Eosinophilic angiocentric fibrosis is an uncommon tumefactive lesion of the ocular orbit and upper respiratory tract. We present a 44-year old man with a history of severe nasal congestion and nasal obstruction. The patient also reported symptoms of sinusitis. Submucous thickening tissue had been locally resected and the involved anterior nasal septum cartilage partially removed. Histopathological examination of the biopsy indicated eosinophilic angiocentric fibrosis. A CT scan of the sinuses showed a high-density focal mass of soft tissue arising from the anterior aspect of the nasal septum. Examination under low power view showed dense concentric fibrosis and mixed inflammatory cells. The fibrosis was in an angiocentric pattern, resembling an onionskin. High power view showed a mixture of lymphocytes, plasma cells, numerous eosinophils, and proliferating fibroblasts. A test for serum IgG performed ten years after the patient's initial presentation was 1421mg/dl (normal range 540–1822mg/dl), and the serum concentration of IgG4 was 168.70mg/dl (normal range 6.1–121mg/dl). A review of the original hematoxylin and eosin-stained slides revealed that this case was stained immunohistochemically with an IgG4 stain showing 50 IgG4-positive plasma cells/HPF.
La fibrosis angiocéntrica eosinofílica es una lesión tumoral infrecuente de la órbita ocular y del tracto respiratorio superior. Presentamos el caso de un hombre de 44 años, con antecedentes de severa congestión y obstrucción nasal, y síntomas de sinusitis. Una TAC de senos paranasales mostró una masa focal de tejidos blandos de alta densidad que crecía desde la cara anterior del septum nasal. Se resecó parte del tabique. Los cortes histológicos mostraron una fibrosis concéntrica densa con patrón angiocéntrico y células inflamatorias mixtas. Se demuestra la presencia de fibrosis angiocéntrica eosinofílica. El dosaje sérico de IgG: 1.421mg/dl (valor normal: 540–1.822) y el de IgG4: 168,70mg/dl (valor normal: 6.1–121). Los preparados histológicos fueron inmunomarcados para IgG4 mostrando 50 plasmocitos IgG4(+)/HPF.
Eosinophilic angiocentric fibrosis (EAF) is an uncommon tumefactive lesion of the ocular orbit and upper respiratory tract. The typical histological finding of EAF is the presence of small-caliber arterioles surrounded by concentric fibrotic fibers, with an inflammatory infiltrate of lymphocytes, plasma cells and predominantly eosinophils. In recent years, the reports have been more frequent, perhaps due to the greater familiarity that exists with this disorder. Trauma and allergies have been involved in its etiology, although little is known since its description in 1985. The EAF has a clear clinic and histological appearance (by which it is diagnosed), but its pathogenesis has not been determined yet.
Deshpande et al.,1 found a patient with EAF with a dramatic elevation of serum IgG4. This fortuitous finding suggested the possibility that EAF would be a form of IgG4-related disease.
We found another case of primary nasal EAF associated with increased serum concentration of IgG4 and a high number of IgG4-containing plasma cells.
CaseA 44-year-old male, referred to our section with a history of progressive severe nasal congestion and obstruction, which affected both nostrils, of 10 years of evolution.
The patient had also reported symptoms of sinusitis, denying a history of trauma, allergies, atopy or peripheral eosinophilia. At the time of the visit, thickened submucosal tissue had been resected and the tissue that compromised the anterior segment of the nasal septum was removed. The histopathological exam demonstrated the presence of EAF.
The physical examination showed that the patient had a broad nasal bridge, and for this reason, vasculitis (such as Wegener's and Churg-Strauss) were ruled out due to the absence of renal involvement and abnormalities in the chest radiograph.
Studies were conducted to rule out collagen diseases such as systemic lupus erythematosus, Churg-Strauss syndrome, Kimura's disease, angiolymphoid hyperplasia with eosinophilia, granuloma faciale and erythema elevatum diutinum.
