Nailfold videocapillaroscopy is a non-invasive tool for the assessment of peripheral microcirculation, the main indication is the study of Raynaud's phenomenon, poorly standardized outside of this context. There is no clear information in real-life about the reasons for referral, the presence of clinical findings of autoimmune diseases, the frequency of patterns of autoantibodies, and specific capillaroscopic findings.
ObjectiveThe purpose of this survey is to describe the sociodemographic, clinical, paraclinical, and angioscopy findings of a cohort of subjects referred to a capillaroscopy service in North-western Colombia.
MethodsA retrospective study was conducted, from 2015 to 2018. Categorical variables were expressed in frequency and percentage and quantitative variables in mean and standard deviation or median with interquartile range, depending on the distribution of the data.
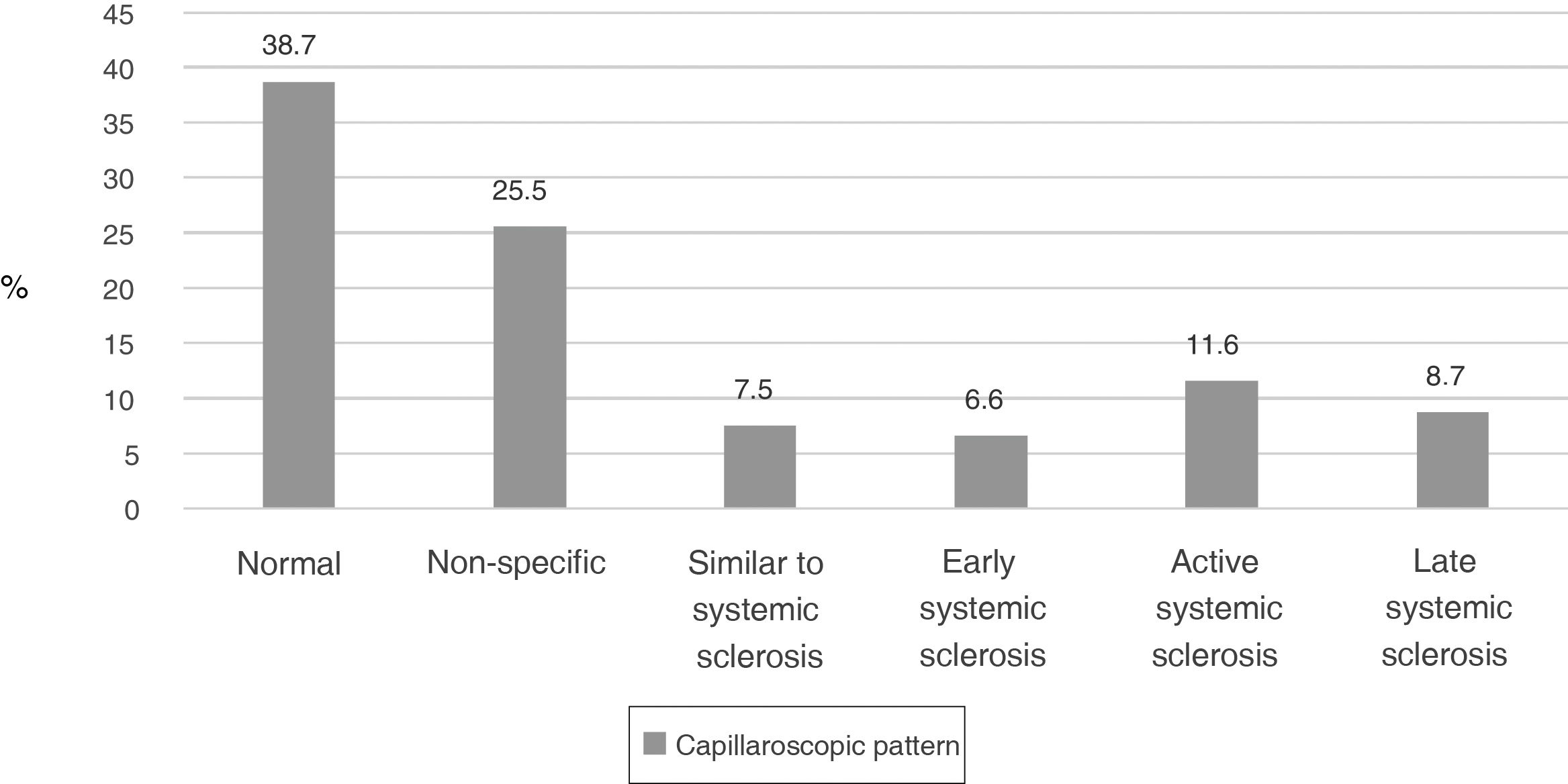
