Takayasu arteritis (TA) is a large vessel vasculitis that affects young people, related to cardiovascular outcomes and chronic kidney disease. We present the case of a 20-year-old male with a diagnosis of TA, who developed chronic kidney disease, impaired renal blood flow was ruled out, renal biopsy was compatible with focal and segmental glomerulosclerosis of a collapsing variety, other possible aetiologies were excluded. The mechanisms that mediate this association have not been determined, immune-mediated mechanisms are proposed. According to our review, this is the second reported case of this association and the first with a collapsing variety.
La arteritis de Takayasu es una vasculitis de grandes vasos que afecta a personas jóvenes y se relaciona con desenlaces cardiovasculares y enfermedad renal crónica. Se presenta el caso de un paciente masculino de 20 años, con diagnóstico de arteritis de Takayasu, que desarrolla enfermedad renal crónica. Se descartan alteraciones en el flujo sanguíneo renal, en tanto que la biopsia renal resulta compatible con glomeruloesclerosis focal y segmentaria de variedad colapsante. Se excluyeron otras posibles etiologías. No se han determinado los mecanismos que median en esta asociación; se proponen mecanismos inmunomediados. Según nuestra revisión, se trata del segundo caso reportado de esta asociación y el primero con variedad colapsante.
Takayasu arteritis (TA) is a large-vessel vasculitis, with variable worldwide incidence, with female predominance with a ratio of 6.9:1 compared to men,1 with a mean age of presentation of 25 years. A quarter of patients present the disease before age 20. Its etiology is not well defined, but genetic (associated with the major histocompatibility complex) and infectious factors are involved, mainly Mycobacterium tuberculosis; for example, in Mexican patients, genetic sequences of this mycobacterium have been found in biopsy samples.2 Its morbimortality is related to cardiovascular events and chronic kidney disease. In children it is the third general cause of vasculitis and the most frequent of large vessels; likewise, TA is the main cause of aortic stenosis and renovascular hypertension, with a peak incidence between 10 and 15 years.3
