Psychiatric diagnosis is based on clinical manifestations, resulting from patients’ internal state, their life situation, the evolution of their condition and the response to our interventions. There are currently few objective data which help to establish the diagnosis which is why this is based on diagnostic criteria such as the Diagnostic and Statistical Manual of Mental Disorders (DSM).
The DSM defines entities by their diagnostic stability, however there are several causes of variability as categorised by Spritzer et al. (1987): subjects variance (changing in patients), occasions variance (different episodes), information variance (new information) and observation variance (different interpretations).
This paper aims to determine the diagnostic stability of patients with Psychotic Disorders among patients readmitted to our Psychiatric Unit.
MethodsRetrospective analysis of the diagnoses of patients with Psychotic Disorders who had been readmitted to our unit. We analysed data from the last 12 years – 5422 admission episodes with 507 patients with a relevant diagnosis in this period.
ResultsPsychiatric diagnosis does evolve over time, nevertheless some diagnostic groups show a relatively significant stability over time – Bipolar Disorder and Schizophrenia with 69% and 77% stability, respectively. Diagnosis such as Depressive Psychosis and Drug-induced psychosis show a significantly lower stability (8% and 21%, respectively).
ConclusionsKnowing our own reality can make us aware that a cross-sectional view of patients can be insufficient and only time can determine a clear diagnosis. This study may help us to understand how psychotic disorders evolve.
El diagnóstico psiquiátrico se basa en las manifestaciones clínicas, consecuencia del estado interno del paciente, de su situación vivencial, de la evolución de su enfermedad y de la respuesta a nuestras intervenciones. Actualmente, existen pocos datos objetivos que ayudan a establecer el diagnóstico por lo que éste se basa en criterios diagnósticos como el Manual Diagnóstico y Estadístico de los Trastornos Mentales (DSM).
La DSM define diagnósticos por su estabilidad, sin embargo, existen varias causas de variabilidad caracterizadas por Spritzer et al. (1987): variación en el sujeto (cambio en el paciente), variación ocasional (diferentes episodios), variación en la información (nueva información) y variación en la observación (diferentes interpretaciones).
Este trabajo pretende evaluar la estabilidad diagnóstica de los pacientes con Trastornos Psicóticos reinternados en nuestro internamiento psiquiátrico.
MétodosAnálisis retrospectivo de los diagnósticos de los pacientes con Trastornos Psicóticos con reingresos en nuestro servicio. Se analizaron datos de los últimos 12 años - 5422 admisiones con 507 pacientes con diagnóstico de interés en ese período.
ResultadosEl diagnóstico psiquiátrico se altera con el tiempo, sin embargo, algunos grupos revelan una mayor estabilidad a lo largo del tiempo - Perturbación Afectiva Bipolar y Esquizofrenia con el 69% y el 77%, respectivamente. Los diagnósticos como la depresión psicótica y la psicosis tóxica, revelan una estabilidad significativamente menor (8% y 21% respectivamente).
ConclusionesConocer nuestra realidad nos hace conscientes de que una mirada transversal a los enfermos puede ser insuficiente y sólo el tiempo puede determinar un diagnóstico claro. Este trabajo puede ayudarnos a entender cómo evolucionan las enfermedades psicóticas.
Psychiatric diagnosis is based in the clinical presentation which is made into objective data by the mental state examination performed by a Psychiatrist. The mental state depends on the patient's life story, the evolution of the disease and the current state. So far, there aren’t many objective means to helps us obtain a diagnosis so the psychiatric diagnosis is framed by diagnostic criteria such as Diagnostic and Statistic Manual of Mental Disorders (DSM) or the International Classification of Diseases (ICD). Although there are clinical presentations that can point us towards a diagnosis, there aren’t any pathognomonic symptoms of any kind of Psychosis1.
For the accurate diagnosis of an entity it's crucial to include a longitudinal evaluation which requires a long follow up. Therefore, diagnostic uncertainty is part of the psychiatric evaluation.
Since the early classification systems proposed and until the most recent criteria systems, one of the main features of a psychiatric diagnosis is its stability over time – the more stable one diagnosis is, the more likely it is to represent a consistent pathophysiologic process2. Diagnostic stability2 reflects how a diagnosis is maintained over consecutive evaluations of the same patient.
Diagnosis is important for the treatment and prognosis but also the investigation field which needs to be uniform and replicable creating homogeneous groups allowing aetiology, pathogenesis and treatment studies to take place1.
