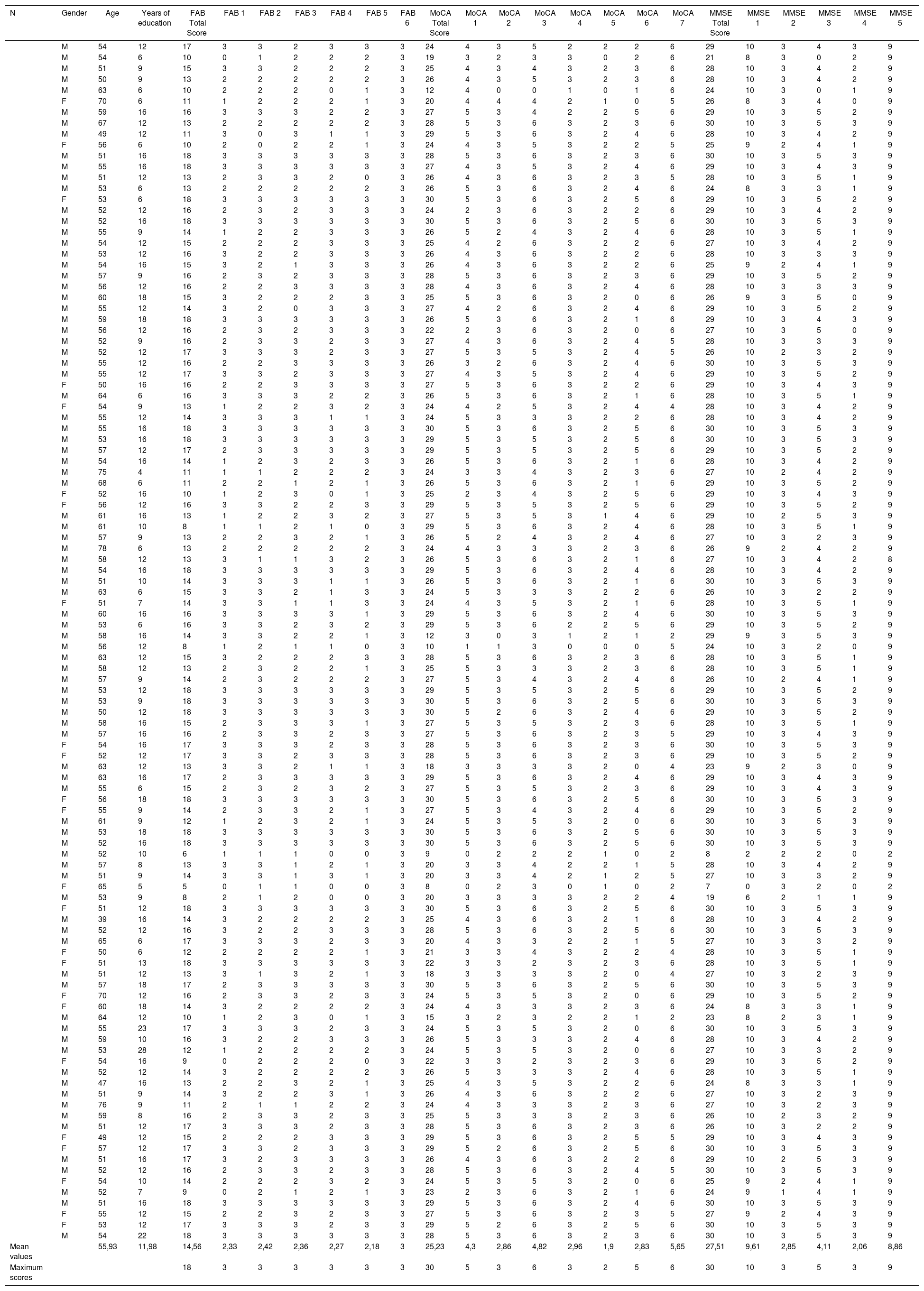
Data were collected from a group sample of 110 HIV-positive patients in the 1st University Neurology Department of AHEPA University General Hospital of Thessaloniki. The evaluation was performed prior to the administration of treatment to the participants. The study aimed to examine whether the Frontal Assessment Battery would be able to identify the potential decline in the executive functions of the subjects. All study participants gave written informed consent to participate in this study.
Among the 110 HIV-positive patients, 86 (78.2%) were males and 24 (21.8%) were females. Their age ranged from 39 to 78 years (mean, 55.95±6.04) and their educational status ranged from 4 to 28 (11.98±4.21) years of education.
