We aim to determine the prevalence of mental disorders in siblings of children with attention deficit hyperactivity disorder (ADHD), and to determine how psychosocial adversity factors relate to this psychopathology, in a low-middle income country (Colombia).
MethodsWe evaluated subjects with ADHD diagnosed according to the DSM-5 criteria, one of their parents and one of their siblings (ages 8-19). We used the ADHD rating scale and a set of instruments to assess the presence of mental disorders as well as psychosocial adversity.
ResultsWe evaluated 74 trios formed by the index case with ADHD, one sibling and one of the parents. We found that 24.3% of the participating siblings also met the criteria for ADHD and another 24.3% for other psychiatric disorders. The risk of these siblings having ADHD increased further when one of the parents reported a history of ADHD. We also found that 28.3% of the families faced high levels of psychosocial adversity as per their scores in the Rutter Adversity Index.
ConclusionsSiblings of subjects with ADHD showed a significant risk for ADHD and other mental disorders. That risk increased if a parent reported a history of ADHD and also when two or more psychosocial adversity factors were present. This study supports the importance of early detection in efforts to decrease the risk for other siblings.
Nuestro objetivo es determinar la prevalencia de trastornos mentales en hermanos de casos con TDAH y cómo los factores de adversidad psicosocial se relacionan con esta psicopatología en un país de ingresos bajos-medios (Colombia).
MétodosSe evaluó a sujetos con TDAH diagnosticado según los criterios del DSM-5, uno de sus padres y uno de sus hermanos (edades, 8-19 años). Mediante la escala de calificación del TDAH y un conjunto de otros instrumentos se evaluó la presencia de trastornos mentales y adversidad psicosocial.
ResultadosSe evaluó a 74 tríos formados por el caso índice con TDAH, un hermano y uno de los padres. Se halló que un 24,3% de los hermanos participantes también cumplían los criterios de TDAH y otro 24,3%, otros trastornos psiquiátricos. El riesgo de que estos hermanos tuvieran TDAH aumentó aún más cuando uno de los padres informó antecedentes de TDAH. También, que el 28,3% de las familias se enfrentaron a altos niveles de adversidad psicosocial según sus puntuaciones en el Índice de Adversidad de Rutter.
ConclusionesLos hermanos de sujetos con TDAH mostraron un significativo riesgo de TDAH y otros trastornos mentales. Ese riesgo aumenta si uno de los padres reporta antecedentes de TDAH y también cuando se presentan 2 o más factores de adversidad psicosocial. Este estudio respalda la importancia de la detección temprana con el fin de disminuir el riesgo para otros hermanos.
Attention deficit hyperactivity disorder (ADHD) is highly common in childhood, with a worldwide prevalence of 5.3%.1,2 Patients with ADHD generally report low quality of life, poor overall functioning and a high prevalence of premature death largely due to accidents.3,4 Additionally, they present multiple psychiatric comorbidities such as oppositional defiant disorder (ODD) and conduct disorder (CD), with reported rates ranging from 40 to 70%, as well as high rates of depressive and anxious disorders, in the range of 30 to 40%.5-8
The heritability of ADHD is high (average, 75%) and it is estimated that up to 50% of parents of ADHD children had the same diagnosis during childhood.9,10 Several studies have shown that the prevalence of ADHD in siblings is also high, ranging from 26 to 45.2%.4,11,12 Siblings of ADHD cases also have an increased risk for other mental disorders such as ODD, tics, anxiety, and CD, with a prevalence of 72.3% in those siblings who also have ADHD, and 42.7% in siblings without ADHD, compared to 33.1% in controls.9 The most common comorbidity in siblings with and without ADHD has been ODD (44.7-59% vs. 11.4-19%), followed by major depressive disorder (MDD) (10.6-36% vs. 8.2-10%).4
ADHD is a chronic disorder. One study found that the appearance and persistence of ADHD have been associated with the presence of 2 or more psychosocial adversity factors such as family dysfunction, low socioeconomic status, large families, criminality in the father, mental disorder in the mother, and child institutionalization (shelters or substitute homes).12
Studies in siblings of subjects with ADHD, specifically about psychosocial adversity and the prevalence of ADHD or other psychopathologies, have not been conclusive due to multiple factors such as population heterogeneity and the methodologies used.13 Besides, the samples studied in developed countries have different genetic and environmental components. Our study seeks to determine in siblings of subjects with ADHD, what is the prevalence of this and other mental disorders, and to examine how psychosocial adversity factors affect this psychopathology, in a low/middle-income country. For the present study, the “Paisa” population was considered, is a very well characterized Colombian genetic isolate.14–16 The main reason is to approach the role of genetic and environmental factors in the development of ADHD in future studies.
