The COVID-19 pandemic has increased the magnitude of mental illnesses such as depression, not only in the general population, but also in healthcare personnel. However, in Peru the prevalence, and the associated factors for developing depression in healthcare personnel, are not known. The objective was to determine the prevalence and identify the factors associated with depression in healthcare personnel, in the context of the SARS-CoV-2 pandemic.
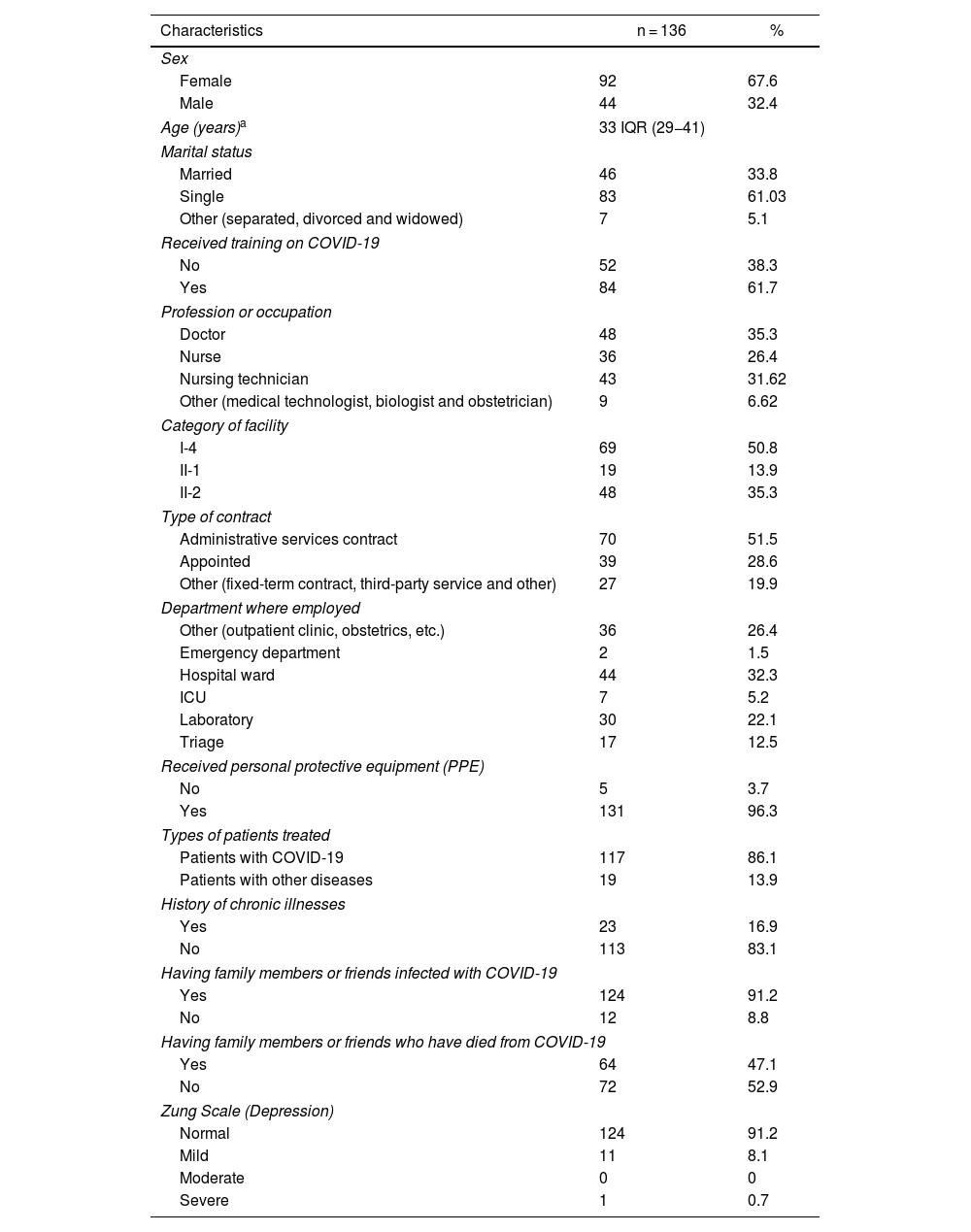
MethodsAn analytical cross-sectional study was carried out from May to September in healthcare establishments. A sample of 136 health workers were included and a survey was applied to collect the data. Depression as a dependent variable was measured using the Zung self-report scale. To identify the associated factors, the bivariate and multivariate analysis was performed by logistic regression with STATA v 14.