The comparison group comprised 53 healthy individuals, among whom 31 (58.5%) were males and 22 (41.5%) were females. Their age ranged from 19 to 66 (48±8.27) years and their educational level ranged from 9 to 27 (14.35±4.02) years.
HIV patients consistently scored lower than the control group in the executive function tasks. Using the Pearson correlation coefficient (Pearson's r), correlations between the three neuropsychological examination results (MMSE, MoCA, and FAB) were evaluated, in pursuit of statistically significant correlations. FAB was found to correlate statistically significantly with the MoCA total assay (r=.68; P<.01) as well as with the assessment rating of the MoCA executive function sub-test (r=.6; P<.01). FAB was also found to correlate with the MMSE assay (r=.67; P<.01). By making a linear regression between MoCA, MMSE and FAB, MoCA test was found to be a predictor for the FAB assay (β=0.47; P<.01) — meaning that MoCA results may be able to prognosticate the Frontal Assessment Battery test scoring. Furthermore, MoCA could interpret 47% of the variance in the 2 overall scores (R2=0.47; P<.01). A different result was found, per contra, for the MMSE test. Comparing the FAB average scores between the patient group and the control group, there were statistically significant differences in the total scores of the 2 groups and in five of the 6 sub-assessments. In particular, the group of patients yielded a lower performance in the following sub-categories: Similarities, Verbal fluency, Programming, Contradictory instructions and Inhibitory control (P<.001). The ROC curve was used to estimate the sensitivity of FAB, MoCA and MMSE. The highest degree of sensitivity was found in FAB (0.755), followed by the MoCA test (0.615). The MMSE ROC curve analysis disclosed baseline results (0.52) (table 1).
Analytical table of patients in the examined group sample.
| N | Gender | Age | Years of education | FAB Total Score | FAB 1 | FAB 2 | FAB 3 | FAB 4 | FAB 5 | FAB 6 | MoCA Total Score | MoCA 1 | MoCA 2 | MoCA 3 | MoCA 4 | MoCA 5 | MoCA 6 | MoCA 7 | MMSE Total Score | MMSE 1 | MMSE 2 | MMSE 3 | MMSE 4 | MMSE 5 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | 54 | 12 | 17 | 3 | 3 | 2 | 3 | 3 | 3 | 24 | 4 | 3 | 5 | 2 | 2 | 2 | 6 | 29 | 10 | 3 | 4 | 3 | 9 | |
| M | 54 | 6 | 10 | 0 | 1 | 2 | 2 | 2 | 3 | 19 | 3 | 2 | 3 | 3 | 0 | 2 | 6 | 21 | 8 | 3 | 0 | 2 | 9 | |