MethodsWe conducted a multi-centric cross-sectional, analytical study. The study was endorsed by the ethics committee of the Facultad de Medicina of Universidad de Antioquia and Hospital San Vicente Fundación (HSVF), in the city of Medellín-Colombia, and Clínica CES in Sabaneta-Colombia. We recruited index ADHD patients in a period of one calendar year, in the HSVF outpatient psychiatric office and the Clínica CES for child psychology. Additionally, we consulted the HSVF database of all patients treated with ADHD diagnosis during the last two years, with whom telephone communication was established to confirm diagnosis and eligibility.
The index ADHD cases were diagnosed according to the DSM-5 criteria.2 One of the siblings of these index cases, who was between the ages of 8 and 19, was then selected, following their agreement to participate in the study, confirmed by an assent letter, and an informed consent form signed by the parents. For each one of the index ADHD cases, 1 sibling was selected. Both the index case and the sibling shared a biological mother. We excluded cases with chronic, severe mental illness (schizophrenia or bipolar disorder) and those cases for which a parent was not available to provide the needed information.
We used the following evaluation instruments: a) ADHD rating scale for the DSM-IV (ADHD Rating Scale DSM-IV Version, ADHD RS-IV),17 that has shown good validity in several countries of the world. This scale has been validated in Spanish and used in multinational studies but is not validated in Colombia;18,19b) Children-Global Assessment Scale (CGAS), that provides a global measure of the level of functioning in children and adolescents; c) Apgar family for children,20 that evaluates overall family functioning according to the perception of its members, and can be reliably used in younger family members; d) Brief Psychiatric Evaluation Scale-Modified Adolescent Clinic (BPRS C-25),21 which is a scale designed to provide a descriptive profile of symptoms that is applicable to a wide range of psychiatric disorders in children and adolescents, and a useful clinical instrument to evaluate possible psychiatric conditions in a dimensional way; e) the Mini-International Neuropsychiatric Interview (MINI)22 was used to determine the presence of MDD, suicidal behavior, generalized anxiety disorder (GAD), ADHD and antisocial personality disorder; f) Beck Anxiety Inventory (BAI); g) the Structured Clinical Interview for DSM-IV (SCID) was used to evaluate borderline personality disorder and antisocial personality disorder,23 and h) sociodemographic data and psychosocial adversity form, that was specifically developed for this study;12 we used it to evaluate gender, educational level of patients and parents, family dysfunction, large family, legal problems of the parent, socioeconomic level, age of identification of ADHD symptoms, and mental illness in the mother. This information was used to determine the Rutter Adversity Index (RIA).24
Rutter Adversity IndexFor the present study, we defined a “high RIA score” as the presence of 2 or more of the following factors: low socioeconomic status, large family, criminality in the father, psychiatric disorder in the mother, and family dysfunction. None of the cases had the 6 factors of the RIA (“institutionalization”). We defined each factor as follows:
- •
Low socioeconomic status: the 2 lowest status of the final sample obtained. We took this data according to the economic stratification of housing in Colombia that ranges from level 1 (lowest) to level 6 (highest).
- •
Large family: it was defined as having 3 or more children.
- •
Criminality in the father: we considered this present if the father met criteria for antisocial personality at some time in his life (by the SCID scale), or if there was a history of a legal process in which the father was involved. The mother interviewed was asked about the background of the parent who did not attend the evaluation. A positive history was determined if he presented a history of being detained for more than a week, having been in jail, or having been involved in any legal process.
- •
Psychiatric condition in the mother: we considered it present if the mother met criteria for at least 2 disorders during the life of her children (the oldest child was taken as a reference). These disorders were those assessed with the MINI (MDD, dysthymia, and ADHD). In addition, suicide attempts, dependence on alcohol and/or psychoactive substances, borderline personality disorder, and anxiety disorder assessed by the BAI were considered as part of the psychiatric condition category.
- •
Family dysfunction: we considered it to be present when 2 or more of the following were elicited: single-parent family, frequent arguments/conflicts between parents at any time during the children's lives (occurring one or more times per month), domestic violence (presence of physical violence of at least 1 every 6 months or any episode of violence that produced separation from the parents), and family conflict (Apgar familiar score: ≤ 6, from the index case or from the sibling).