We present the case of a young patient with TA who developed nephritic syndrome in his evolution. The histopathological study is compatible with focal and segmental glomerulosclerosis with collapsing variety; secondary causes such as hemodynamic alterations of renal blood flow were ruled out; it is considered that there is an association with TA, probably through immune-mediated mechanisms.4
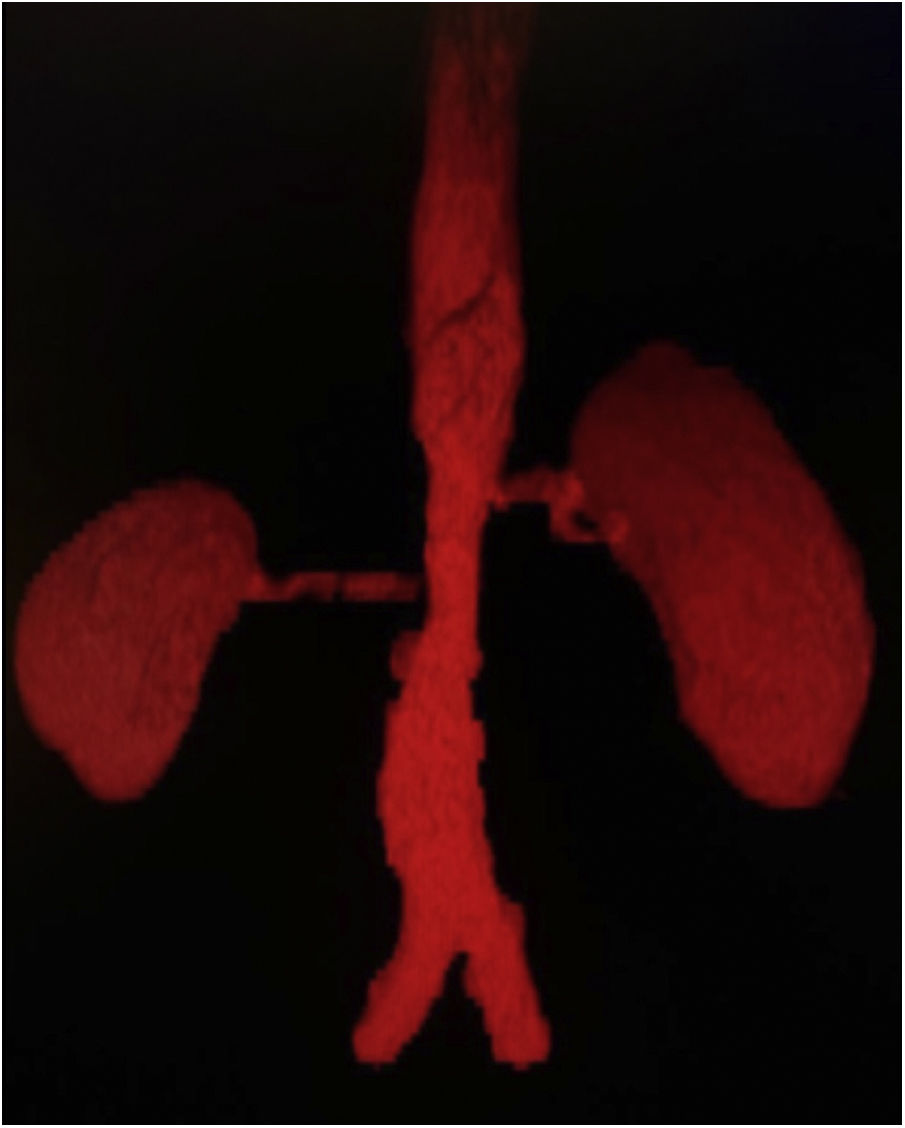
Case presentationA 20-year-old Mexican male, with no relevant family history, began at age 16 with symptoms of pain and claudication in the lower extremities, fatigue, and elevated blood pressure levels. On physical examination, asymmetry of the popliteal and pedal pulses, abdominal bruit, and discrepancy of blood pressure values (>10mmHg) in upper limbs compared to lower limbs was observed. A secondary arterial hypertension approach was started; endocrinopathies were initially excluded. Hence, computed tomography angiography with three-dimensional reconstruction was performed (Fig. 1), in which 70% stenosis of the inframesenteric abdominal aorta involving both renal arteries at the level of the ostium was documented; supra-aortic trunks showed no lesions. An elevation of acute phase reactants (C-reactive protein 18.1mg/dl and erythrocyte sedimentation rate 64mm/h) was found. With this information, TA classification criteria were met. Baseline renal function was preserved (serum creatinine: 0.58mg/dl and glomerular filtration rate: 146ml/min). Immunosuppressive treatment with steroids was started with prednisone at 50mg/day (1mg/kg/day), with a dose reduction to 20mg/day at 6 months follow-up and 5mg/day after 12 months. In addition, methotrexate up to 15mg/week, anticoagulation with rivaroxaban, and antihypertensive therapy with losartan and nifedipine were administered. In the third year of follow-up, there was an increase in serum creatinine; hematuria (20 red blood cells per high-power field), and albuminuria in the subnephrotic range (1441mg in 24h) also were documented. A renal ultrasound is performed, evidencing normal morphology and size: right kidney 9.3×6.6×5cm; left kidney 10.2×7.4×5.1cm in their longitudinal, anteroposterior, and transverse axes, respectively.