| M | 51 | 9 | 15 | 3 | 3 | 2 | 2 | 2 | 3 | 25 | 4 | 3 | 4 | 3 | 2 | 3 | 6 | 28 | 10 | 3 | 4 | 2 | 9 | |
| M | 50 | 9 | 13 | 2 | 2 | 2 | 2 | 2 | 3 | 26 | 4 | 3 | 5 | 3 | 2 | 3 | 6 | 28 | 10 | 3 | 4 | 2 | 9 | |
| M | 63 | 6 | 10 | 2 | 2 | 2 | 0 | 1 | 3 | 12 | 4 | 0 | 0 | 1 | 0 | 1 | 6 | 24 | 10 | 3 | 0 | 1 | 9 | |
| F | 70 | 6 | 11 | 1 | 2 | 2 | 2 | 1 | 3 | 20 | 4 | 4 | 4 | 2 | 1 | 0 | 5 | 26 | 8 | 3 | 4 | 0 | 9 | |
| M | 59 | 16 | 16 | 3 | 3 | 3 | 2 | 2 | 3 | 27 | 5 | 3 | 4 | 2 | 2 | 5 | 6 | 29 | 10 | 3 | 5 | 2 | 9 | |
| M | 67 | 12 | 13 | 2 | 2 | 2 | 2 | 2 | 3 | 28 | 5 | 3 | 6 | 3 | 2 | 3 | 6 | 30 | 10 | 3 | 5 | 3 | 9 | |
| M | 49 | 12 | 11 | 3 | 0 | 3 | 1 | 1 | 3 | 29 | 5 | 3 | 6 | 3 | 2 | 4 | 6 | 28 | 10 | 3 | 4 | 2 | 9 | |
| F | 56 | 6 | 10 | 2 | 0 | 2 | 2 | 1 | 3 | 24 | 4 | 3 | 5 | 3 | 2 | 2 | 5 | 25 | 9 | 2 | 4 | 1 | 9 | |
| M | 51 | 16 | 18 | 3 | 3 | 3 | 3 | 3 | 3 | 28 | 5 | 3 | 6 | 3 | 2 | 3 | 6 | 30 | 10 | 3 | 5 | 3 | 9 | |
| M | 55 | 16 | 18 | 3 | 3 | 3 | 3 | 3 | 3 | 27 | 4 | 3 | 5 | 3 | 2 | 4 | 6 | 29 | 10 | 3 | 4 | 3 | 9 | |
| M | 51 | 12 | 13 | 2 | 3 | 3 | 2 | 0 | 3 | 26 | 4 | 3 | 6 | 3 | 2 | 3 | 5 | 28 | 10 | 3 | 5 | 1 | 9 | |
| M | 53 | 6 | 13 | 2 | 2 | 2 | 2 | 2 | 3 | 26 | 5 | 3 | 6 | 3 | 2 | 4 | 6 | 24 | 8 | 3 | 3 | 1 | 9 | |
| F | 53 | 6 | 18 | 3 | 3 | 3 | 3 | 3 | 3 | 30 | 5 | 3 | 6 | 3 | 2 | 5 | 6 | 29 | 10 | 3 | 5 | 2 | 9 | |
| M | 52 | 12 | 16 | 2 | 3 | 2 | 3 | 3 | 3 | 24 | 2 | 3 | 6 | 3 | 2 | 2 | 6 | 29 | 10 | 3 | 4 | 2 | 9 | |
| M | 52 | 16 | 18 | 3 | 3 | 3 | 3 | 3 | 3 | 30 | 5 | 3 | 6 | 3 | 2 | 5 | 6 | 30 | 10 | 3 | 5 | 3 | 9 | |
| M | 55 | 9 | 14 | 1 | 2 | 2 | 3 | 3 | 3 | 26 | 5 | 2 | 4 | 3 | 2 | 4 | 6 | 28 | 10 | 3 | 5 | 1 | 9 | |
| M | 54 | 12 | 15 | 2 | 2 | 2 | 3 | 3 | 3 | 25 | 4 | 2 | 6 | 3 | 2 | 2 | 6 | 27 | 10 | 3 | 4 | 2 | 9 | |
| M | 53 | 12 | 16 | 3 | 2 | 2 | 3 | 3 | 3 | 26 | 4 | 3 | 6 | 3 | 2 | 2 | 6 | 28 | 10 | 3 | 3 | 3 | 9 | |
| M | 54 | 16 | 15 | 3 | 2 | 1 | 3 | 3 | 3 | 26 | 4 | 3 | 6 | 3 | 2 | 2 | 6 | 25 | 9 | 2 | 4 | 1 | 9 | |
| M | 57 | 9 | 16 | 2 | 3 | 2 | 3 | 3 | 3 | 28 | 5 | 3 | 6 | 3 | 2 | 3 | 6 | 29 | 10 | 3 | 5 | 2 | 9 | |
| M | 56 | 12 | 16 | 2 | 2 | 3 | 3 | 3 | 3 | 28 | 4 | 3 | 6 | 3 | 2 | 4 | 6 | 28 | 10 | 3 | 3 | 3 | 9 | |
| M | 60 | 18 | 15 | 3 | 2 | 2 | 2 | 3 | 3 | 25 | 5 | 3 | 6 | 3 | 2 | 0 | 6 | 26 | 9 | 3 | 5 | 0 | 9 | |
| M | 55 | 12 | 14 | 3 | 2 | 0 | 3 | 3 | 3 | 27 | 4 | 2 | 6 | 3 | 2 | 4 | 6 | 29 | 10 | 3 | 5 | 2 | 9 | |