We selected patients with ADHD previously diagnosed according to DSM-5 criteria.2 We defined them as index patients. Then we called their parents and invited them to participate in the study. We scheduled appointments for index patient, 1 of his siblings, and a guardian (mother or father). We performed a 2-h clinical assessment, in which we conducted the ADHD-RS, BPRS C-25, CGAS and, Apgar family scales to children. Also, we conducted the MINI modules for MDD, GAD, antisocial disorder, and ADHD to the tutor. Finally, we collected with the 3 participants sociodemographic data and the psychosocial adversity form. The assessment were conducted by clinicians with experience in child psychiatry, also by pediatric psychiatry third-year psychiatric fellows. They were previously trained in the use of the instruments.
Statistic analysisThe demographic and clinical characteristics of the participants were described by frequencies and percentages for qualitative variables and were described by means±standard deviations for quantitative variables. The frequency of psychopathology and psychosocial adversity was compared between siblings with ADHD and siblings without ADHD. In addition, the frequency of psychiatric condition in siblings was compared according to low or high adversity. For these comparisons, the disparity ratio (odds ratio) with a 95% confidence interval (95%CI) was calculated. These analyzes were performed in the statistical package IBM® SPSS Statistics version 25.00.
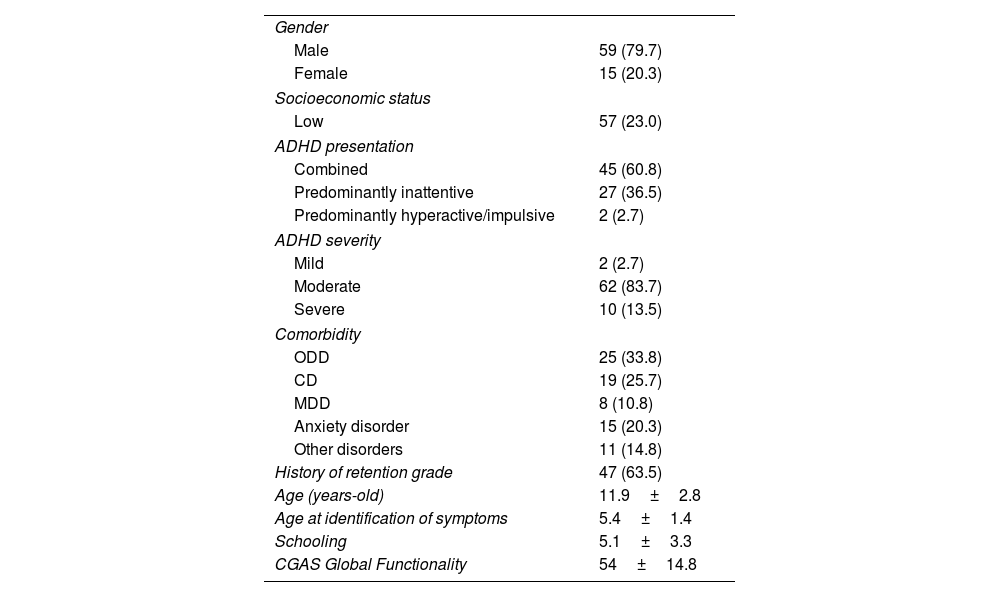
ResultsWe evaluated a total of 74 families. Each family participated with a “triplet” made up of an index case, a sibling, and the guardian. Of the index cases, 79.7% were men, 50% were attending primary school, and almost 2 thirds of them have had been held back in school (‘retention grade’). These subjects had an average C-GAS score at the time of evaluation of 72.14±19.8, and a score at the most severe time of ADHD of 54.0±14.8. Finally, the most common comorbidities were ODD, CD, and anxiety disorders (Table 1).
Characterization of 74 index cases with ADHD.
| Gender | |
| Male | 59 (79.7) |
| Female | 15 (20.3) |
| Socioeconomic status | |
| Low | 57 (23.0) |
| ADHD presentation | |
| Combined | 45 (60.8) |
| Predominantly inattentive | 27 (36.5) |
| Predominantly hyperactive/impulsive | 2 (2.7) |
| ADHD severity | |
| Mild | 2 (2.7) |
| Moderate | 62 (83.7) |
| Severe | 10 (13.5) |
| Comorbidity | |
| ODD | 25 (33.8) |
| CD | 19 (25.7) |
| MDD | 8 (10.8) |
| Anxiety disorder | 15 (20.3) |
| Other disorders | 11 (14.8) |
| History of retention grade | 47 (63.5) |
| Age (years-old) | 11.9±2.8 |
| Age at identification of symptoms | 5.4±1.4 |
| Schooling | 5.1±3.3 |
| CGAS Global Functionality | 54±14.8 |
ADHD: attention deficit/hyperactivity disorder; CD: conduct disorder; CGAS: Children Global Assessment Scale; MDD: major depressive disorder; ODD: oppositional defiant disorder.
