Remitting seronegative symmetrical synovitis with pitting oedema (RS3PO) was described by McCarty (1985), as a benign form of rheumatoid arthritis that onset in men older than 70 years (80% of cases), with symmetrical and associated involvement of oedema of hands and feet. The approach of acute polyarthritis in the elderly should include the RS3PO syndrome, where poor steroid response and multisystem involvement oriented towards paraneoplastic nature, mainly with solid tumours (gastric and pancreatic adenocarcinoma), lymphomas and leukaemia. The case is presented of a patient with RS3PO as a paraneoplastic manifestation of mesothelioma, which is rare in this type of tumour.
El síndrome RS3PE (sinovitis simétrica seronegativa remitente con edema) fue descrito por McCarty (1985) como una forma benigna de artritis reumatoide de inicio en hombres mayores de 70 años, con compromiso simétrico y asociada a edema de manos y pies. El enfoque de la poliartritis aguda en el adulto mayor debe incluir el síndrome RS3PE, en el que la pobre respuesta a esteroides y el compromiso multisistémico orientan hacia una naturaleza paraneoplásica, principalmente tumores sólidos (adenocarcinoma gástrico y pancreático), linfomas y leucemias. Se presenta el caso de un paciente con RS3PE como manifestación paraneoplásica de mesotelioma, una manifestación rara en este tipo de tumor.
A 73-year old patient with a history of hypertension, hypothyroidism, smoking (32 packs per year) and family history of lung cancer, with no history of exposure to asbestos, came to the clinic after experiencing polyarticular pain for 15 days, predominantly in the second and fourth interphalangeal joints and shoulders, in addition to oedema. The physical examination evidenced bilateral hand oedema with fovea and synovitis in the proximal metacarpophalangeal and interphalangeal joints (Fig. 1A), painful movements and limited wrist extension, non-responder to non-steroid anti-inflammatory agents. The paraclinical tests included rheumatoid factor (RF), cyclic citrullinated peptide antibodies and normal erythrocyte sedimentation rate, positive CRP at 13.6mg/dl, and comparative hand X-ray with changes suggestive of osteoarthrosis (Fig. 2). Hand joints ultrasound imaging or MRI were not performed.
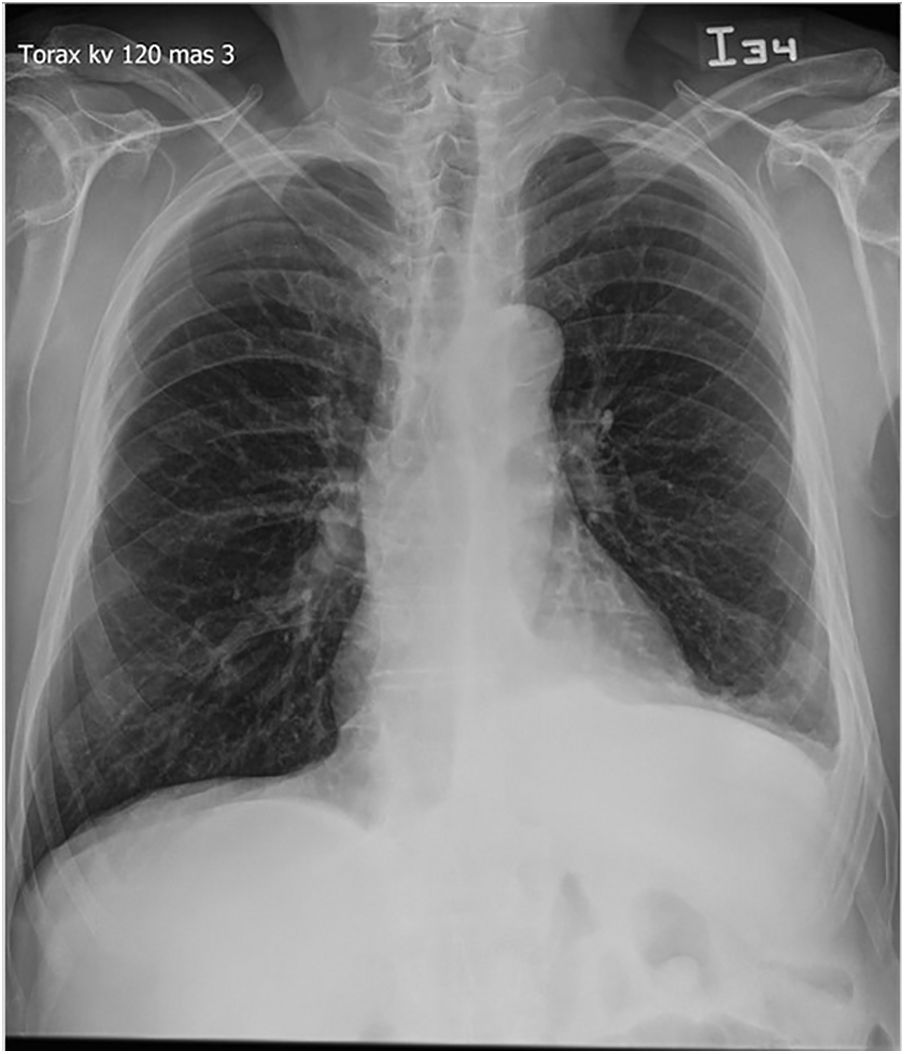
The chest X-ray showed left lymphocytic exudate-type pleural effusion, with positive cytology for malignancy (Fig. 3). The biopsy was obtained via left thoracotomy, with intraoperative findings of nodes of varying size in the posterior and inferior parietal pleura, which infiltrated the diaphragm (the largest node measuring 10×10mm), and immunohistochemistry compatible with stage IV epithelial mesothelioma compromising the lungs.