| M | 59 | 18 | 18 | 3 | 3 | 3 | 3 | 3 | 3 | 26 | 5 | 3 | 6 | 3 | 2 | 1 | 6 | 29 | 10 | 3 | 4 | 3 | 9 | |
| M | 56 | 12 | 16 | 2 | 3 | 2 | 3 | 3 | 3 | 22 | 2 | 3 | 6 | 3 | 2 | 0 | 6 | 27 | 10 | 3 | 5 | 0 | 9 | |
| M | 52 | 9 | 16 | 2 | 3 | 3 | 2 | 3 | 3 | 27 | 4 | 3 | 6 | 3 | 2 | 4 | 5 | 28 | 10 | 3 | 3 | 3 | 9 | |
| M | 52 | 12 | 17 | 3 | 3 | 3 | 2 | 3 | 3 | 27 | 5 | 3 | 5 | 3 | 2 | 4 | 5 | 26 | 10 | 2 | 3 | 2 | 9 | |
| M | 55 | 12 | 16 | 2 | 2 | 3 | 3 | 3 | 3 | 26 | 3 | 2 | 6 | 3 | 2 | 4 | 6 | 30 | 10 | 3 | 5 | 3 | 9 | |
| M | 55 | 12 | 17 | 3 | 3 | 2 | 3 | 3 | 3 | 27 | 4 | 3 | 5 | 3 | 2 | 4 | 6 | 29 | 10 | 3 | 5 | 2 | 9 | |
| F | 50 | 16 | 16 | 2 | 2 | 3 | 3 | 3 | 3 | 27 | 5 | 3 | 6 | 3 | 2 | 2 | 6 | 29 | 10 | 3 | 4 | 3 | 9 | |
| M | 64 | 6 | 16 | 3 | 3 | 3 | 2 | 2 | 3 | 26 | 5 | 3 | 6 | 3 | 2 | 1 | 6 | 28 | 10 | 3 | 5 | 1 | 9 | |
| F | 54 | 9 | 13 | 1 | 2 | 2 | 3 | 2 | 3 | 24 | 4 | 2 | 5 | 3 | 2 | 4 | 4 | 28 | 10 | 3 | 4 | 2 | 9 | |
| M | 55 | 12 | 14 | 3 | 3 | 3 | 1 | 1 | 3 | 24 | 5 | 3 | 3 | 3 | 2 | 2 | 6 | 28 | 10 | 3 | 4 | 2 | 9 | |
| M | 55 | 16 | 18 | 3 | 3 | 3 | 3 | 3 | 3 | 30 | 5 | 3 | 6 | 3 | 2 | 5 | 6 | 30 | 10 | 3 | 5 | 3 | 9 | |
| M | 53 | 16 | 18 | 3 | 3 | 3 | 3 | 3 | 3 | 29 | 5 | 3 | 5 | 3 | 2 | 5 | 6 | 30 | 10 | 3 | 5 | 3 | 9 | |
| M | 57 | 12 | 17 | 2 | 3 | 3 | 3 | 3 | 3 | 29 | 5 | 3 | 5 | 3 | 2 | 5 | 6 | 29 | 10 | 3 | 5 | 2 | 9 | |
| M | 54 | 16 | 14 | 1 | 2 | 3 | 2 | 3 | 3 | 26 | 5 | 3 | 6 | 3 | 2 | 1 | 6 | 28 | 10 | 3 | 4 | 2 | 9 | |
| M | 75 | 4 | 11 | 1 | 1 | 2 | 2 | 2 | 3 | 24 | 3 | 3 | 4 | 3 | 2 | 3 | 6 | 27 | 10 | 2 | 4 | 2 | 9 | |
| M | 68 | 6 | 11 | 2 | 2 | 1 | 2 | 1 | 3 | 26 | 5 | 3 | 6 | 3 | 2 | 1 | 6 | 29 | 10 | 3 | 5 | 2 | 9 | |
| F | 52 | 16 | 10 | 1 | 2 | 3 | 0 | 1 | 3 | 25 | 2 | 3 | 4 | 3 | 2 | 5 | 6 | 29 | 10 | 3 | 4 | 3 | 9 | |
| F | 56 | 12 | 16 | 3 | 3 | 2 | 2 | 3 | 3 | 29 | 5 | 3 | 5 | 3 | 2 | 5 | 6 | 29 | 10 | 3 | 5 | 2 | 9 | |
| M | 61 | 16 | 13 | 1 | 2 | 2 | 3 | 2 | 3 | 27 | 5 | 3 | 5 | 3 | 1 | 4 | 6 | 29 | 10 | 2 | 5 | 3 | 9 | |
| M | 61 | 10 | 8 | 1 | 1 | 2 | 1 | 0 | 3 | 29 | 5 | 3 | 6 | 3 | 2 | 4 | 6 | 28 | 10 | 3 | 5 | 1 | 9 | |
| M | 57 | 9 | 13 | 2 | 2 | 3 | 2 | 1 | 3 | 26 | 5 | 2 | 4 | 3 | 2 | 4 | 6 | 27 | 10 | 3 | 2 | 3 | 9 | |
| M | 78 | 6 | 13 | 2 | 2 | 2 | 2 | 2 | 3 | 24 | 4 | 3 | 3 | 3 | 2 | 3 | 6 | 26 | 9 | 2 | 4 | 2 | 9 | |
| M | 58 | 12 | 13 | 3 | 1 | 1 | 3 | 2 | 3 | 26 | 5 | 3 | 6 | 3 | 2 | 1 | 6 | 27 | 10 | 3 | 4 | 2 | 8 | |