There can be various causes for variability or diagnostic instability as presented by
Spritzer et al. (1987): subject variance (change in patients), occasions variance (differences between different episodes), information variance (new or better information), observation variance (different clinical interpretation) and criterion variance. Only the quality of the clinical evaluation and the tools to obtain information can be trained in order to improve clinical abbilities1. This is of utmost relevance in psychotic disorders as they tend to have a chronic course leading to long term treatment frequently based on an early diagnosis.
We aim to evaluate the diagnostic stability of our ward using the diagnosis at discharge.
Materials and MethodsThis is an observational, naturalistic, longitudinal and retrospective study based on discharge diagnosis of the Psychiatric Ward at the Psychiatric Department of Centro Hospitalar Gaia/Espinho from January 2005 until December 2016. From the 5422 admissions representing 3138 patients we selected those with more than one admission (n=966). From this data pool we analysed those with at least one admission having one of our diagnosis of interest for the purpose of this study – Primary or Secondary Psychotic Diseases. We then came to a 507 patients sample (n=507).
We decided to use the diagnosis at discharge from our ward as these are mandatory to be filled and they are assumed to be more acurate3 because of the type of continued and multidisciplinary evaluation with families and because in this setting we have the opportunity to use the information previously collected by the attending psychiatrist. Using this information registered by the attending psychiatrist can be useful in order to better understand the evolution of the disease but it can also lead us to maintain a previously assigned diagnosis. In our unit the classification in use during this period was still the International Classification of Diseases 9 (ICD 9).
We decided to study diagnosis stability using major disease groups as it didn’t seem relevant to analyse differences associated with different phases of the same condition.
The data were analysed using Excel and SPSS and this study was approved by the Ethics Committee of Centro Hospitalar Gaia / Espinho.
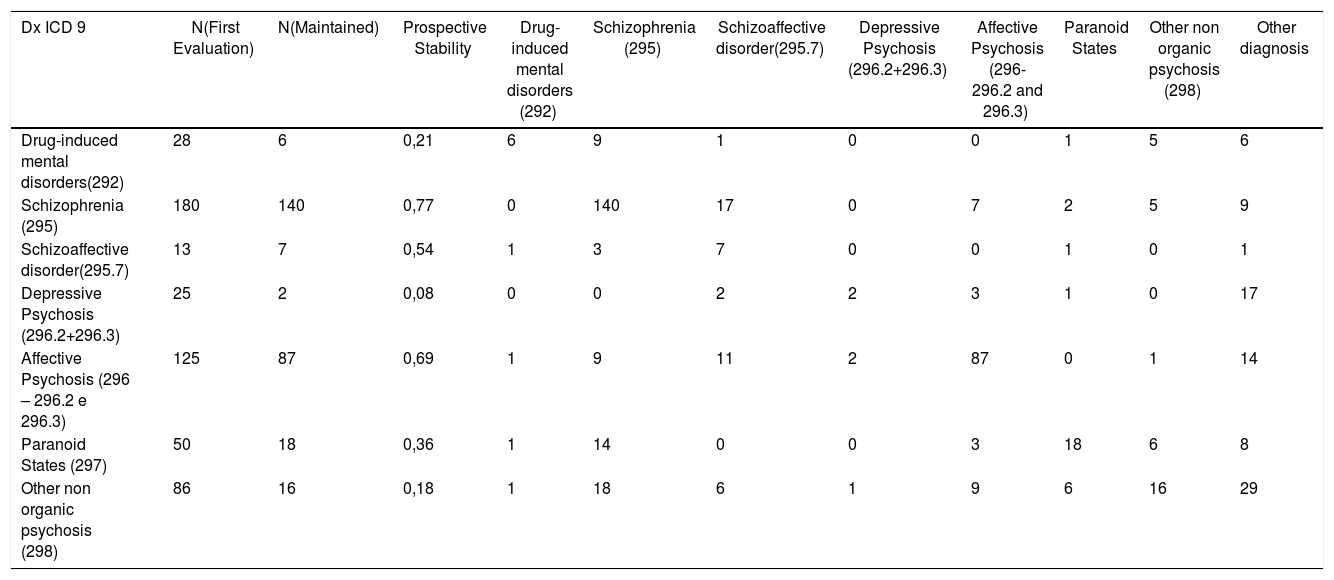
ResultsThe prospective general stability in this sample was of 54% which states the proportion of individuals who maintained the same diagnosis of a specific Psychotic Disorder in the latest discharge comparing with the first admission discharge. We assumed the latest discharge as Gold Standard as this was stablished with more information (previous data and longitudinal data). Table 1
Diagnosis and prospective stability.