Anxiety disorder includes separation, generalized, and social. Other disorders includes tics, enuresis, language disorder, and sleep disorder. ADHD severity was defined by CGAS score (mild, 71-100; moderate, 41-70; severe, 1-40).
Data are presented as n (%) or mean±standard deviation.
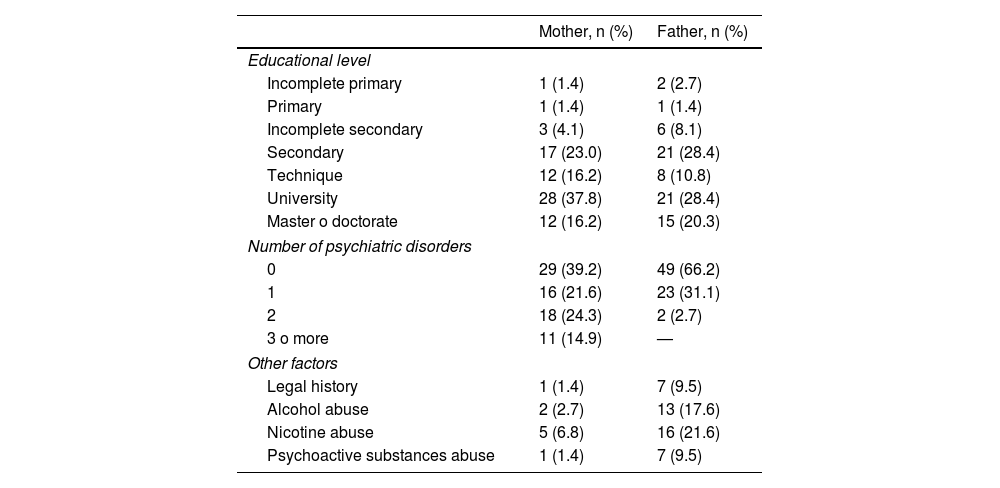
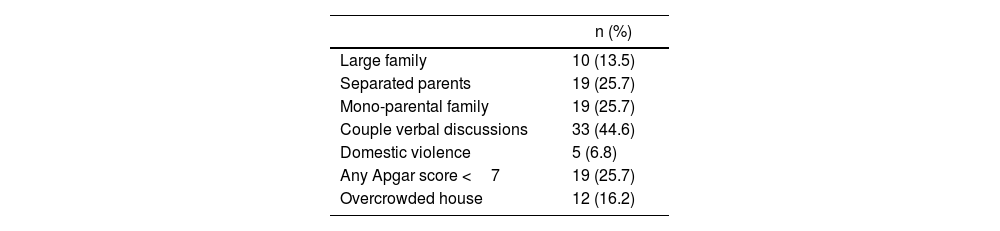
The parents evaluated were predominantly mothers (95.9%) with a mean age of 41.38±6.03 years old. Twenty-seven reported a history of ADHD during childhood and additional 11 (14.9%) had between 3 and 5 psychiatric conditions (Table 2). Of the total sample, 22 families (29.7%) presented family dysfunction, the most frequent factors being verbal discussions (44.6%), followed by separated parents, single-parent family, and an Apgar family score <6 (Table 3).
Characterization of 74 guardians.
| Mother, n (%) | Father, n (%) | |
|---|---|---|
| Educational level | ||
| Incomplete primary | 1 (1.4) | 2 (2.7) |
| Primary | 1 (1.4) | 1 (1.4) |
| Incomplete secondary | 3 (4.1) | 6 (8.1) |
| Secondary | 17 (23.0) | 21 (28.4) |
| Technique | 12 (16.2) | 8 (10.8) |
| University | 28 (37.8) | 21 (28.4) |
| Master o doctorate | 12 (16.2) | 15 (20.3) |
| Number of psychiatric disorders | ||
| 0 | 29 (39.2) | 49 (66.2) |
| 1 | 16 (21.6) | 23 (31.1) |
| 2 | 18 (24.3) | 2 (2.7) |
| 3 o more | 11 (14.9) | — |
| Other factors | ||
| Legal history | 1 (1.4) | 7 (9.5) |
| Alcohol abuse | 2 (2.7) | 13 (17.6) |
| Nicotine abuse | 5 (6.8) | 16 (21.6) |
| Psychoactive substances abuse | 1 (1.4) | 7 (9.5) |
Psychosocial adversity characteristics of 74 participant families.
| n (%) | |
|---|---|
| Large family | 10 (13.5) |
| Separated parents | 19 (25.7) |
| Mono-parental family | 19 (25.7) |
| Couple verbal discussions | 33 (44.6) |
| Domestic violence | 5 (6.8) |
| Any Apgar score <7 | 19 (25.7) |
| Overcrowded house | 12 (16.2) |
APGAR: APGAR family environment scores.