| M | 54 | 16 | 18 | 3 | 3 | 3 | 3 | 3 | 3 | 29 | 5 | 3 | 6 | 3 | 2 | 4 | 6 | 28 | 10 | 3 | 4 | 2 | 9 | |
| M | 51 | 10 | 14 | 3 | 3 | 3 | 1 | 1 | 3 | 26 | 5 | 3 | 6 | 3 | 2 | 1 | 6 | 30 | 10 | 3 | 5 | 3 | 9 | |
| M | 63 | 6 | 15 | 3 | 3 | 2 | 1 | 3 | 3 | 24 | 5 | 3 | 3 | 3 | 2 | 2 | 6 | 26 | 10 | 3 | 2 | 2 | 9 | |
| F | 51 | 7 | 14 | 3 | 3 | 1 | 1 | 3 | 3 | 24 | 4 | 3 | 5 | 3 | 2 | 1 | 6 | 28 | 10 | 3 | 5 | 1 | 9 | |
| M | 60 | 16 | 16 | 3 | 3 | 3 | 3 | 1 | 3 | 29 | 5 | 3 | 6 | 3 | 2 | 4 | 6 | 30 | 10 | 3 | 5 | 3 | 9 | |
| M | 53 | 6 | 16 | 3 | 3 | 2 | 3 | 2 | 3 | 29 | 5 | 3 | 6 | 2 | 2 | 5 | 6 | 29 | 10 | 3 | 5 | 2 | 9 | |
| M | 58 | 16 | 14 | 3 | 3 | 2 | 2 | 1 | 3 | 12 | 3 | 0 | 3 | 1 | 2 | 1 | 2 | 29 | 9 | 3 | 5 | 3 | 9 | |
| M | 56 | 12 | 8 | 1 | 2 | 1 | 1 | 0 | 3 | 10 | 1 | 1 | 3 | 0 | 0 | 0 | 5 | 24 | 10 | 3 | 2 | 0 | 9 | |
| M | 63 | 12 | 15 | 3 | 2 | 2 | 2 | 3 | 3 | 28 | 5 | 3 | 6 | 3 | 2 | 3 | 6 | 28 | 10 | 3 | 5 | 1 | 9 | |
| M | 58 | 12 | 13 | 2 | 3 | 2 | 2 | 1 | 3 | 25 | 5 | 3 | 3 | 3 | 2 | 3 | 6 | 28 | 10 | 3 | 5 | 1 | 9 | |
| M | 57 | 9 | 14 | 2 | 3 | 2 | 2 | 2 | 3 | 27 | 5 | 3 | 4 | 3 | 2 | 4 | 6 | 26 | 10 | 2 | 4 | 1 | 9 | |
| M | 53 | 12 | 18 | 3 | 3 | 3 | 3 | 3 | 3 | 29 | 5 | 3 | 5 | 3 | 2 | 5 | 6 | 29 | 10 | 3 | 5 | 2 | 9 | |
| M | 53 | 9 | 18 | 3 | 3 | 3 | 3 | 3 | 3 | 30 | 5 | 3 | 6 | 3 | 2 | 5 | 6 | 30 | 10 | 3 | 5 | 3 | 9 | |
| M | 50 | 12 | 18 | 3 | 3 | 3 | 3 | 3 | 3 | 30 | 5 | 2 | 6 | 3 | 2 | 4 | 6 | 29 | 10 | 3 | 5 | 2 | 9 | |
| M | 58 | 16 | 15 | 2 | 3 | 3 | 3 | 1 | 3 | 27 | 5 | 3 | 5 | 3 | 2 | 3 | 6 | 28 | 10 | 3 | 5 | 1 | 9 | |
| M | 57 | 16 | 16 | 2 | 3 | 3 | 2 | 3 | 3 | 27 | 5 | 3 | 6 | 3 | 2 | 3 | 5 | 29 | 10 | 3 | 4 | 3 | 9 | |
| F | 54 | 16 | 17 | 3 | 3 | 3 | 2 | 3 | 3 | 28 | 5 | 3 | 6 | 3 | 2 | 3 | 6 | 30 | 10 | 3 | 5 | 3 | 9 | |
| F | 52 | 12 | 17 | 3 | 3 | 2 | 3 | 3 | 3 | 28 | 5 | 3 | 6 | 3 | 2 | 3 | 6 | 29 | 10 | 3 | 5 | 2 | 9 | |
| M | 63 | 12 | 13 | 3 | 3 | 2 | 1 | 1 | 3 | 18 | 3 | 3 | 3 | 3 | 2 | 0 | 4 | 23 | 9 | 2 | 3 | 0 | 9 | |
| M | 63 | 16 | 17 | 2 | 3 | 3 | 3 | 3 | 3 | 29 | 5 | 3 | 6 | 3 | 2 | 4 | 6 | 29 | 10 | 3 | 4 | 3 | 9 | |
| M | 55 | 6 | 15 | 2 | 3 | 2 | 3 | 2 | 3 | 27 | 5 | 3 | 5 | 3 | 2 | 3 | 6 | 29 | 10 | 3 | 4 | 3 | 9 | |
| F | 56 | 18 | 18 | 3 | 3 | 3 | 3 | 3 | 3 | 30 | 5 | 3 | 6 | 3 | 2 | 5 | 6 | 30 | 10 | 3 | 5 | 3 | 9 | |