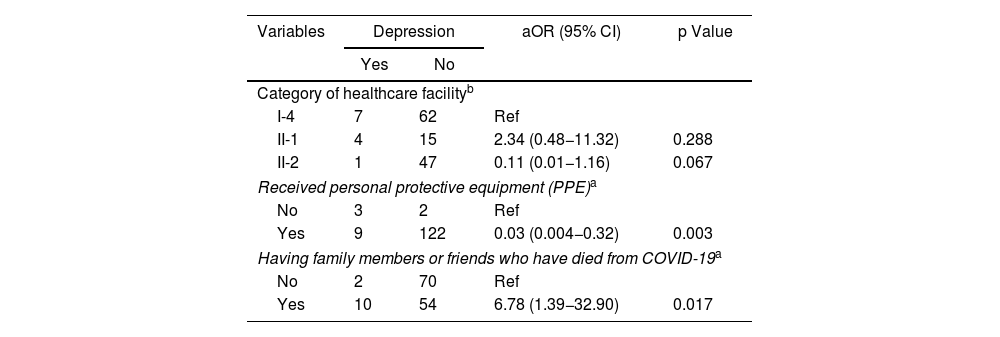
ResultsThe prevalence of depression was 8.8% (95%CI, 4.64–14.90). Having a family member or friend who had died from COVID-19 was associated with depression (OR = 6.78; 95%CI, 1.39–32.90; p = 0.017). Whereas the use of personal protective equipment was found to be a protective factor against developing depression (OR = 0.03; 95%CI, 0.004−0.32; p = 0.003).
ConclusionsApproximately 1 in 10 healthcare professionals and technicians developed depression during the COVID-19 pandemic in this study. In addition, having relatives or friends who had died from COVID-19 was negatively associated with depression and use of personal protective equipment was identified as a protective factor.
La pandemia de COVID-19 ha incrementado la magnitud de enfermedades mentales como la depresión no solo entre la población general, sino también en el personal de salud. En Perú no se conocen la prevalencia y los factores asociados con depresión en personal de salud. El objetivo es determinar la prevalencia e identificar los factores asociados con depresión en el personal de salud, en el contexto de la pandemia por SARS-CoV-2.
MétodosSe realizó un estudio transversal analítico entre mayo y septiembre en establecimientos de salud. Se incluyó una muestra de 136 trabajadores de la salud y se aplicó una encuesta para recoger los datos. La variable dependiente depresión se midió con la escala autoaplicada de Zung. Para identificar los factores asociados, se realizaron análisis bivariado y multivariado por regresión logística con STATA v 14.
ResultadosLa prevalencia de depresión es del 8,8% (IC95%, 4,64–14,90). Se asociaron con depresión el antecedente de tener familiar o amigo muerto por COVID-19 (OR = 6,78; IC95%, 1,39–32,90; p = 0,017). En cambio, se encontró que el uso de equipos de protección personal (EPP) es un factor protector contra la depresión (OR = 0,03; IC95%, 0,004–0,32; p = 0,003).
ConclusionesAproximadamente 1 de cada 10 profesionales y técnicos de salud sufrió depresión durante la pandemia de COVID-19 en este estudio. Además, el antecedente de tener familiares o amigos muertos por COVID-19 se asoció negativamente con depresión y el uso de EPP se identificó como factor protector contra la depresión.