Large family: 3 or more siblings. Overcrowded house: 3 or more persons per room.
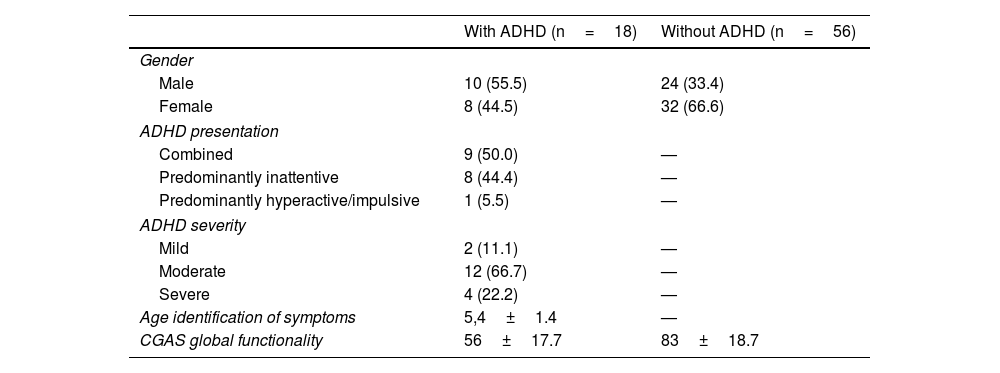
The siblings evaluated were 54.1% female, with an average age of 12.3±3.7 years. About half of them were attending primary school, with a grade average of 5.5±4.2; 66.2% of them had been held back in school (‘retention grade’). ADHD was present in 24.3% of siblings, a majority male, and ADHD combined was the most frequent presentation. The most common psychiatric disorder in siblings with and without ADHD was ODD followed by anxiety disorders. In addition, siblings with ADHD scored lower in the global functionality C-GAS score than siblings without ADHD (Table 4).
Characterization of 74 siblings.
| With ADHD (n=18) | Without ADHD (n=56) | |
|---|---|---|
| Gender | ||
| Male | 10 (55.5) | 24 (33.4) |
| Female | 8 (44.5) | 32 (66.6) |
| ADHD presentation | ||
| Combined | 9 (50.0) | — |
| Predominantly inattentive | 8 (44.4) | — |
| Predominantly hyperactive/impulsive | 1 (5.5) | — |
| ADHD severity | ||
| Mild | 2 (11.1) | — |
| Moderate | 12 (66.7) | — |
| Severe | 4 (22.2) | — |
| Age identification of symptoms | 5,4±1.4 | — |
| CGAS global functionality | 56±17.7 | 83±18.7 |
ADHD: attention deficit/hyperactivity disorder; CGAS: Children Global Assessment Scale.
ADHD severity was defined by CGAS score (mild, 71-100; moderate, 41-70; severe, 1-40).
Data are presented as n (%) or mean±standard deviation.