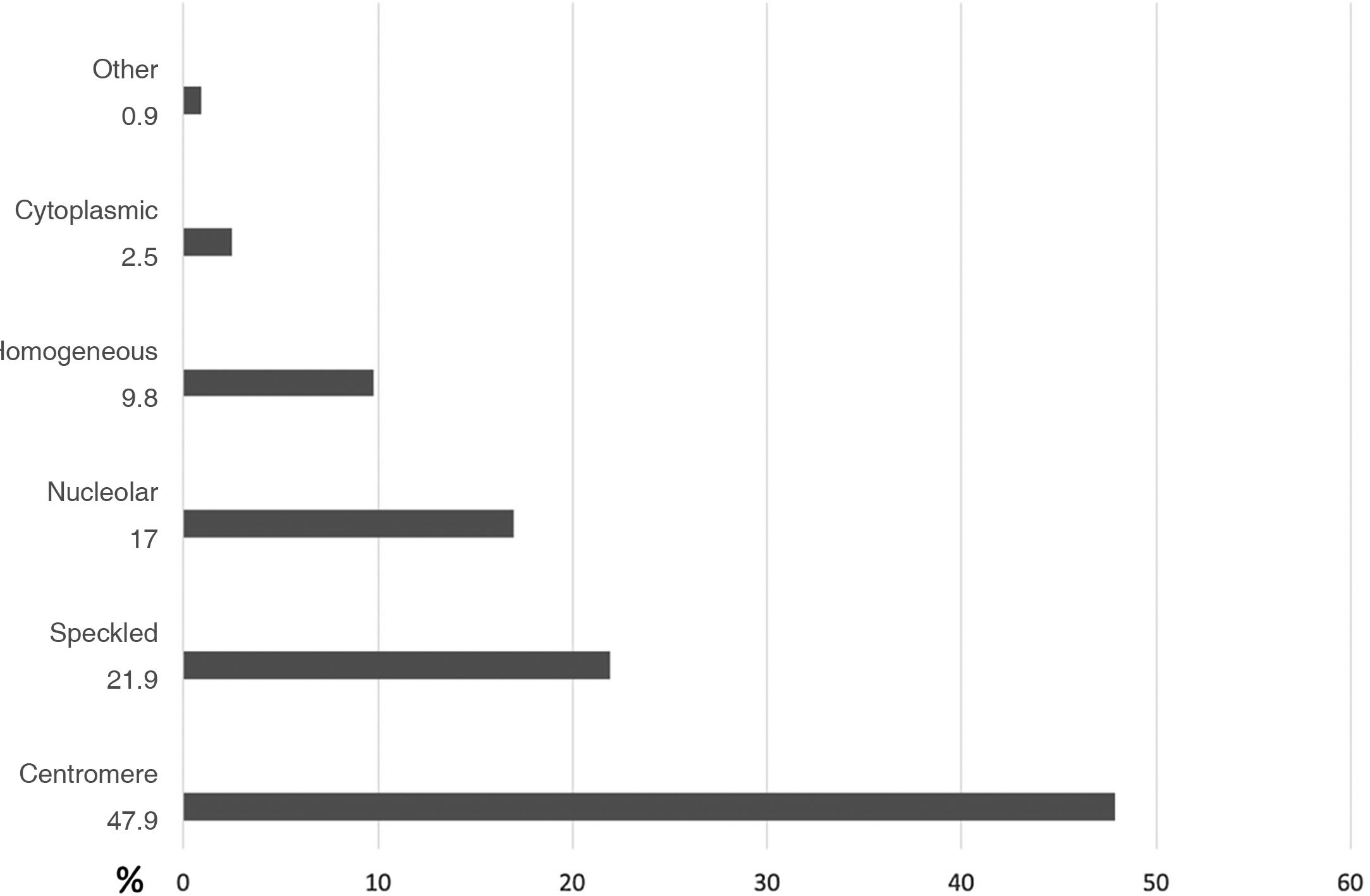
ResultsA total of 318 capillaroscopies were performed for the first time. The main referral reason was Raynaud`s phenomenon (n = 134; 42.1%). The most frequent baseline capillaroscopic pattern found was normal (n = 123; 38.7%). Of the 12 capillaroscopies that presented a non-specific pattern at a 6-month follow-up, only one (8.3%) progressed to a scleroderma pattern. In the subjects with systemic sclerosis, the most frequent clinical finding was sclerodactyly (n = 34; 37.8%), and 42/44 individuals (95.4%) had positive antinuclear antibodies; the most frequent pattern was centromere (n = 27; 64.3%)
ConclusionsIn a real-world setting, the main referral reason for capillaroscopy was Raynaud`s phenomenon; more than a third of the subjects had normal capillaroscopic findings. Sclerodactyly was the most frequent clinical finding in patients with scleroderma capillaroscopic pattern.