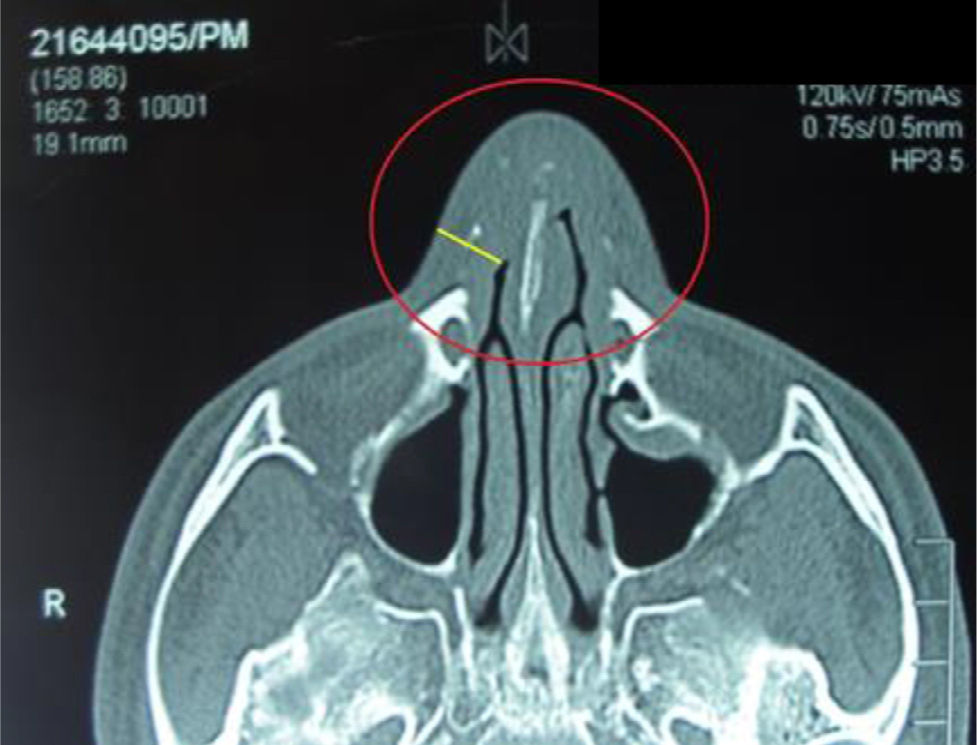
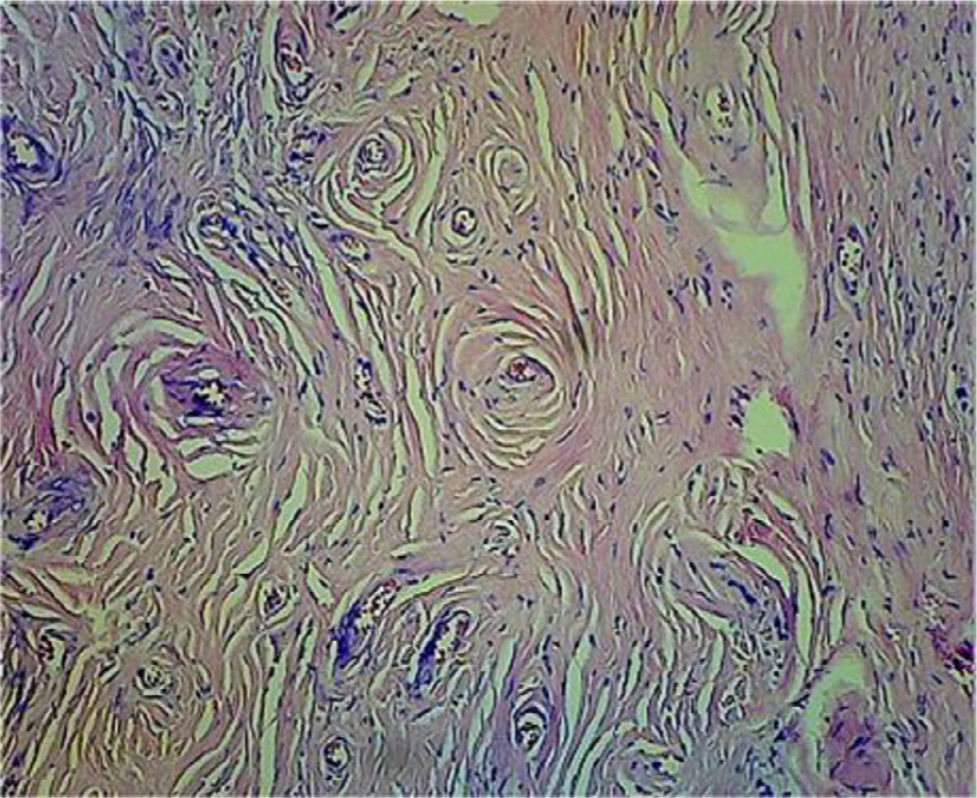
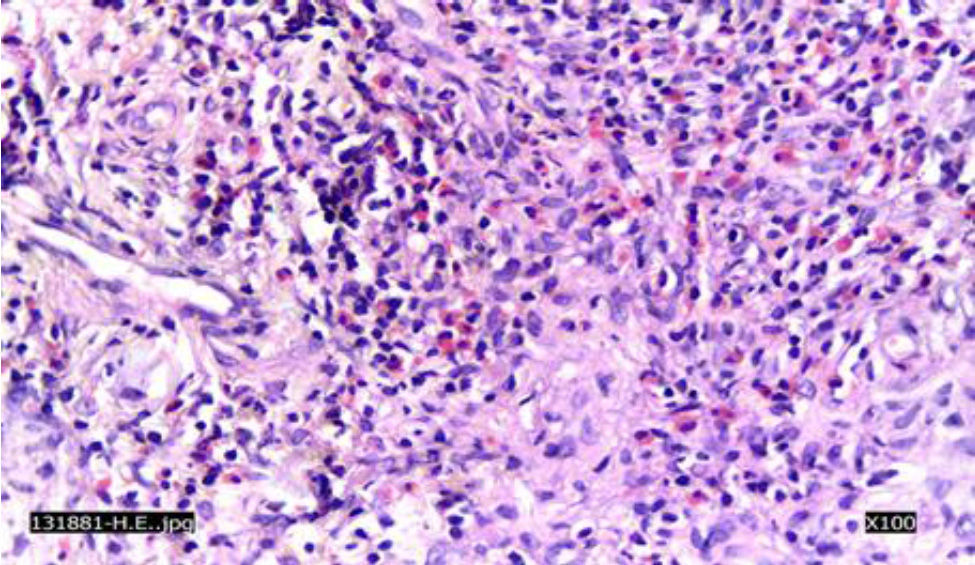
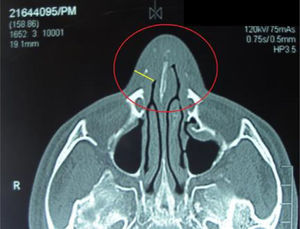
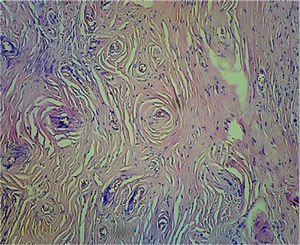
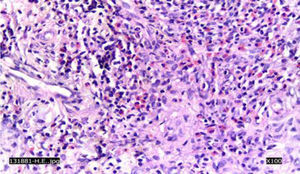
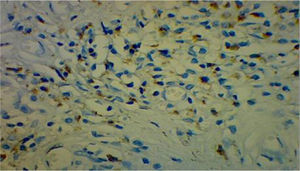
A CT scan of the paranasal sinuses showed a focal mass of high density in soft tissues arising from the anterior segment of the nasal septum (Fig. 1). The histological examination with 20× showed concentric areas of fibrosis (resembling