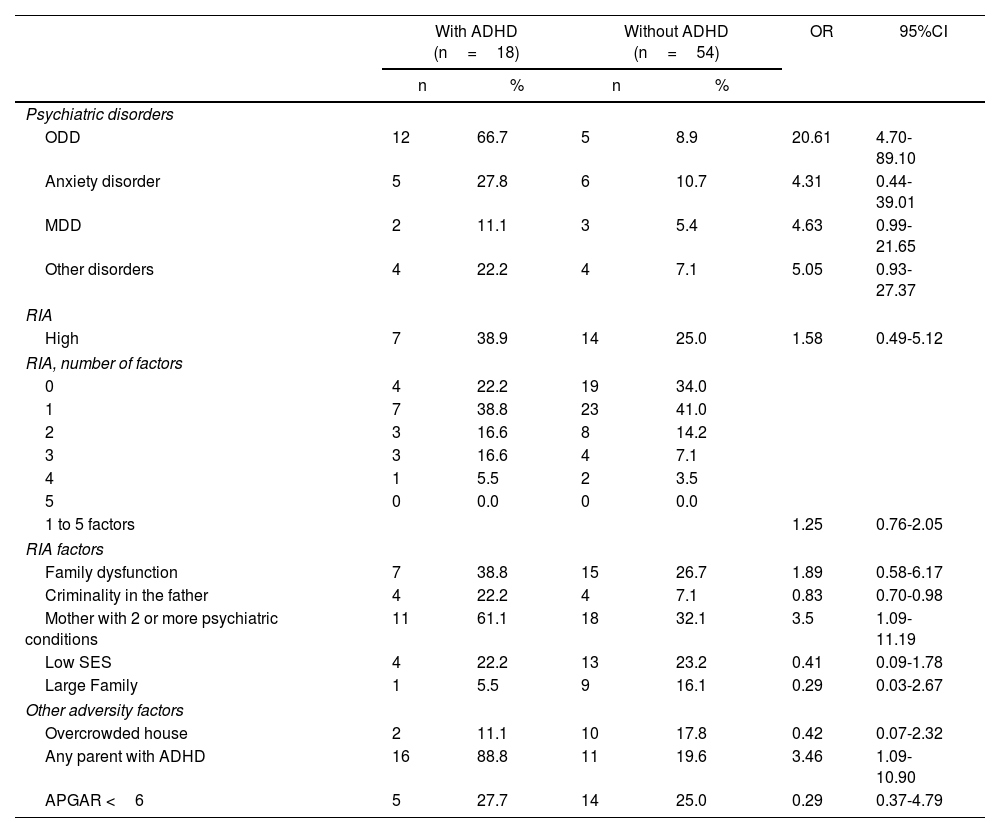
Compared to the group of siblings without ADHD, the group of siblings with ADHD had a high frequency of adversity factors, such as a mother with 2 or more psychiatric disorders (61.1% vs. 32.1%) and also family dysfunction (38.8% vs. 26.7%). Additionally, in this group, the history of ADHD was higher in any of the 2 parents (88.8% vs. 19.6%). On the other hand, a high RIA score was presented in 28.4% of the participating families. Table 5 shows the psychopathological characteristics of siblings, and the psychosocial adversity of their families. Table 6 shows the relationship between a high RIA score and other psychiatric condition.
Siblings psychopathology and psychosocial adversity.
| With ADHD (n=18) | Without ADHD (n=54) | OR | 95%CI | |||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Psychiatric disorders | ||||||
| ODD | 12 | 66.7 | 5 | 8.9 | 20.61 | 4.70-89.10 |
| Anxiety disorder | 5 | 27.8 | 6 | 10.7 | 4.31 | 0.44-39.01 |
| MDD | 2 | 11.1 | 3 | 5.4 | 4.63 | 0.99-21.65 |
| Other disorders | 4 | 22.2 | 4 | 7.1 | 5.05 | 0.93-27.37 |
| RIA | ||||||
| High | 7 | 38.9 | 14 | 25.0 | 1.58 | 0.49-5.12 |
| RIA, number of factors | ||||||
| 0 | 4 | 22.2 | 19 | 34.0 | ||
| 1 | 7 | 38.8 | 23 | 41.0 | ||
| 2 | 3 | 16.6 | 8 | 14.2 | ||
| 3 | 3 | 16.6 | 4 | 7.1 | ||
| 4 | 1 | 5.5 | 2 | 3.5 | ||
| 5 | 0 | 0.0 | 0 | 0.0 | ||
| 1 to 5 factors | 1.25 | 0.76-2.05 | ||||
| RIA factors | ||||||
| Family dysfunction | 7 | 38.8 | 15 | 26.7 | 1.89 | 0.58-6.17 |
| Criminality in the father | 4 | 22.2 | 4 | 7.1 | 0.83 | 0.70-0.98 |
| Mother with 2 or more psychiatric conditions | 11 | 61.1 | 18 | 32.1 | 3.5 | 1.09-11.19 |
| Low SES | 4 | 22.2 | 13 | 23.2 | 0.41 | 0.09-1.78 |
| Large Family | 1 | 5.5 | 9 | 16.1 | 0.29 | 0.03-2.67 |
| Other adversity factors | ||||||
| Overcrowded house | 2 | 11.1 | 10 | 17.8 | 0.42 | 0.07-2.32 |
| Any parent with ADHD | 16 | 88.8 | 11 | 19.6 | 3.46 | 1.09-10.90 |
| APGAR <6 | 5 | 27.7 | 14 | 25.0 | 0.29 | 0.37-4.79 |
95%CI: 95% confidence interval; ADHD: attention deficit/hyperactivity disorder; Apgar: Apgar family environment score; MDD: major depressive disorder; ODD: oppositional defiant disorder; OR: odds ratio; RIA: Rutter Adversity Index; SES: socioeconomic status.