| Dx ICD 9 | N(First Evaluation) | N(Maintained) | Prospective Stability | Drug-induced mental disorders (292) | Schizophrenia (295) | Schizoaffective disorder(295.7) | Depressive Psychosis (296.2+296.3) | Affective Psychosis (296- 296.2 and 296.3) | Paranoid States | Other non organic psychosis (298) | Other diagnosis |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Drug-induced mental disorders(292) | 28 | 6 | 0,21 | 6 | 9 | 1 | 0 | 0 | 1 | 5 | 6 |
| Schizophrenia (295) | 180 | 140 | 0,77 | 0 | 140 | 17 | 0 | 7 | 2 | 5 | 9 |
| Schizoaffective disorder(295.7) | 13 | 7 | 0,54 | 1 | 3 | 7 | 0 | 0 | 1 | 0 | 1 |
| Depressive Psychosis (296.2+296.3) | 25 | 2 | 0,08 | 0 | 0 | 2 | 2 | 3 | 1 | 0 | 17 |
| Affective Psychosis (296 – 296.2 e 296.3) | 125 | 87 | 0,69 | 1 | 9 | 11 | 2 | 87 | 0 | 1 | 14 |
| Paranoid States (297) | 50 | 18 | 0,36 | 1 | 14 | 0 | 0 | 3 | 18 | 6 | 8 |
| Other non organic psychosis (298) | 86 | 16 | 0,18 | 1 | 18 | 6 | 1 | 9 | 6 | 16 | 29 |
As expected, the diagnosis with higher stability were those of the major psychiatric syndromes: Schizophrenia with 77% stability and Bipolar Disease (BD) with 69% stability. Depressive psychosis patients were those with a surprisingly low stability of only 8%.
About a third of individuals (32%) initially diagnosed as having Drug Induced Psychosis had a diagnostic shift towards Schizophrenia. However, 21% of those with a first admission diagnosis of Drug Induced Psychosis were latter readmitted with a diagnosis outside the scope of this paper, which means, a non psychotic one. It is also relevant to point out that we focused on readmitted patients, therefore, we can’t extrapolate the percentage of Schizophrenia conversion in these patients – that would be an important issued to be addressed in further studies.
DiscussionSchizophrenia diagnosis implies a longitudinal evaluation with several clinical data and a careful differential diagnosis as it carries a burden of stigma and chronicity. We hypothesize that this is why it is the diagnosis with greater prospective stability with 77% of patients maintaining it. 9,4% shifted towards a Schizoaffective Disorder (SQA), a reasonable number if we consider that only after a major depressive episode or a manic episode can we come to this diagnosis. Only 4% of these patients shifted towards a Bipolar Disorder, a true diagnosis reclassification, which can be questionable or question the previous diagnosis – after an affective episode, in a patient with previous psychotic symptoms meeting criteria for a Schizophrenia Diagnosis, the diagnosis to assume should be one of Schizoaffective Disorder. To point out that from the 180 patients initially diagnosed as Schizophrenic, only one shifted to Paranoia and none evolve into a Drug Induced Psychosis although we it is known that sometimes drug use is maintained.
Schizoaffective Disorder shows a reasonable prospective diagnostic stability of 54% (similar to that of the total sample). To point out that 23% of these patients shifted towards a diagnosis of Schizophrenia. This transition, as previously stated in this paper, raises some issues: the previous medical information wasn’t taken into consideration? Was it not considered trustworthy? This is of the most importance as it can have therapeutics and prognostic consequences in these patients. None of the those initially diagnosed as having Schizoaffective Disorder were latter diagnosed with Bipolar Disorder.
Depressive psychosis refers to a diagnosis of an episode of a morbid state which, although implying surveillance and the risk for a new episode, doesn’t necessarily implies chronicity or irreversibility. Therefore, only 8% of these patients maintained the diagnosis and about 68% shifted towards a diagnosis outside the scope of this paper in a later admission. However, 8% shifted towards Schizoaffective Disorder and 12% to Bipolar Disorder, none was later diagnosed as Schizophrenic.
Bipolar Disorder shows a high diagnostic stability of 69%. 7,2% were reclassified as Schizophrenic raising, once again, the issue: were the previous data dismissed? What new data lead to this reclassification over Bipolar or Schizoaffective Disorder? Despite these questions, 8,8% were reclassified as Schizoaffective patients, presumably presenting one or more psychotic episodes in the absence of major affective symptoms.
From the 50 patients initially diagnosed with Paranoia only 36% maintained it in the most recent evaluation. This diagnosis shows a relatively low stability which could be explained by new data surfaced (personality or functionality compromise, major affective symptoms, etc.) Therefore, 28% were reclassified in later admissions as Schizophrenic and 6% as Bipolar.