The patient was initially managed with prednisolone (20mg/day), with significant clinical response at day three (the visual analogue scale index dropped from 8 to 2/10). The treatment was then progressively tapered down to every 72h for 2 weeks, down to a maintenance dose of 5mg/day, and the patient was discharged with this dose, achieving complete resolution of the joint manifestation.
The patient was followed by oncology and received palliative chemotherapy with 6 cycles of pemetrexed and carboplatin, since surgical resection was not indicated being an ECOG 1 patient.
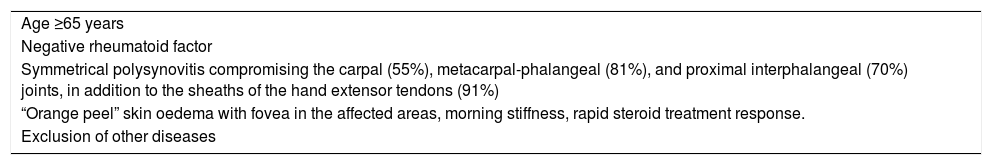
DiscussionThe most frequently mentioned diagnostic criteria for RS3PO to date were published by Olivo et al. in 19941 (Table 1).
Diagnostic criteria suggested for the RS3PE syndrome (remitting seronegative symmetrical synovitis with pitting oedema).
| Age ≥65 years |
| Negative rheumatoid factor |
| Symmetrical polysynovitis compromising the carpal (55%), metacarpal-phalangeal (81%), and proximal interphalangeal (70%) joints, in addition to the sheaths of the hand extensor tendons (91%) |
| “Orange peel” skin oedema with fovea in the affected areas, morning stiffness, rapid steroid treatment response. |
| Exclusion of other diseases |
In a few patients, the comparative hand X-ray shows soft tissue oedema and osteoarthrosis changes. The MRI is able to identify mostly dorsal tenosynovitis in the hands (involvement of the extensor tendons), with no signs of arthritis.2
The differential diagnoses described for this entity include rheumatic polymyalgia (RPM) and late onset rheumatoid arthritis. The association between RS3PE and cancer has been described in the literature since the original report of the syndrome, despite its low incidence among the general population (0.09%),3 which usually precedes the onset of neoplasms. The rates of association seem to be variable according to the continent: cancer was reported in a European/American cohort of patients with RS3PO in 31% of the cases (11/36), as compared against 7% of the cases in the Asian population with RS3PE (2/28), among which there were also reports of isolated RPM in 2.4% (3/123), and presented with a diagnosis of uterine, gastric and hepatocellular carcinoma.4,5 Manzo et al.6 followed 200 patients over 65 years old, for 24 months, and found that those patients diagnosed with RPM+RS3PE developed more cancer (28.5%) than those diagnosed only with RPM (2.04%), with a higher frequency of cancer originating in the prostate, the bladder and multiple myeloma.
Isolated cases of RS3PE syndrome have been described in our population, associated with neoplasm and as a paraneoplastic manifestation in Colombia and Peru7,8; however, there were no cases found in the literature review described as paraneoplastic manifestation of mesothelioma.
From the pathophysiological perspective, up to 50% of the patients present with HLA-B7 (+)9 and elevated serum levels of the vascular endothelial growth factor – both idiopathic and paraneoplastic – have been observed. Elevated levels of metalloproteinase 310 have also been described among the latter cases, which have been associated with invasion and solid tumour progression, in addition to destruction of the synovial membrane, following a synovial hypervascularisation phenomenon and increased vascular permeability driven by VEGF. Genetic sequencing for HLA-B7 was not prescribed in our patient, though it could be helpful in patients with diagnostic suspicion of RS3PE syndrome.
Yanamoto et al.11 reported the association between pleural and pericardial effusion with RS3PE syndrome and documented an exudate-type pleural effusion, negative for malignancy, which responded very well to steroid therapy. The treatment of choice suggested is prednisolone at a maximum dose of 30mg/day, for at least 18 months, with weekly tapering. Most patients improve their symptoms after 72h of starting the medication. In most patients with isolated RS3PE the symptoms resolve with no sequelae. In the group that develops the condition as a paraneoplastic phenomenon (such as our patient), the clinical improvement is only partial, with a higher rate of future relapses. In these patients, the management of the neoplasm is the priority and it determines the prognosis; therefore, in the absence of a cancer diagnosis, the recommendation is to follow the patient for at least 2 years, in elderly individuals with a recent diagnosis of RS3PE. In our case, the clinical response was satisfactory and the diagnosis of malignancy was final.
ConclusionThe occurrence of acute symmetrical seronegative polysynovitis in the elderly, associated to oedema with fovea on the dorsum of the hands and feet, should guide towards the diagnosis of RS3PE. The paraneoplastic association with RS3PE is clearer than with RPM and late onset rheumatic arthritis; therefore, in these cases, a systematic study should be conducted to rule our malignancy. There are no reports in the current literature describing the association of this rheumatological condition with primary tumours of the pleura; hence this case represents a new horizon in the clinical spectrum of cancer-associated manifestations.
FundingNone declared.
Conflicts of interestNo conflict of interest to disclose.
Please cite this article as: Rondón-Carvajal J, Figueroa Lemus WJ, Muñoz-Velandia ÓM. Síndrome RS3PE (sinovitis simétrica seronegativa remitente con edema) como manifestación paraneoplásica de mesotelioma: reporte de un caso y revisión de la literatura. Rev Colomb Reumatol. 2020;27:116–119.