Takayasu Arteritis (TA) is classified as a large vessel vasculitis, it primarily affects aorta and principal branches. The clinical presentation in pediatric patients is odd and there a few literature about it. The case is about a feminine patient hospitalized after birth with diagnosis of patent ductus arterious (PDA), abnormal widening of the descending aorta, aneurysm of the aortic arch. It is kept under close surveillance for 5 years, with imaging improvement in treatment with methotrexate and immunoglobulin, however she presented relapses on two occasions where the caliber decreased in descending aorta and left iliac artery. We can conclude that Identifying AT findings is important for early diagnosis, medical management, and proper monitoring specifically in pediatric patients where little literature is available.
La arteritis de takayasu (AT) se clasifica como una vasculitis de grandes vasos desarrollándose principalmente en aorta y ramas principales. Su presentación en pacientes pediátricos es rara y existe muy poca literatura.Se trata de una paciente femenina hospitalizada al nacimiento donde se diagnostica ductus arterioso persistente (DAP), dilatación de aorta descendente y aneurisma de arco aórtico. Se mantiene bajo vigilancia estrecha durante 5 años, con mejoría imagenológica en tratamiento a base metrotexato e inmunoglobulina, sin embargo presenta recaídas en dos ocasiones donde se observa disminución de calibre de aorta descendente y arteria iliaca izquierda. Se puede concluir que el identificar los hallazgos de la AT son importantes para poder realizar un diagnóstico temprano, manejo médico y vigilancia adecuada específicamente en pacientes pediátricos donde se tiene poca literatura.
Takayasu arteritis (TA) is a large-vessel vasculitis that mainly involves the aorta and its branches 1. It particularly affects females between 10 and 40 years,2 with a greater distribution in Asia.3 Its incidence in adults is 2.6/1,000,000 per year in North America, while the incidence in pediatric patients is unknown.4
AT presents non-specific symptoms such as headache, hypertension, fever, arthralgia, diaphoresis, and weight loss4; however, the presentation in children is usually atypical.
Case presentationFemale patient, hospitalized at birth in 2015 due to suspected genopathy with symptomatic hypoglycemia, apnea, intrauterine pneumonia, and septic shock. During her hospital stay, a patent ductus arteriosus (PDA) was diagnosed. After surgical repair, an echocardiogram revealed dilation of the descending aorta and aneurysm in the aortic arch posterior to the subclavian artery, as well as the presence of a 4 × 3 cm thrombus at the opening of the superior vena cava. Therefore, a computed tomography angiography was performed, which revealed an aortic aneurysm, probable aortic coarctation, and an abdominal aortic aneurysm. Infectious etiology was ruled out and treatment with immunoglobulin, prednisone, and anticoagulation was initiated. This article describes the 5-year follow-up of the patient.
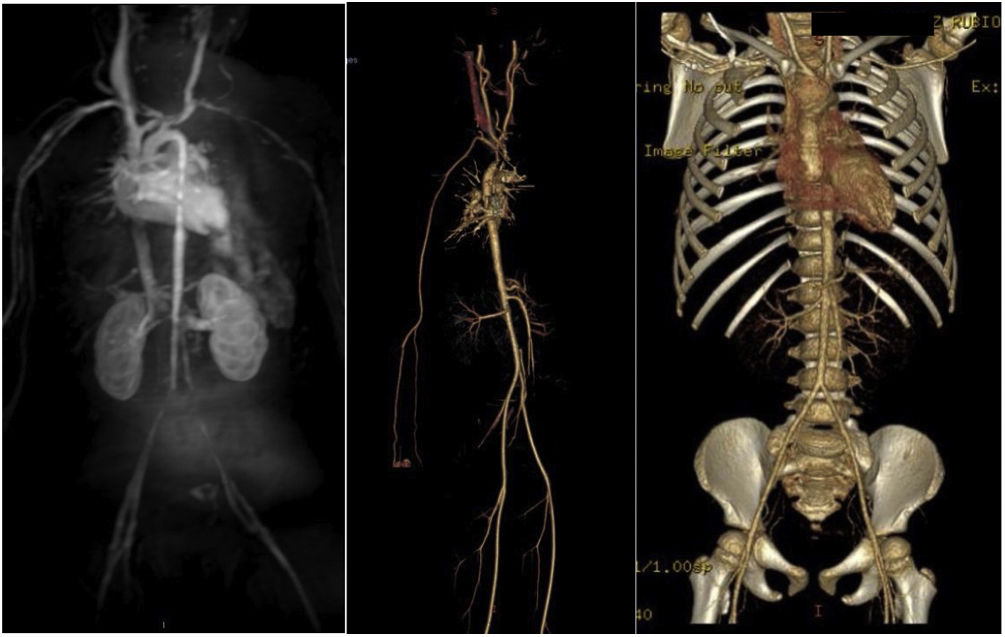
In 2015, after 6 months of treatment with monthly immunoglobulin, new imaging studies revealed aortic arch, ascending, descending, and abdominal aorta with normal caliber, absence of lesions, or abnormal paths. (Fig. 1).
