The rheumatoid nodules have been described in 30% of patients with rheumatoid arthritis. There are localized generally at subcutaneous planes, are rare in visceral organs, and appear typically in advance stages of the disease. Its appearance in atypical localizations can be confused with other conditions. We are going to discuss a patient who debuted with rheumatoid nodules in the liver as first manifestation of rheumatoid arthritis.
Los nódulos reumatoides se han descrito en cerca del 30% de los pacientes con artritis reumatoide, ellos se localizan general a nivel subcutáneo, pero son poco frecuentes en órganos viscerales, generalmente aparecen en estados tardíos de la enfermedad. Su apariencia puede ser confundida con otras condiciones clínicas en las localizaciones atípicas. Nosotros presentamos una paciente que debutó con nódulos reumatoides en el hígado como primera manifestación de artritis reumatoide.
Rheumatoid arthritis (RA) is a chronic autoimmune disease of multifactorial etiology, characterized by symmetric peripheral polyarthritis and bone erosions leading to joint deformity and destruction.1 Different extraarticular manifestations have been described, with varying incidence based on the different studies and geographical characteristics; these extraarticular manifestations present in 17.8–40.9% of patients with RA,2 with rheumatoid nodules being the most common presentation.3 These subcutaneous nodules are usually seen on the extensor surface of the proximal ulna and in pressure areas such as the sacrum, the Achilles tendon, the occipital area and tendons of the hands. Visceral rheumatoid nodules are identified in areas such as the lung and the heart.4 Different series of cases have been conducted in an attempt to describe this type of involvement; however, the development of liver nodules is quite rare and there is little evidence about them.
Clinical caseThis is the case of a 31-year-old female patient who 2 years ago, during her first pregnancy, presented with pruritus and arthralgia in the wrists and fingers. The physical examination showed no inflammatory changes of the joints or primary skin lesions. During puerperium she experienced a notable improvement of her joint symptoms, but persistent pruritus. Her tests indicated elevated transaminases, gamma glutamyl transpeptidase (GGT) and alkaline phosphatase, mild hypoalbuminemia, normal bilirubin, negative tests for hepatotropic viruses, and normal liver and biliary tree ultrasound. Autoimmune profile with anti-smooth muscle antibodies (ASMA) and antimitochondrial antibodies (AMA) with negative IIF; antinuclear antibodies (ANA) IIF 1/80 nucleolar pattern, extractable nucleus antibodies (ENA) with ELISA negative ([reference value: <25U/mL]: anti-Ro 21U/mL, anti-La 8.5U/mL, anti-Sm 2.9U/mL, anti-RNP 6.2U/mL), anti-double stranded DNA with ELISA ([reference value: <20IU/mL]: anti-DNA 22) and antineutrophil cytoplasmic antibodies (ANCA) with ELISA negative ([reference value: <5U/mL]: anti-PR3 1.4U/mL, anti-MPO 2.2U/mL). Treatment with ursodeoxycholic acid and cholestyramine was initiated, with no improvement of the cholestasis.
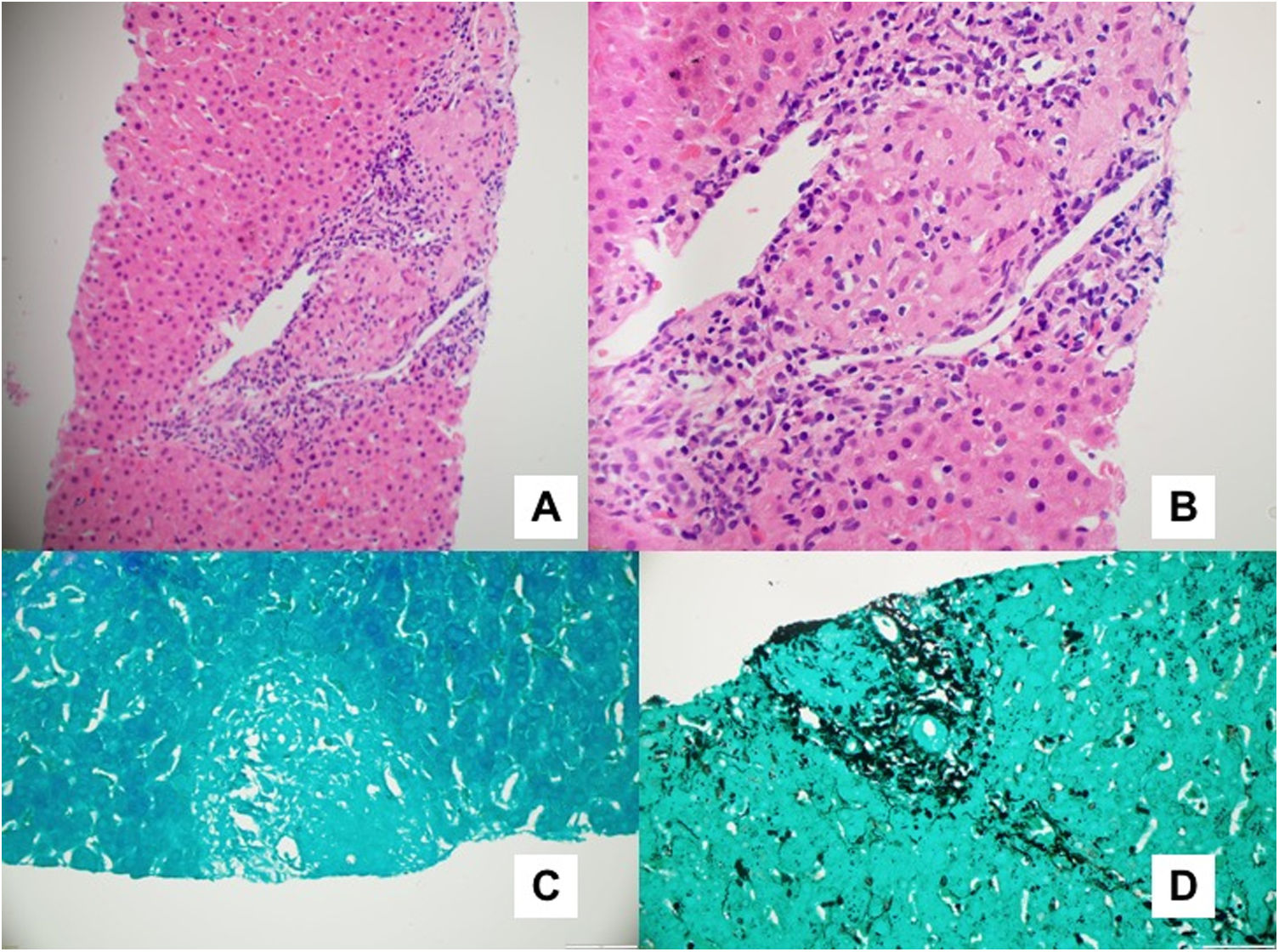
A liver biopsy was performed with findings of chronic granulomatous inflammation with no associated necrosis, localized in the portal triad, with no increase in the portal or periportal inflammatory infiltrate, intact portal structures, and no evidence of ductopenia, ductulitis, ductular proliferation or venulitis. No significant inflammatory infiltrate was identified in the lobule, no steatosis, hepatocyte ballooning, megamitochondria or histological indication suggestive of Mallory’s hyaline, no cholestasis or hyaline globules (Fig. 1). Stains were performed with Ziehl-Neelsen, Gomori, iron, Orcein, PAS, trichrome and reticulin, all negative.
Although the patient never presented respiratory symptoms, due to the characteristics of the findings, additional studies were conducted to rule out sarcoidosis based on angiotensin converting enzyme levels, serum calcium and urine calcium in 24h, which were all negative, as well as a chest X-ray which was normal.