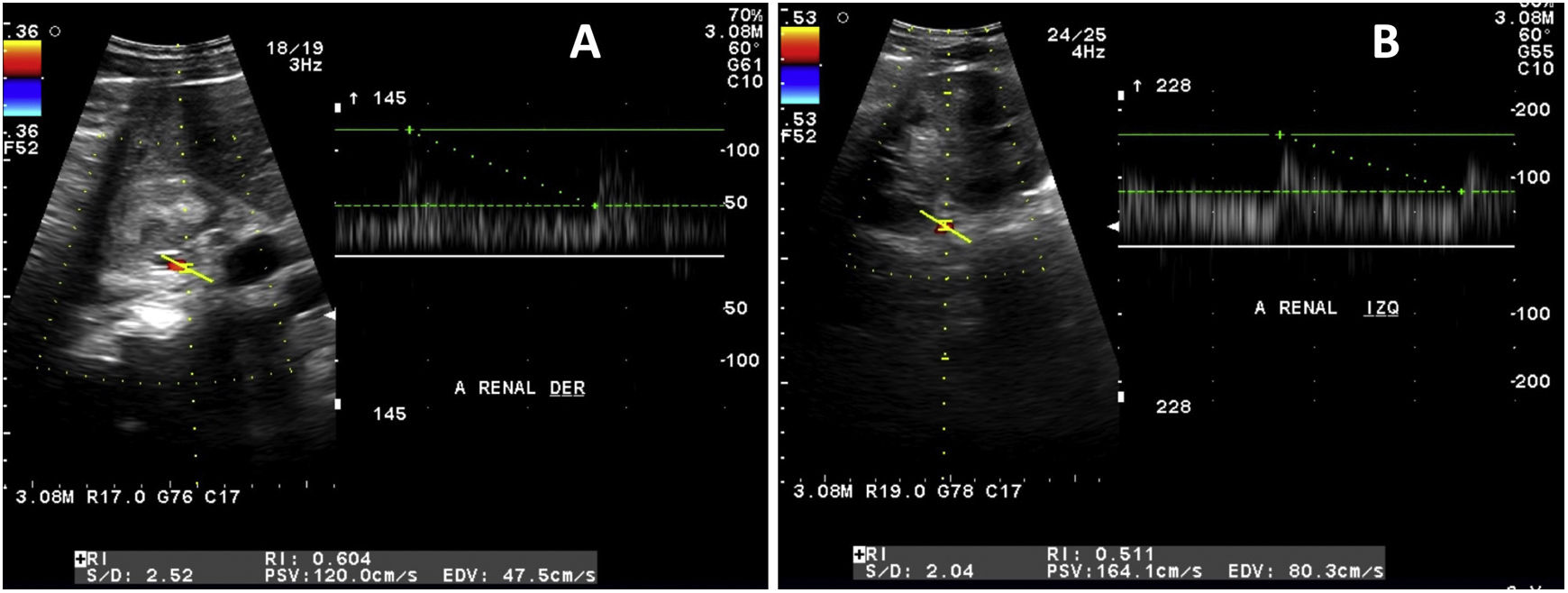
Given the suspicion of renovascular hypertension, a Doppler was practiced with the following findings (Fig. 2): maximum systolic velocity of 120cm/s in the right renal artery at the ostium and 120cm/s at the hilum, with a resistance index of 0.60. The left renal artery evidenced a maximum systolic velocity of 137cm/s at the ostium and 164cm/s at the hilum, with a resistance index of 0.51. These normal values do not support the diagnosis of renovascular hypertension; therefore, to completely rule out this possibility, a 99mTc-DMSA renal scintigram with captopril was performed, documenting baseline glomerular filtration rate in the left kidney of 149.3ml/min and the right kidney of 79.9ml/min; post-captopril: 232.6ml/min and 156.4ml/min, respectively.
Doppler ultrasound of renal arteries. A) Right: maximum systolic velocity of 120cm/s at the ostium level and 120cm/s at the hilum, with a resistance index of 0.60. B) Left: maximum systolic velocity of 137cm/s at the ostium and 164cm/s at the hilum, with a resistance index of 0.51.