La videocapillaroscopia del lecho ungular es una herramienta no invasiva para la evaluación de la microcirculación periférica; la indicación principal es el estudio del fenómeno del Raynaud. Luego de una revisión de la literatura, no hay información clara sobre los motivos de remisión, presencia de hallazgos clínicos de enfermedades autoinmunes, frecuencia de patrones de autoanticuerpos y hallazgos capilaroscópicos específicos.
ObjetivoDescribir los hallazgos sociodemográficos, clínicos, paraclínicos y capilaroscópicos de sujetos remitidos a un servicio de capilaroscopia en el noroccidente colombiano.
MétodosEstudio retrospectivo, de 2015 a 2018. Las variables categóricas se expresaron en frecuencias absolutas y porcentajes y las variables cuantitativas en media y desviación estándar o mediana con rango intercuartílico, dependiendo de la distribución de los datos.
ResultadosSe realizaron 318 capilaroscopias por primera vez. El principal motivo de remisión fue el fenómeno de Raynaud (n = 134; 42.1%). El patrón capilaroscópico basal más frecuente fue el normal (n = 123; 38.7%). De las 12 capilaroscopias que presentaron un patrón no específico, en un seguimiento de seis meses, sólo una (8.3%) progresó a un patrón de esclerodermia. En los sujetos con esclerosis sistémica, el hallazgo clínico más frecuente fue la esclerodactilia (n = 34; 37.8%), y 42/44 individuos (95.4%) tenían anticuerpos antinucleares positivos; el patrón más frecuente fue el centromérico (n = 27; 64.3%)
ConclusionesLa razón principal de remisión para realizar una capilaroscopia fue el fenómeno de Raynaud; más de un tercio de los sujetos tenían hallazgos capilaroscópicos normales. La esclerodactilia fue el hallazgo clínico más frecuente en pacientes con patrón capilaroscópico de esclerodermia.
Capillaroscopy is a non-invasive and reproducible imaging method that allows to evaluate structural changes in the peripheral microcirculation.1 This procedure has different purposes, such as: evaluation of patients with Raynaud’s phenomenon (RF), monitorization of the transition from primary to secondary RF, early diagnosis of systemic sclerosis (SSc) and the differential diagnosis of acrovascular syndromes.2–4
Despite being a procedure frequently used in clinical practice, there is no uniform consensus about its indications; Some authors have suggested the following:5
- •
Evaluation of the RF and differentiation between the primary and secondary RF, being able to contribute to the early diagnosis of a systemic autoimmune disease.
- •
Diagnosis of SSc.
- •
Differential diagnosis of undifferentiated connective tissue disease that presents RF as a clinical manifestation.
- •
Follow-up of non-specific findings: it has been found that a connective tissue disease can be found in up to 20% of these subjects if capillaroscopic evaluation is performed every six months for two years.