Six months later the patient developed inflammatory arthralgias in the metacarpophalangeal and interphalangeal proximal bilateral joints and exacerbation of pruritus. The physical examination found evidence of joint swelling in the above-mentioned sites.
The paraclinical tests reported positive rheumatoid factor (RF) ([reference value: <14UI/mL] RF: 34), anti-citrullinated protein antibodies (ACPA) with positive ELISA ([reference value: 20–40UI/mL]) ACPA: 353), and persistence of elevated transaminases and alkaline phosphatase; an MRI of the hands showed severe synovial inflammatory changes in the carpal-metacarpal joints, resulting in a diagnosis of seropositive RA. Given the results of the liver tests indicating liver involvement, the patient was treated with steroids, antimalaria agent associated with rituximab biologic therapy. The symptoms regressed and the control liver test were normal.
DiscussionRheumatoid nodules have been described in up to 30% of the patients with RA. These may be detected in exposed areas such as the fingers, tendons or elbows, in organs such as the larynx, pharynx, vulva or breasts and in viscera such as kidneys, lungs or heart.
The liver is one of the largest lymphoid organs and its role is not just as an immunotolerance site, but also as a primary line of defense in the mucosal biology.5 There is evidence of its importance for the immunomodulatory response in chronic inflammatory and autoimmune diseases.6
Liver involvement is not a frequent extraarticular characteristic in RA. The presence of nodules is more frequent in RA when the RF and ACPA are positive; their pathogenesis is not clearly understood; however, it is hypothesized that small hemorrhages in organs give rise to the accumulation of RF complexes on the site of the injury. RF complexes play a chemotactic role in immune response, due to the local activation of monocytes and the development of vasculitis at that level.
Laboratory results may indicate abnormal liver tests which will vary depending on the disease activity, particularly alkaline phosphatase elevation, which has been reported to be high in about 18–50% of patients. In our case, the patient presented persistent AST, ALT and GGT elevation, in addition to alkaline phosphatase. The histological progression of rheumatoid nodules undergoes three stages: one acute-inflammatory, one granulomatous and a final necrotic stage.7–9 Our patient had chronic granulomatous non-necrotizing inflammation localized in the portal triad.
The rheumatoid nodules localized in the viscera have a broad differential diagnosis. In this case, a liver biopsy was performed with immunohistochemical studies and special stains. Additionally, sarcoidosis was ruled out, leading to the diagnosis of hepatic rheumatoid nodules.
The description of hepatic rheumatoid nodules in the literature is scarce; only one report was found in 1986 describing multiple hepatic nodules in the autopsy of a woman with a 13-year history of active AR10; following her diagnosis, possible therapies were evaluated. In view of the scarce or non-existent information on the development of liver nodules, we decided to extrapolate the management approaches in other localizations, finding that the use of conventional disease modifying anti-rheumatic drugs (DMARD) such as methotrexate11 and leflunomide,12 may increase the size of the nodules, despite the good RA response. The poor improvement with some biologics such as etanercept13,14 and infliximab15 has also been documented. Therefore, based on some literature reports,16,17 seropositivity to high titers of auto-antibodies and compromised liver tests, the decision was made to use rituximab, which subsequently improved the symptoms and normalized the liver tests.
ConclusionThe article discusses a rare case of RA; as clinicians there is a need to consider rheumatoid nodules as a potential cause of masses and liver dysfunction.
Conflict of interestsThe authors have no conflict of interests to disclose.
Please cite this article as: Bautista Vargas M, Escobar Cárdenas D, Jiménez C, Echeverri García A. Granuloma no caseificante como primera manifestación de artritis reumatoide. A propósito de un caso. Rev Colomb Reumatol. 2021;28:141–144.