| F | 55 | 9 | 14 | 2 | 3 | 3 | 2 | 1 | 3 | 27 | 5 | 3 | 4 | 3 | 2 | 4 | 6 | 29 | 10 | 3 | 5 | 2 | 9 | |
| M | 61 | 9 | 12 | 1 | 2 | 3 | 2 | 1 | 3 | 24 | 5 | 3 | 5 | 3 | 2 | 0 | 6 | 30 | 10 | 3 | 5 | 3 | 9 | |
| M | 53 | 18 | 18 | 3 | 3 | 3 | 3 | 3 | 3 | 30 | 5 | 3 | 6 | 3 | 2 | 5 | 6 | 30 | 10 | 3 | 5 | 3 | 9 | |
| M | 52 | 16 | 18 | 3 | 3 | 3 | 3 | 3 | 3 | 30 | 5 | 3 | 6 | 3 | 2 | 5 | 6 | 30 | 10 | 3 | 5 | 3 | 9 | |
| M | 52 | 10 | 6 | 1 | 1 | 1 | 0 | 0 | 3 | 9 | 0 | 2 | 2 | 2 | 1 | 0 | 2 | 8 | 2 | 2 | 2 | 0 | 2 | |
| M | 57 | 8 | 13 | 3 | 3 | 1 | 2 | 1 | 3 | 20 | 3 | 3 | 4 | 2 | 2 | 1 | 5 | 28 | 10 | 3 | 4 | 2 | 9 | |
| M | 51 | 9 | 14 | 3 | 3 | 1 | 3 | 1 | 3 | 20 | 3 | 3 | 4 | 2 | 1 | 2 | 5 | 27 | 10 | 3 | 3 | 2 | 9 | |
| F | 65 | 5 | 5 | 0 | 1 | 1 | 0 | 0 | 3 | 8 | 0 | 2 | 3 | 0 | 1 | 0 | 2 | 7 | 0 | 3 | 2 | 0 | 2 | |
| M | 53 | 9 | 8 | 2 | 1 | 2 | 0 | 0 | 3 | 20 | 3 | 3 | 3 | 3 | 2 | 2 | 4 | 19 | 6 | 2 | 1 | 1 | 9 | |
| F | 51 | 12 | 18 | 3 | 3 | 3 | 3 | 3 | 3 | 30 | 5 | 3 | 6 | 3 | 2 | 5 | 6 | 30 | 10 | 3 | 5 | 3 | 9 | |
| M | 39 | 16 | 14 | 3 | 2 | 2 | 2 | 2 | 3 | 25 | 4 | 3 | 6 | 3 | 2 | 1 | 6 | 28 | 10 | 3 | 4 | 2 | 9 | |
| M | 52 | 12 | 16 | 3 | 2 | 2 | 3 | 3 | 3 | 28 | 5 | 3 | 6 | 3 | 2 | 5 | 6 | 30 | 10 | 3 | 5 | 3 | 9 | |
| M | 65 | 6 | 17 | 3 | 3 | 3 | 2 | 3 | 3 | 20 | 4 | 3 | 3 | 2 | 2 | 1 | 5 | 27 | 10 | 3 | 3 | 2 | 9 | |
| F | 50 | 6 | 12 | 2 | 2 | 2 | 2 | 1 | 3 | 21 | 3 | 3 | 4 | 3 | 2 | 2 | 4 | 28 | 10 | 3 | 5 | 1 | 9 | |
| F | 51 | 13 | 18 | 3 | 3 | 3 | 3 | 3 | 3 | 22 | 3 | 3 | 2 | 3 | 2 | 3 | 6 | 28 | 10 | 3 | 5 | 1 | 9 | |
| M | 51 | 12 | 13 | 3 | 1 | 3 | 2 | 1 | 3 | 18 | 3 | 3 | 3 | 3 | 2 | 0 | 4 | 27 | 10 | 3 | 2 | 3 | 9 | |
| M | 57 | 18 | 17 | 2 | 3 | 3 | 3 | 3 | 3 | 30 | 5 | 3 | 6 | 3 | 2 | 5 | 6 | 30 | 10 | 3 | 5 | 3 | 9 | |
| F | 70 | 12 | 16 | 2 | 3 | 3 | 2 | 3 | 3 | 24 | 5 | 3 | 5 | 3 | 2 | 0 | 6 | 29 | 10 | 3 | 5 | 2 | 9 | |
| F | 60 | 18 | 14 | 3 | 2 | 2 | 2 | 2 | 3 | 24 | 4 | 3 | 3 | 3 | 2 | 3 | 6 | 24 | 8 | 3 | 3 | 1 | 9 | |
| M | 64 | 12 | 10 | 1 | 2 | 3 | 0 | 1 | 3 | 15 | 3 | 2 | 3 | 2 | 2 | 1 | 2 | 23 | 8 | 2 | 3 | 1 | 9 | |
| M | 55 | 23 | 17 | 3 | 3 | 3 | 2 | 3 | 3 | 24 | 5 | 3 | 5 | 3 | 2 | 0 | 6 | 30 | 10 | 3 | 5 | 3 | 9 | |
| M | 59 | 10 | 16 | 3 | 2 | 2 | 3 | 3 | 3 | 26 | 5 | 3 | 3 | 3 | 2 | 4 | 6 | 28 | 10 | 3 | 4 | 2 | 9 | |
| M | 53 | 28 | 12 | 1 | 2 | 2 | 2 | 2 | 3 | 24 | 5 | 3 | 5 | 3 | 2 | 0 | 6 | 27 | 10 | 3 | 3 | 2 | 9 | |