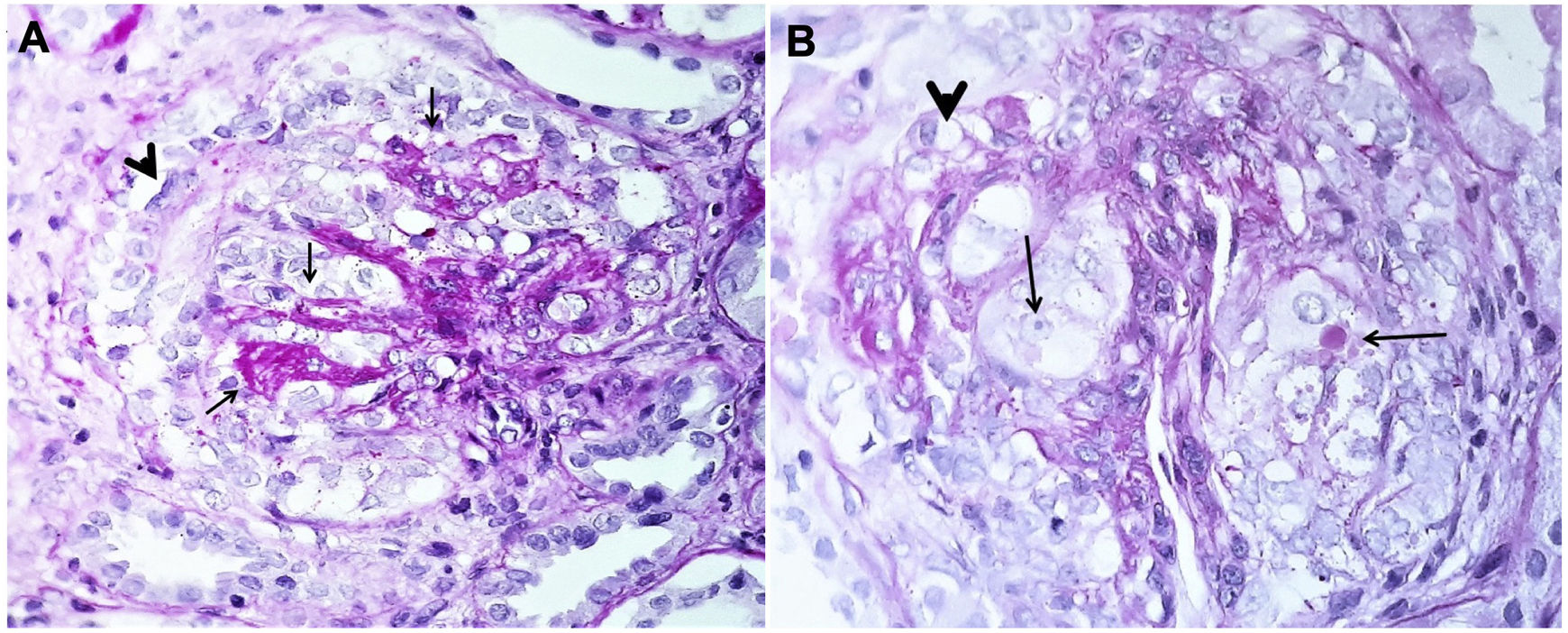
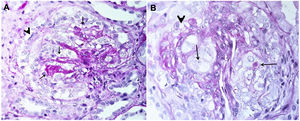
At follow-up, exclusive renal disease activity was found with normalization of acute-phase reactants, yet a progressive drop in glomerular filtration rate. At the fourth year of follow-up, creatinine increased up to 3.45mg/dl with a glomerular filtration rate of 34ml/min and persistence of hematuria and albuminuria of 1840mg in 24h. A nephritic syndrome was diagnosed, and the following studies were conducted: anti-neutrophil cytoplasm antibodies, complement profile, systemic lupus erythematosus, and viral panel, reported as normal. A renal biopsy was accomplished, demonstrating focal and segmental glomerulosclerosis with a collapsing variety (Fig. 3). High-dose glucocorticoid treatment was initiated (prednisone 50mg/day–1mg/kg/day–), switching methotrexate to azathioprine at 2mg/kg/day, with no response: nitrogen compounds were elevated, with a serum creatinine of 8.32mg/dl. Renal replacement therapy was started with hemodialysis. The patient is under follow-up with no data on extrarenal vasculitis activity.