Non organic psychosis includes atypical psychosis, brief or reactive psychosis and also those cases where the admission episode wasn’t enough for a clear major syndrome diagnosis. Only 18% of patients maintained this diagnosis. 20,9% shifted to Schizophrenia and 6,7% to Schizoaffective Disorder, 10,6% to Bipolar and 7% to Paranoia. One out of three (33%) was diagnosed as having a diagnosis outside the scope of this paper.
LimitationsDespite being a relevant contribution to the discussion on psychiatric diagnosis, this paper has its own limitations. It is a naturalistic study in which there were no clinical revaluations nor there were used clinical auxiliary tools or questionnaires. To point out that in our study there are different time gaps between the first diagnosis of a psychotic episode and the last one. Also, the classification system in use was ICD 9 which is not the most updated although it is still used in the National Healthcare System in Portugal. All of the diagnosis were made using the same classification system by the different doctors responsible for clinical discharge of these patients.
ConclusionsFrom our data we can see that, psychiatric diagnosis, although in many cases associated with chronicity, aren’t immutable. Diagnosis such as Schizophrenia or Bipolar Disorder show high values of prospective diagnostic stability (of 77% and 69%, respectively) but we have to be aware of the considerable percentage of diagnostic shift. The disease's natural evolution, new data arising and differences in the observer can be some of the causes. Nevertheless, stability percentages are very different depending on the initial diagnosis – for example, Drug Induced Psychosis with just 21% stability or non organic Psychosis with just 18% prospective stability, very different from those of Schizophrenia or Bipolar Disorder.
These diagnostic shifts can have different causes: a natural diagnosis evolution, which means, the progression from one clinical entity towards another, which raises the question if the validity of the diagnosis classification systems we use; new information related to this new admission episode but also from the period between the admissions – making very clear the need for the longitudinal evaluation of a psychiatric diagnosis; and also the differences between different clinicians establishing psychiatric diagnosis.
Classical nominal and dichotomous classifications should be questioned, diagnosis should be seen in a dimensional perspective and elements such as symptoms, evolution, outcome, familial patterns and therapeutic response should be added to the classification4.
A study3 with 485 adults readmitted in a Psychiatric Ward in Kerman (Iran) showed that the diagnosis was more stable for Bipolar Disorder with a 71% prospective stability and Schizophrenia with 55,9% whereas Schizoaffective Disorder should lower stability with only 28,5%. Our sample shows a similar prospective stability in Bipolar patients but a higher one for Schizophrenia and Schizoaffective Disorder. In a study very similar to ours but with outpatients, Bipolar and Schizophrenic patients were also the most stable, supposed to be associated with a more endogenous basis when compared to entities more dependent of “nurture” and the environment5.
Another study7 with 166 patients from a First Psychotic Episode Program in Hong Kong, evaluated the diagnosis at follow-up, five years after initial diagnosis. 80,7% of those patients maintained their initial diagnosis. From those who did switch diagnosis, the majority shifted towards Schizophrenia. Bipolar Disorder showed a prospective stability of 100% and Schizophrenia 95,8%. Non Organic Psychosis, Acute and Transient Psychosis and Delusional Disorder showed lower numbers. This tendency was maintained in our sample although with a smaller stability, maybe because this cited study was restricted to a 5-year close follow-up.
Any psychiatric diagnosis can and should be questioned as new data surface. However, this should not overlook a longitudinal frame of one's history and of the disease evolution. According to Baca–Garcia6, diagnostic stability is greater in admitted patients than in those in outer patient appointments making this a privileged setting for diagnostic reclassification. This paper evaluates, as never before (to the extent of our knowledge) the diagnostic stability in a Psychiatric Ward in Portugal. We present a reasonable time frame and a considerable number of patients.
This paper raises questions that can lead to new work in this field: which factors influence diagnosis shift? What is the influence of that shift in the therapeutics plan used in admitted patients? What is the influence of simultaneous substance abuse on the evolution of the diagnosis?
No funding was granted for thus study. No conflict of interest to declare.
Individual ContributionsAll of the above authors contributed to the overal design and concept of this study as it was constructed by the medical team at our unit and also with the help of Rui Magalhães with inputs as to how to improve the data design. All of the authors helped in contribuing to the writing and reviewing of this paper and have all agreed to its final editing.
Conflict of interests and source of fundingThe authors of this paper have no conflict of interest to disclose nor have received any financial support for his writing.