| F | 54 | 16 | 9 | 0 | 2 | 2 | 2 | 0 | 3 | 22 | 3 | 3 | 2 | 3 | 2 | 3 | 6 | 29 | 10 | 3 | 5 | 2 | 9 | |
| M | 52 | 12 | 14 | 3 | 2 | 2 | 2 | 2 | 3 | 26 | 5 | 3 | 3 | 3 | 2 | 4 | 6 | 28 | 10 | 3 | 5 | 1 | 9 | |
| M | 47 | 16 | 13 | 2 | 2 | 3 | 2 | 1 | 3 | 25 | 4 | 3 | 5 | 3 | 2 | 2 | 6 | 24 | 8 | 3 | 3 | 1 | 9 | |
| M | 51 | 9 | 14 | 3 | 2 | 2 | 3 | 1 | 3 | 26 | 4 | 3 | 6 | 3 | 2 | 2 | 6 | 27 | 10 | 3 | 2 | 3 | 9 | |
| M | 76 | 9 | 11 | 2 | 1 | 1 | 2 | 2 | 3 | 24 | 4 | 3 | 3 | 3 | 2 | 3 | 6 | 27 | 10 | 3 | 2 | 3 | 9 | |
| M | 59 | 8 | 16 | 2 | 3 | 3 | 2 | 3 | 3 | 25 | 5 | 3 | 3 | 3 | 2 | 3 | 6 | 26 | 10 | 2 | 3 | 2 | 9 | |
| M | 51 | 12 | 17 | 3 | 3 | 3 | 2 | 3 | 3 | 28 | 5 | 3 | 6 | 3 | 2 | 3 | 6 | 26 | 10 | 3 | 2 | 2 | 9 | |
| F | 49 | 12 | 15 | 2 | 2 | 2 | 3 | 3 | 3 | 29 | 5 | 3 | 6 | 3 | 2 | 5 | 5 | 29 | 10 | 3 | 4 | 3 | 9 | |
| F | 57 | 12 | 17 | 3 | 3 | 2 | 3 | 3 | 3 | 29 | 5 | 2 | 6 | 3 | 2 | 5 | 6 | 30 | 10 | 3 | 5 | 3 | 9 | |
| M | 51 | 16 | 17 | 3 | 2 | 3 | 3 | 3 | 3 | 26 | 4 | 3 | 6 | 3 | 2 | 2 | 6 | 29 | 10 | 2 | 5 | 3 | 9 | |
| M | 52 | 12 | 16 | 2 | 3 | 3 | 2 | 3 | 3 | 28 | 5 | 3 | 6 | 3 | 2 | 4 | 5 | 30 | 10 | 3 | 5 | 3 | 9 | |
| F | 54 | 10 | 14 | 2 | 2 | 2 | 3 | 2 | 3 | 24 | 5 | 3 | 5 | 3 | 2 | 0 | 6 | 25 | 9 | 2 | 4 | 1 | 9 | |
| M | 52 | 7 | 9 | 0 | 2 | 1 | 2 | 1 | 3 | 23 | 2 | 3 | 6 | 3 | 2 | 1 | 6 | 24 | 9 | 1 | 4 | 1 | 9 | |
| M | 51 | 16 | 18 | 3 | 3 | 3 | 3 | 3 | 3 | 29 | 5 | 3 | 6 | 3 | 2 | 4 | 6 | 30 | 10 | 3 | 5 | 3 | 9 | |
| F | 55 | 12 | 15 | 2 | 2 | 3 | 2 | 3 | 3 | 27 | 5 | 3 | 6 | 3 | 2 | 3 | 5 | 27 | 9 | 2 | 4 | 3 | 9 | |
| F | 53 | 12 | 17 | 3 | 3 | 3 | 2 | 3 | 3 | 29 | 5 | 2 | 6 | 3 | 2 | 5 | 6 | 30 | 10 | 3 | 5 | 3 | 9 | |
| M | 54 | 22 | 18 | 3 | 3 | 3 | 3 | 3 | 3 | 28 | 5 | 3 | 6 | 3 | 2 | 3 | 6 | 30 | 10 | 3 | 5 | 3 | 9 | |
| Mean values | 55,93 | 11,98 | 14,56 | 2,33 | 2,42 | 2,36 | 2,27 | 2,18 | 3 | 25,23 | 4,3 | 2,86 | 4,82 | 2,96 | 1,9 | 2,83 | 5,65 | 27,51 | 9,61 | 2,85 | 4,11 | 2,06 | 8,86 | |
| Maximum scores | 18 | 3 | 3 | 3 | 3 | 3 | 3 | 30 | 5 | 3 | 6 | 3 | 2 | 5 | 6 | 30 | 10 | 3 | 5 | 3 | 9 |
FAB 1: Similarities; FAB 2: Lexical fluency; FAB 3: Motor series – programming; FAB 4: Sensitivity to interference; FAB 5: Inhibitory control; FAB 6: Environmental autonomy. MoCA 1: Executive functions; MoCA 2: Naming; MoCA 3: Attention; MoCA 4: Language; MoCA 5: Abstraction; MoCA 6: Delayed recall; MoCA 7: Orientation. MMSE 1: Orientation; MMSE 2: Registration; MMSE 3: Attention; MMSE 4: Recall; MMSE 5: Language.