In addition to capillaroscopic evaluation, certain clinical findings help to confirm or rule out the presence of SSc: sclerodactyly, diffuse edema of the fingers, sclerosis cutis proximal to the metacarpophalangeal joints, limited mouth opening, platysma sign, and presence of “pitting scars” or digital ulcers, among other findings.6 Other diagnostic aids, such as autoantibodies, allow to correlate and increase the diagnostic probability and provide relevant prognostic information.7
As for the capillaroscopic follow-up, changes over time are described for SSc (patterns: early, active, and late); the approximate time of progression from an early to an active stage and from an early to a late stage is 28 ± 20 months vs. 36 ± 29 months, respectively; likewise, clinical symptoms progress, along with capillaroscopic changes, by 60%.8,9
After an extensive and pragmatic literature review, little information is found in daily clinical practice on the reasons for referral to perform a capillaroscopy, the presence of clinical findings of autoimmune diseases that can be detected during the performance of this procedure, as well as the frequency of autoantibody patterns and capillaroscopic findings specific of SSc.
The purpose of this study was to describe the sociodemographic, clinical and laboratory findings of patients treated in a capillaroscopy service in North-western Colombia.
Materials and methodsPatientsA retrospective study was conducted in patients who were referred to a capillaroscopy referral center in North-western Colombia between January 2015 and December 2018; all patients over 18 years of age who underwent this procedure were included, without any exclusion criteria.
Clinical variablesThe following data from the patients were collected: sex, age, reason for performing capillaroscopy, clinical manifestations of SSc and antinuclear antibodies at the time of the examination (dilution and pattern); comorbidities were not included. These data were compiled in a form.
As part of the evaluation prior to capillaroscopy, two rheumatologists who meet the definition of experts from the Capillaroscopy Study Group of the Pan American League of Associations of Rheumatology (PANLAR)10 reached consensus on the variables of interest for the study; subsequently, they carried out a baseline clinical evaluation of the patients, actively searching for clinical signs of SSc which included: RF, defined according the flowchart of the international consensus of 2014 as: sclerodactyly, diffuse edema of the hands, digital ulcers or “rat bite” lesions (“pitting scars”), telangiectasia, microstomia and platisma sign.11 Gottron’s sign and Gottron papules were also actively searched, looking for dermatomyositis.
Laboratory variablesThe ambulatory report of antinuclear antibodies in any titer and pattern performed with the technique of indirect immunofluorescence was included.12 These antibodies were carried out in different centers.
Capillaroscopic variablesThe videocapillaroscope (Optilia Instruments AB, Sollentuna, Sweden), with a 200× magnification was used, operated by two expert rheumatologists (the Kappa of correlation between rheumatologists is 0.84, 95% CI: 0-66-1),13 once the compliance by the patients of the previous requirements for the performance of this procedure in terms of manipulation of the cuticle, coffee intake and hand washing, among others, was verified. After having applied almond oil to all the fingers of the hand, following the recommendations,14 four photos of each finger were taken in an angle of 90°.
The capillaroscopic variables included were determined according to the videocapillaroscopy semiquantitative scale defined by Cutolo et al.,15 which includes, among other characteristics: visibility, pericapillary edema, subcapillary venous plexus, number of capillaries per millimeter, largest diameter of the capillary evaluated, presence of comb-shaped capillaries, tortuous capillaries, crossing capillaries, dilated capillaries larger than 30 μm, megacapillaries larger than 50 μm, microhemorrhages, avascular areas, neovascularization and capillary disorganization; according to this scale, the patients were classified based on the capillaroscopic patterns defined by Cutolo et al.,15 into normal, non-specific, similar to SSc and SSc (active, early and late) patterns.
Based on the clinical and Capillaroscopic criteria, the 2013 classificatory criteria for SSc were applied.6 In addition, the records of capillaroscopies performed six months later in the subjects who presented a non-specific pattern were included, in order to determine if there was a change in the capillaroscopic pattern found. It was not possible to include clinical information in the follow-up capillaroscopies, which were performed by the same two experts. All capillaroscopies performed between the years 2015 and 2018 were included in the analysis, regardless of the clinical diagnoses and pathological antecedents.
Statistical analysisThe categorical variables were expressed as absolute frequencies and percentages, while the quantitative variables were presented as mean and standard deviation, or as median with interquartile range (IQR), depending on the data distribution. The statistical analysis was performed using the Statistical Package for Social Sciences (SPSS® v.25, SPSS Inc., Chicago, Illinois, USA), licensed for the institution where the study was conducted.
Ethical aspectsThe study was considered without risk for patients, according to current national regulations, due to its retrospective design, and was approved by the health research ethics committee of the participating institution, through act number 16 of October 31, 2018.