onion cataphylls): (Fig. 2) and mixed inflammatory infiltrate (lymphocytes, plasma cells, eosinophils and fibroblasts proliferation) (Fig. 3). Granulomas, foreign-body giant cells, geographic necrosis or obliterative venulitis were not identified.
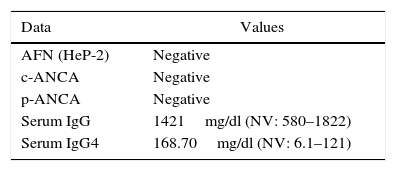
The laboratory data are detailed in Table 1.
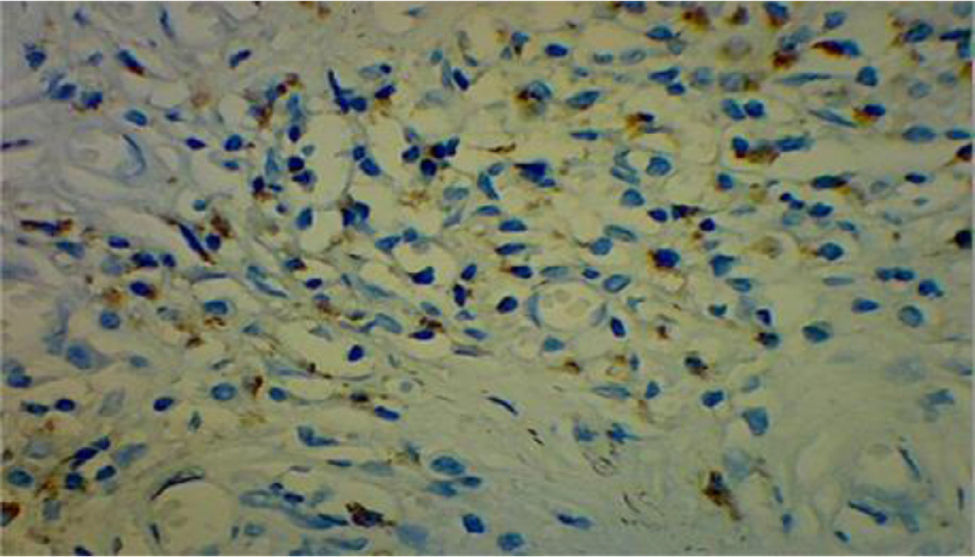
A review of the histological samples stained primarily with hematoxylin–eosin, was immunolabeled for IgG4, showing 50 plasma cells with IgG4/HFP (Fig. 4).