Anxiety disorder includes separation, and generalized and social anxiety disorder. Other disorders includes tics, enuresis, language disorder, and sleep disorder.
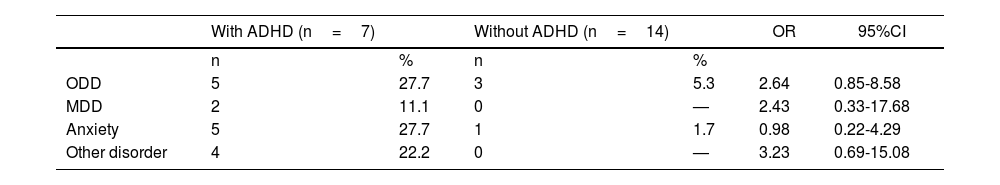
Relationship between siblings with high RIA scores and other psychiatric disorders.
| With ADHD (n=7) | Without ADHD (n=14) | OR | 95%CI | |||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| ODD | 5 | 27.7 | 3 | 5.3 | 2.64 | 0.85-8.58 |
| MDD | 2 | 11.1 | 0 | — | 2.43 | 0.33-17.68 |
| Anxiety | 5 | 27.7 | 1 | 1.7 | 0.98 | 0.22-4.29 |
| Other disorder | 4 | 22.2 | 0 | — | 3.23 | 0.69-15.08 |
95%CI: 95% confidence interval; ADHD: attention deficit/hyperactivity disorder; MDD: major depressive disorder; ODD: oppositional defiant disorder; OR: odds ratio; RIA: Rutter Adversity Index.
Anxiety disorder includes separation, generalized, and social anxiety disorder. Other disorders includes tics, enuresis, language disorder, and sleep disorder.
Our study sought to determine the prevalence of mental disorders in siblings of subjects with ADHD in a developing country. Also it sought to establish the relationship between ADHD and psychosocial adversity factors. We found that in fact, as reported in the literature, these siblings have a high prevalence of ADHD and another psychiatric condition. Siblings seem more likely to develop ADHD if there are two or more conditions of psychosocial adversity in their family. Nevertheless, the strongest association for ADHD in a sibling was to also have a parent with a personal history of ADHD. While the literature supports this association, it has been less clear in demonstrating the relationship between psychosocial adversity, ADHD, and other mental disorders.
Psychiatric disorder in siblingsWe found that siblings of ADHD index cases have an ADHD prevalence of 24.3%, which is higher than that for the general population reported by several studies (3-7.2%).1,3,25 This prevalence of ADHD was similar to that found in other studies of siblings of subjects with ADHD.13 As in the case of other studies, we found that ADHD was more prevalent in male siblings (55.5%) and that ADHD combined presentation was the most frequent (50%), followed by the ADHD predominantly inattentive presentation. A similar study conducted in Mexico by Palacios-Cruz et al. showed that almost half 68.4% of siblings with ADHD had combined presentations.12
Our study showed that siblings with and without ADHD have a high prevalence of other psychiatric disorders. Other studies have also shown that these siblings are at high-risk for psychopathology. Yang et al. in 2011 found, in their study with siblings of subjects with ADHD, that the most frequent mental disorders were ODD, tics, anxiety, and CD. Even for siblings without ADHD, the prevalence of psychiatric conditions was high (42.7%), ODD being the most common.4 Other sibling's study showed that comorbidity with ODD was the most frequent (59%), followed by CD, affective disorders, and substance use disorder.26 In our sample, comorbid ODD was the most prevalent disorder (66.7%), and it was the only disorder showing statistical significance. This result should be interpreted with caution as the confidence interval indicates a possible low level of accuracy. We believe that this effect might change with a larger sample. However, this suggests that, in this group of siblings, ADHD is an important risk factor for presenting ODD.
Clinical implicationsThese findings are clinically relevant. We observed a high prevalence of psychiatric conditions in siblings, even though they had not been previously evaluated for these. One possible explanation for this phenomenon is that the ADHD index case may have shown more striking and dysfunctional symptoms than the other sibling with ADHD. This phenomenon has been called “unmet need”, and has already been described in other studies with the same population.27 This last phenomenon, plus our findings, allows us to highlight the importance of promoting an active search for psychopathology in these high-risk siblings and, thus, to promote early diagnosis and intervention. In the same way, a more adequate approach can be made to reduce the burden of a family with 2 members with mental disorders.