ResultsThere was a total of 392 capillaroscopies; 81% (n = 318) of the patients only required one capillaroscopy, while 18.9% had follow-up: 12% (n = 47) required two capillaroscopies, 6% (n = 21) three capillaroscopies, and 1% (n = 5) four capillaroscopies.
318 capillaroscopies were performed for the first time, 94.3% (n = 300) in women; the median age was 46.4 years (IQR: 32.8−58.9). The main characteristics of the study population are summarized in Table 1.
General characteristics in a referral center of capillaroscopy in North-western Colombia (n = 318).
| Characteristics | n (%) |
|---|---|
| Sex (female) | 300 (94.3) |
| Age (years), median (IQR) | 46.4 (32.8−58.9) |
| Reason for referral to the capillaroscopic clinic | |
| Raynaud’s phenomenon | 134 (42.1) |
| Evaluation of the SSc | 79 (24.8) |
| Connective tissue diseases other than SSc | 105 (33.1) |
| ANA positivity n/N | 131/160 (81.9) |
| >1:160 | 107/131 (81.7) |
| Centromere pattern | 59/123 (47.9) |
| Speckled pattern | 27/123 (21.9) |
| Nucleolar pattern | 21/123 (17.0) |
| Capillaroscopic pattern (n = 318) | |
| Normal pattern | 123 (38.7) |
| Non-specific pattern | 81 (25.5) |
| Pattern similar to SSc | 24 (7.5) |
| SSc | 90 (28.3) |
| Early pattern | 21/90 (23.3) |
| Active pattern | 38/90 (42.2) |
| Late pattern | 31/90 (34.4) |
ANA: antinuclear antibodies; SSc: systemic sclerosis; IQR: interquartile range.
It was found that the normal (n = 123; 38.7%) and the non-specific (n = 81; 25.5%) patterns were the most common (Fig. 1). The main reason for referral for capillaroscopy was RF.
Of the individuals referred for capillaroscopy for the first time, 160 (50.3%) had ANA, and 81.9% of them were positive. The most frequent pattern was the centromere, 59/123 (47.9%); the other patterns are schematized in Fig. 2.
Sclerodactyly (n = 81; 47.9%) and “pitting scars” (n = 12; 71%) were the most frequent semiological findings. The other clinical manifestations are summarized in Table 2.
Distribution of the semiological signs of systemic autoimmune disease in a referral center of capillaroscopy in North-western Colombia.
| Semiological sign | n (%) |
|---|---|
| Sclerodactyly | 81 (47.9) |
| Barnett’s sign | 21 (12.4) |
| Puffy fingers | 20 (11.8) |
| Telangiectasia | 19 (11.2) |
| Pitting scars | 12 (7.1) |
| Gottron’s sign | 10 (5.9) |
| Microstomia | 6 (3.5) |
Capillaroscopic follow-up was performed in 47 patients, in a period of six months; the changes in the capillaroscopic patterns are summarized in Table 3.
Correlation between the first and second capillaroscopies in a referral center in North-western Colombia.
| Normal | Non-specific | Similar to SSc | Early SSc | Active SSc | Late SSc | Total | |
|---|---|---|---|---|---|---|---|
| Normal | 11 | 9 | 0 | 0 | 0 | 0 | 20 |
| Non-specific | 5 | 6 | 0 | 1 | 0 | 0 | 12 |
| Similar to SSc | 0 | 1 | 0 | 0 | 0 | 0 | 1 |
| Early SSc | 1 | 1 | 0 | 0 | 2 | 0 | 4 |
| Active SSc | 1 | 1 | 0 | 0 | 3 | 0 | 5 |
| Late SSc | 0 | 0 | 0 | 0 | 1 | 4 | 5 |
| Total | 18 | 18 | 0 | 1 | 6 | 4 | 47 |
SSc: systemic sclerosis.
In 51% (24/47) of the cases there were not changes in the second capillaroscopy, 12 capillaroscopies had a non-specific pattern, only one (8.3%) progressed to a SSc pattern, and five of these were reclassified as normal pattern.
The final diagnosis of SSc, given the clinical and capillaroscopic findings and the ANA pattern, affected 90/318 (28.3%) of the patients.