Combined antiretroviral therapy has helped patients in the battle against HIV, but clinical significance also lies in the evaluation of screening tools’ usage for the assessment of cognitive functions. Due to higher survival rates, the necessity for observation and evaluation of the concomitant long-term HIV-associated mental deficits pertain to the effectiveness assessment of HIV treatment. Emphasis should be given on the difficulties of the abovementioned procedure due specifically to the varying cognitive status of the patients under treatment, as cognitive impairment or cognitive recovery may occur. HIV infection is closely associated with disorders in executive functions, and namely, programming has been shown to be the most influenced cognitive parameter.
By comparing the two groups (HIV-positive patients and controls), significant differences were observed in the executive functions, confirming the authors’ initial hypothesis that the patient group would score lower in executive functions, despite the fact that they received treatment. Larger cognitive deficits were found in the cognitive parameters of programming, sensitivity to interference and suspension testing. There was no difference in the acceptability of environmental autonomy (reflexive behavior). Furthermore, the sensitivity of the 3 evaluation tools was investigated. Despite the fact that the frontal assessment battery exhibited the highest sensitivity score of 0.755, the authors do not consider it a stand-alone indicator in the identification of cognitive impairment in HIV-associated dementia, especially among patients undergoing treatment. The authors recommend the use of FAB along with the MoCA neuropsychological evaluation for the brief assessment of cognitive potential, as the FAB clearly measures the deterioration of executive functions in patients positive for the human immunodeficiency virus and serves as a valuable neuropsychological assessment tool. Given the varying nature of HIV patients’ cognitive profile, however, it has to be part of a wider battery of neuropsychological evaluation for HAND. The results are consistent with other recently conducted studies.17
FundingThis work has not been funded by any corporation.
Conflict of interestsThere are no potential conflicts of interest regarding this study.