Psychosocial adversityWe found that siblings with ADHD had a high frequency of psychosocial adversity factors, compared to siblings without ADHD (38.8% vs. 26.7%). Although this finding was not statistically significant, the presence of these factors suggests an increased risk for ADHD. The above is similar to that reported by Palacios-Cruz et al. In their study, there were no significant differences in adversity between siblings with and without ADHD, but the average number of adversities was greater in those who did have the disorder. They interpreted this as a risk factor for having ADHD.12 On the other hand, a seminal study conducted on the Isle of Wight also found an association between psychosocial adversity and the presence of various mental disorders, including ADHD.28
We found that as ADHD risk increases, a greater number of adversity factors are present. Moreover, we also found that maternal psychopathology (39,2%) was a specific factor associated with the presence of ADHD in the index case and in the sibling. The latter observation is similar to that highlighted by Biederman et al.24 (36%). On the other hand, a study carried out in Colombia also showed a high prevalence of ADHD in parents (36.6%), although lower than that found in our study.5 However, it is not comparable because that study had a different methodology.
Having a parent with ADHDWe found that children of an ADHD parent have 3 times the risk of presenting the same disorder, which is consistent with the study by Joelsson et al.29 The above can be understood as that the genetic load has a greater influence than the environmental factors.30 However, several studies have shown that living with an ADHD parent represents immense psychosocial adversity, due to greater hostility in parenting, higher levels of conflict, lower levels of cohesion in the family, decreased positive parenting, and high expressed emotions.31–36
This is an ongoing study, and it is possible that, with a larger sample, an association can be confirmed between psychosocial adversity and the presentation of ADHD in these siblings. However, we do not ignore the fundamental role played by the genetic burden of ADHD in first-degree relatives.37 Therefore, studies that seek the role of genetic factors and environmental factors in siblings of subjects with ADHD are required.
Strengths and limitationsOur study has several strengths. First, we use diagnostic scales that are widely used and have high reliability and validity.17 Second, both the diagnosis of ADHD and other psychiatric conditions were confirmed by clinicians with more than 15 years of experience. Third, in this study psychosocial adversity variables were considered, which are related to the presence and persistence of psychiatric conditions. Fourth, although the approach to psychosocial adversity is complex, we managed to do so in a structured way through the RIA. Fourth, this is a family-based approach, selecting a proband with ADHD; it has special relevance in this “Paisa” population, and will allow to carry out population genetics approaches. Finally, this is a study in a developing country that focuses on the population of siblings of patients with ADHD. We also want to point out some limitations. On one hand, in comparison with some previous studies, our sample is smaller, which reduces precision to some of the results obtained. On the other hand, our study allows us to make association relationships between ADHD and other psychopathologies or between these diagnoses and psychosocial adversity, but does not grant us to establish a causal relationship. We hope that with a larger sample and additional Sib-Pair analysis the environment can be differentiated from environmental effects. Moreover, the size of the sample and how the analyses were carried out allow us to make only a few conclusions. This is an ongoing study, intending to triple the sample. Future medical genetic studies with a larger sample size and a reorganization of the data in family trees will allow us to carry out a genetic approach, confirm the current conclusions, and provide new findings.
Our study allows us to conclude that siblings of subjects with ADHD have a high prevalence not only of ADHD but also of other psychiatric conditions. In this population of siblings, the risk of having ADHD or another mental illness increases when they have: a parent with ADHD, a mother with a history of any psychopathology, and the presence of 2 or more psychosocial adversity factors. It is necessary to carry out studies with larger samples, as well as studies that explore psychosocial adversity factors different from those mentioned by Rutter. Besides, to study the relationship between these psychosocial adversity factors with the emergence of ADHD and other psychiatric disorders in siblings to determine measures for the early detection of mental disorders in these high-risk populations, and timely intervention plans in developing countries.
FundingThis project was funded by Colciencias No 111577757629. “Características clínicas, marcadores genéticos, y factores de adversidad psicosocial que predicen Trastorno por Déficit de atención con Hiperactividad (TDAH) en hermanos de alto riesgo”, and also by CODI 2017-16250. “Factores de adversidad psicosocial, genética y clínica asociada al TDAH en hermanos en alto riesgo”. Co-funded by the University of Antioquia and the CES University.
Conflicts of interestThe authors have no conflicts of interest to declare.