DiscussionIn the present study, as far as is known, the characteristics of videocapillaroscopy in daily clinical practice, performed in a referral center, are described for the first time, and it is reported that a significant number of referred patients had a normal capillaroscopy and were referred for the study of the RF.
RF is a relatively frequent finding in the general population, with a prevalence of 3% in men and 4% in women16; in primary RF there are no changes in capillaroscopy, which occurs in 60% of the patients17; in secondary RF, the systemic autoimmune disease most frequently found is SSc. In previous studies, videocapillaroscopy has shown good performance in assessing the progression of the SSc, with a sensitivity of 94% and a specificity of 92%17; however, the prevalence of a normal or indeterminate capillaroscopy pattern in patients with SSc can vary between 4 and 20%18; these subjects could correspond to a subgroup of this disease that is characterized by having less skin involvement, less telangiectasias and less lung involvement.
In the present study, 134 patients were referred due to RF, 63 (47%) of them had a normal capillaroscopy. It is presumed that these subjects had primary RF, therefore, 53% of these subjects had secondary RF; of them, 36.6% were explained by SSc. These findings are in agreement with what has been published in the literature.
On the other hand, secondary RF is accompanied by the presence of autoantibodies and significant tissue damage, manifested as digital ulcers or necrosis, in addition to other cutaneous manifestations such as sclerosis cutis, telangiectasias and gastrointestinal symptoms, findings that have been called “red flags”.19 In the present study, the ANA pattern most associated with the capillaroscopic pattern of SSc was the centromere (47.9%); This finding is similar to that reported in other studies, in which it has been observed a prevalence of anticentromere antibodies of around 45%.20,21 The presence of these antibodies, together with abnormal findings in the capillaroscopy, has an hazard ratio (HR) of 9.34 (5.85–14.9) as predictive variables of SSc.22
The presence of semiological signs of SSc was frequently observed in this cohort; the most common in the subjects with a capillaroscopic pattern of this entity were: sclerodactyly, digital ulcers, puffy fingers and microstomia. In a Spanish cohort of 327 patients, the presence of sclerodactyly and puffy fingers constituted the highest specificity for SSc,6 which is consistent with the findings of this cohort.
Given that currently there is no clear consensus in the literature about how often to follow-up by videocapillaroscopy, previous studies have shown changes from primary to secondary RF of up to 20% in a 10-year follow-up, and the annual incidence of transition was 1%.23 More than 90% of the patients with SSc and 85% of those with mixed connective tissue disease (MCTD) present RF as an early symptom24; the follow-up time to find capillaroscopic changes ranges between 29 and 58 months.24 The time suggested to perform follow-up capillaroscopies has been around six months, mainly in individuals who present antinuclear antibodies with titers higher than 1:160 and centromere pattern. An important finding of the present study was observed in patients with a capillaroscopy pattern with non-specific findings, because in the follow-up capillaroscopies it could be reclassified as a normal pattern in 83%, a finding that was not reported in other capillaroscopy referral centers; this may suggest the importance of the capillaroscopic follow-up in this group of patients, where there can be findings specific for SSc, or a return to normality, as occurred in this cohort.
As far as we know and we want to highlight as a strength of this study, it is the first description of the daily practice, of the clinical, paraclinical and capillaroscopic characteristics of a national referral center on this topic. Several limitations are also recognized, such as the inaccuracy of the information on the reason for referral, the scant information on comorbidities associated with microvascular changes (such as arterial hypertension or diabetes mellitus), the reduced number of capillaroscopies that had been followed-up and the absence of clinical changes of the patients during the evolution, the limited access to the medical records of their treating physician (only the reason for referral was known) and the lack of measurement of ANAs with their pattern and titer in all patients.
ConclusionsVideocapillaroscopy of the nailfold is a useful tool in the study of RF; the latter was the main reason for referral to a reference center. In the majority of cases, it was found a normal capillaroscopic pattern, in addition, almost in one third of the subjects it was possible to establish a diagnosis of SSc, with the combination of clinical, serological and capillaroscopic findings, while in a subgroup of subjects with a non-specific capillaroscopic pattern, at six months there was a change towards a normal pattern, which suggests the importance of follow-up with this procedure in light of these findings.
FundingThis research has not received specific support from public sector agencies, the commercial sector, or non-profit entities.
Conflict of interestThe authors declare that they have no conflict of interest for the preparation of this article.