DiscussionWe present the case of a patient with a 4-year TA whose early signs and symptoms were claudication of the lower extremities, present in 10–35%3 of the cases, and arterial hypertension, which is detected in up to 80% of patients in this age group. Endocrinopathies were ruled out due to the presence of abdominal murmur and pulse asymmetry. A computed tomography angiography was performed, revealing abdominal aorta stenosis, with involvement of the renal arteries at the ostium. The case was classified as AT based on the EULAR/PRINTO/PRES criteria, which include as a mandatory criterion angiographic abnormality of the aorta or its main branches and pulmonary arteries, together with at least one of the following conditions: (a) absence of pulses or claudication in the peripheral artery induced by physical activity; (b) difference of at least 10mmHg in systolic blood pressure in the extremities; (c) murmurs over large arteries; (d) hypertension; and (e) elevation of acute-phase reactants. Compliance with these criteria provides a sensitivity and specificity above 99%.5 The patient met all the above criteria. Differential diagnoses were also ruled out, such as fibromuscular dysplasia, present in young patients, which generally spares the aorta and affects the distal 2/3 of the renal arteries, with a characteristic tortuous morphology.6
Classification criteria for TA require evidence of angiographic abnormality, either by angiography, magnetic resonance angiography, or computed tomography angiography; the latter is a non-invasive method that offers excellent anatomical detail of both the lumen of the vessel and its wall. Along with magnetic resonance angiography, they have replaced angiography, historically considered the gold standard, for its invasive nature and the absence of information on the vessel wall.7 In this case, there was evidence of involvement limited to the abdominal aorta and renal arteries, classified as Numano IV, present in only 5.9% of patients diagnosed with TA.8
Doppler ultrasound is an inexpensive, non-invasive tool, without exposure to radiation or contrast media; it is an option when other procedures for diagnosis and monitoring of TA are not available. In this case, it was used to study renal artery stenosis. The best accepted criterion by different studies is a maximum systolic velocity above 180cm/s, with a sensitivity that can reach up to 90%.9 A 99mTc-DMSA renal scintigram was also performed with captopril, which showed an increase in post-drug glomerular filtration rate, being negative for renovascular hypertension. This latter study is recommended for patients with low pre-test probability, with a high negative predictive value; in some series, it is reported up to 100%.10 Based on these data, renovascular hypertension was ruled out.
Renal manifestations of TA are related to renovascular hypertension and rarely to disorders that affect the renal parenchyma, although some cases have been reported. In the reviewed literature, a single previous report was found associated with focal and segmental glomerulosclerosis in a 29-year-old female patient who presented TA with multifocal disease, without evidence of renal flow alterations, with probable immune-mediated etiology.4 In a single-center series in China, six cases were reported, all female, with a mean age of 35 years. The clinical presentation in 2 cases was hematuria (10–15 red blood cells per field), in 5 significant proteinuria, of which 2 were in nephrotic range and one with nephrotic syndrome. Renal manifestations occurred in a mean of 60.7 months after the diagnosis of TA, and in no case alterations in renal blood flow were found. Histopathological studies reported IgA nephropathy in 2 cases, proliferative mesangial glomerulonephritis, membranoproliferative glomerulonephritis, minimal-change disease, and fibrillary glomerulonephritis (one case each).11
The initial response to treatment, when only the diagnosis of TA was available, was favorable; however, during follow-up, with the appearance of focal segmental glomerulosclerosis, the patient had proteinuria close to the nephrotic range, in addition to elevated nitrogen compounds, and a rapid decline in glomerular filtration rate, all poor prognosis criteria and response to steroids.12 Consequently, it was decided to initiate azathioprine instead of methotrexate based on recommendations drawn from the few existing studies. This combination, as primary treatment, achieves remission rates of up to 80%,13 but due to the baseline clinical features aforementioned and the histological variety, his evolution was poor, ending up on renal replacement therapy.
ConclusionIn this case report, one patient diagnosed with TA underwent a renal biopsy due to nephritic syndrome, with proteinuria in a subnephrotic range, without an evident cause. Changes consistent with focal segmental glomerulosclerosis were found; this clinicopathological entity is characterized by nephrotic or subnephrotic proteinuria, which may appear as a primary disease or be associated with multiple causes, including familial/genetic, viruses (HIV and cytomegalovirus), drugs, and structural and functional adaptive responses (such as hyperfiltration processes in obese patients, solitary kidneys, or reflux nephropathy.14 The collapsing variety also includes other etiologies allied to ischemia or marked reduction in renal flow.14 All these causes were ruled out in the patient.
Ethical ConsiderationsThe work has been evaluated by the local committees of research, ethics in research and biosafety who have reviewed the content of the manuscript without exposing therein personal data of the patient object of the research.
FinancingThe authors declare that for the realization of this manuscript, they did not receive financial help from third parties, and everything was done with their resources.
Conflict of interestsThe authors declare the absence of a conflict of interest in the preparation of this manuscript.