A PET scan with fluoro-deoxy-glucose was also performed, and it was observed accumulation of the glucose in the soft tissues of the anterior area of the septum and the adjacent areas of the nasal wall. The maximum SUV was 2.8.
It was suggested the administration of systemic steroids (0.6mg/kg/day) with gradual decrease thereof and methotrexate 10mg/kg/day with folic acid supplementation to maintain the effect of prednisone and allow the decrease of the steroids. The patient refused treatment.
DiscussionEAF is a chronic idiopathic disorder that involves the upper respiratory tract with progressive submucosal perivascular fibrosis. The etiology is unknown, even though allergy and trauma have been suggested as possible causes.
The sites most frequently involved are the septum and the lateral nasal walls, but cases of involvement of the maxillary sinuses, orbit, skin, subcutaneous tissue of the arms, breasts and subglottic area have also been reported. The clinical findings of the EAF are non-specific and they produce a variety of symptoms, including nasal obstruction with rhinorrhea, epistaxis, pain, swelling and breathing difficulty. Ophthalmic manifestations such as proptosis, periorbital edema, displacement of the eyeball and epiphora have been described more rarely.2–5 A recent study has proposed that EAF could be part of the spectrum of IgG4-related diseases.1
Our patient presented all the symptoms described in the nose and the paranasal sinuses (obstruction with rhinorrhea, epistaxis, pain, swelling and breathing difficulty).
Men and women are affected in the same proportion and the average age at diagnosis is 48 years, with a range of 19–72. The cases reported in the literature comment an average duration of symptoms of 6.6 years before reaching the diagnosis. In the series reported by Thompson et al., the average duration of the symptoms was 3 years.6
The clinical course of the EAF is a slow progression of the fibrosis, but there is evidence that the lesion becomes stable over time. Mortality due to EAF has not been reported.
The diagnosis of EAF rests on the histology. From this point of view, it corresponds to an eosinophilic vasculitis and an angiocentric fibrosis with an onion cataphylls pattern. The lesion progresses from an early inflammatory lesion into a late fibrotic one. The early lesion is a vasculitis with inflammatory infiltrate containing eosinophils, plasma cells and lymphocytes. It involves only the microvasculature, usually with a patched distribution which evolves into foci of fibrosis. Characteristically there is an absence of fibrinoid necrosis or true granuloma and the mucosa is typically respected. The late lesion is characterized by a dense fibrous infiltrate with perivascular fibrosis in onion cataphylls and a patent of microvasculature with scarce inflammatory infiltrate.2
Deshpande et al., have shown that the lesions of EAF share several characteristics with the IgG4-related disease, including the presence of tumor lesions, high number of IgG4-containing plasma cells and increased levels of serum IgG4.
The differential diagnoses are broad and include Wegener's granulomatosis, Churg-Strauss syndrome, granuloma faciale, Kimura's disease, angiolymphoid hyperplasia with eosinophilia, erythema elevatum diutinum, neoplasia and parasitic infections. The clinical signs and symptoms, the serological markers, the blood count and the images help to exclude other diseases. However, the diagnosis of EAF is still histological.6
Radiographic findings are usually non-specific and include opacifications of the paranasal sinuses, bone sclerosis and focal destruction of the surrounding sinus cavity or of the bone tissue of the nasal cavity.6
The treatment of EAF may be medical or surgical, but none of them controls completely the disease. The first consist of steroids, dapsone, antihistamines, hydroxychloroquine or cytotoxic agents (azathioprine, tamoxifen) that do not seem to provide too many benefits. Rituximab would be a reasonable therapy for those patients who are refractory to steroids.1
Most authors agree that surgical resection would be the treatment of choice despite the high degree of recurrences, requiring multiple resections to control the progression of the EAF.2,4,6–9
We conclude that the presence of IgG4-containing plasma cells and the increased serum levels of IgG4 in this patient support the hypothesis of Deshpande that the EAF is a form of IgG4-related disease.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors declare they do not have any conflict of interest.
Please cite this article as: Gallo J, Pisoni C, González Cueto D, Stone JH, Paira S. Fibrosis angiocéntrica eosinofílica intranasal asociada a enfermedad relacionada con IgG4. Rev Colomb Reumatol. 2017;24:189–192.