After 10 months (2016), the patient was without control treatment. A magnetic resonance angiography reported segmental stenosis, moderate post-stenotic dilation, and areas of caliber reduction in the infrarenal abdominal portion, important stenosis in the origin of the left iliac, and abnormality of segmental caliber in supra-aortic trunks; hence, treatment was started with methotrexate, folic acid, and immunoglobulin (Fig. 2).
One year later, control CT angiography was taken, revealing images within normal ranges. The patient reported an absence of symptoms.
In 2018, an imaging study showed remission of the aortic spasm and stenosis of the left iliac artery. The patient was in good general condition, so she continued treatment with methotrexate and folic acid.
In 2019, the control study demonstrated an adequate caliber of the aorta and iliac bifurcation, without the presence of stenosis. Medication was suspended with continued surveillance and control echocardiograms (the last conducted in 2019, without abnormal data) with negative acute-phase reactants.
DiscussionTA is an unusual diagnosis in pediatric patients due to its low incidence and non-specific clinical presentation. The best way to make a diagnosis of this disease is with the support of imaging, such as computed tomography (CT) and magnetic resonance imaging; in these cases, CT is preferred, recommending CT angiography, which will allow observing the caliber of the arteries, mural changes, and stenosis. This study should include the aortic arch, abdominal aorta, visceral branches, and iliac arteries, considering that the main arteries affected are the left subclavian, abdominal aorta, right renal, and descending thoracic aorta.5 In the same way, four imaging patterns of TA can be identified:
- A)
Variable decrease in caliber in aorta and arteries;
- B)
Full occlusion;
- C)
Fusiform and saccular aneurysms;
- D)
The irregular contour of the aortic wall.
According to imaging findings, we can classify the disease into four types6:
- 1
Limited to the aortic arch and its branches.
- 2
Involvement of the descending thoracic aorta and abdominal aorta.
- 3
Extensive affection, including the aortic arch, thoracic and abdominal aorta.
- 4
Cases with pulmonary involvement added to type 1, 2, and 3 features.
Cases of TA in newborns are not frequently reported in the literature; only about four cases are known, all with different characteristics from our patient: the youngest, 27-days- old, was diagnosed with necrotizing aortitis.
Unfortunately, subjects have a poor prognosis in the absence of treatment; in some occasions, the diagnosis is carried out with autopsy, as was the case of a 3.5-month-old patient admitted to the hospital with evidence of thrombosis; 21 h after, he died; autopsy evidenced TA.7
Treatment to suppress TA activity is usually with steroids and immunosuppressants such as methotrexate and cyclophosphamide; in some cases, percutaneous transluminal angioplasty may also be viable as a palliative treatment.8 However, our patient was refractory to steroids; thus, immunoglobulin was included in his management, with a favorable outcome, avoiding the use of immunosuppressants to reduce the risk of age-related infections, coupled with the lack of vaccination.
ConclusionIdentifying TA findings is important to perform an early diagnosis, establish prompt medical management, and adequate surveillance, specifically in pediatric patients, for whom there is scarce information in the literature. Therapy must be individualized, with a risk/benefit assessment of each of the options and knowledge of their mechanism of action, reducing mortality, and improving prognosis.
Ethical ConsiderationsThe ethics committee of the Jalisciense institute of clinical research approved the research. The authors have complied with the relevant ethical standards for publication and have the informed consent of the patients.
FinancingThe work has not been previously funded or submitted.
Conflict of interestsThe authors declare the absence of any conflict of interest.