Bertolotti's syndrome was first described in 1917. It is due to a congenital anatomical abnormality, and is defined by the presence of a transverse mega-apophysis, which entails an alteration in the lumbosacral transition. It can cause pain due to involvement of various structures: lumbosacral neo-articulation, contralateral facet arthrosis, sciatica, discogenic, or sacroiliac pain. It is characterized by low back pain, with a normal physical examination. According to some studies, the incidence is high (between 7% and 20%). Initial treatment should be conservative, while there are interventionist alternatives.
El síndrome de Bertolotti fue descrito en 1917. Se debe a una anormalidad anatómica congénita y se define por la presencia de una megaapófisis transversa, que conlleva una alteración en la transición lumbosacra. Puede generar dolor por afectación de diversas estructuras: neoarticulación lumbosacra, artrosis facetaria del lado contralateral, lumbociatalgia, dolor discogénico o dolor sacroilíaco. Se caracteriza por un dolor lumbar bajo, con una exploración física normal. Según algunos estudios la incidencia es elevada (entre 7 y 20%). El tratamiento inicial debe ser conservador, si bien existen alternativas intervencionistas.
A 56-year-old woman without known drug allergies, with a history of arterial hypertension, dyslipidemia and polyarthrosis. Her usual treatment was with omeprazole, acetylsalicylic acid, beta-blocker and thiazide. She consulted us for low back pain of mechanical characteristics of long evolution. Such lumbago increases with the trunk flexion and occasionally radiates to the right lower limb until the knee. The rest of the exploration is normal. Under treatment with NSAIDs, tramadol and diazepam, without improvement.
The simple X-ray of the spine (Fig. 1) shows an alteration in the lumbosacral transitional vertebra with a sacral lumbarization and increase in both transverse processes of L5, more pronounced in the right side.
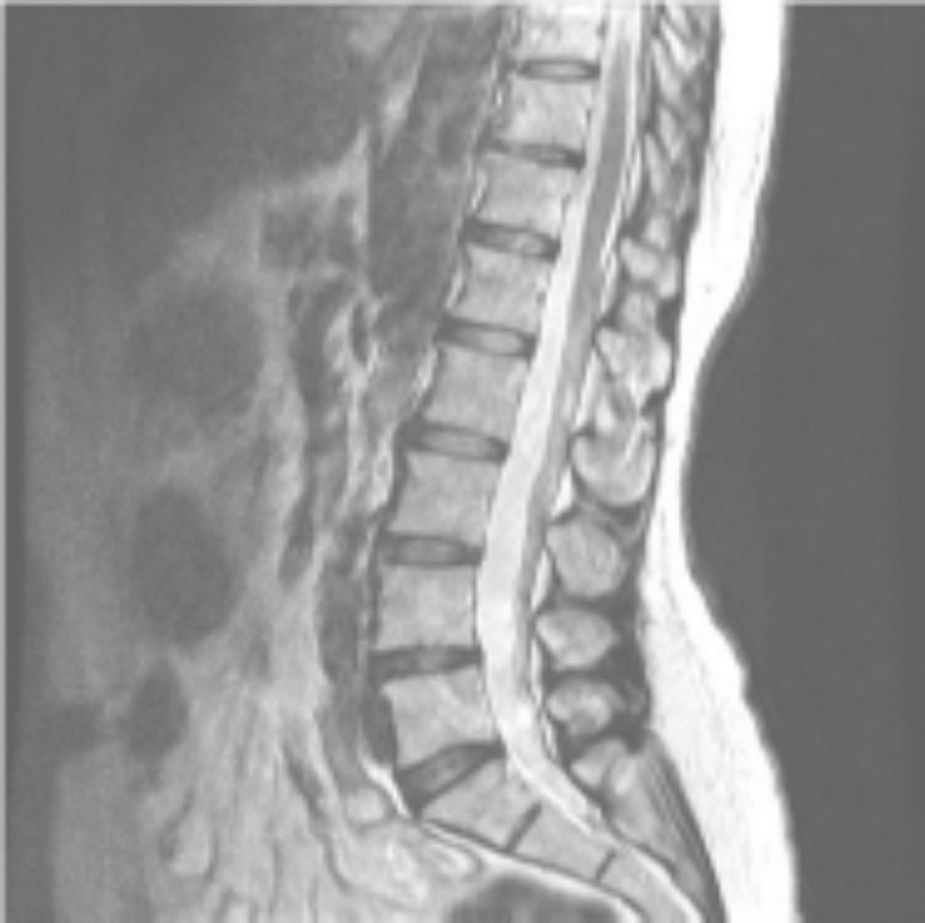
The nuclear magnetic resonance (Fig. 2) reveals some degree of disk dehydration, with moderate diffuse bulging of the annulus fibrosus of the intervertebral discs L4-L5 and L5-S1, with a small posterior annular tear at the L5-S1 level. It also shows interapophyseal degenerative phenomena that cause decrease of the caliber of foramina at the L4-L5 and L5-S1 levels, of greater connotation at the right L4-L5 level.
The nuclear magnetic resonance reveals some degree of disk dehydrations with moderate diffuse bulgings of annulus fibrosus of intervertebral discs L4-L5 and L5-S1 with a small posterior annular tear at the level of L5-S1. It also shows interapophysial degenerative phenomena that cause decrease in the caliber of foramina at L4-L5 and L5-S1 levels, of greater connotation at the right L4-L5 level.
With a diagnosis of alteration of the lumbosacral transitional vertebra or Bertolotti syndrome, we intensified the analgesic treatment along with rehabilitation, but given the poor response, she was referred to the unit of pain management of our hospital, where a block of the medial branch of the dorsal branch of the spinal nerve (facet block) at the L3-4, L4-L5 and L5-S1 levels was carried out, with local anesthetic and corticoid, with a positive but transient outcome. This block served for the localization of the structure that caused the low back pain. For this reason it was decided, subsequently, to perform a conventional radiofrequency (rhizolysis) of the medial branches, of the dorsal branches of the spinal nerves, at the L3-L4, L4-L5 and L5-S1 levels, in the right side. This radiofrequency, by using temperatures of 80 degrees, is ablative because it denervates the innervated joints. In this case the neo-articulation formed between the transverse mega-apophysis of L5 and the iliac blade, receives the innervation from these branches, and therefore, its denervation can produce relief of the low back pain, if this is the cause of this pain. In this patient there was a significant pain relief after performing the rhizolysis.
DiscussionBertolotti syndrome was described in 1917 by Mario Bertolotti, as already mentioned.1 It is a congenital anatomical abnormality, present, according to the literature, in 7–20% of the population.2 It is defined by the presence of a transverse mega-apophysis that articulates with the sacrum or the ilium, which leads to an alteration in the lumbosacral transition, and therefore, to a change in the biomechanics of the axial skeleton.
This alteration can be bilateral or unilateral,3 producing a low back pain clinic usually after the second decade of life.2 Most patients are asymptomatic,4 although when it is assymetric5 it can generate pain, originated in different structures: a neo-articulation in the affected side, arthrosis in the posterior interapophyseal joints, facet arthrosis in the contralateral side, pain in the sacroiliac joint, and even discogenic pain and lumboscyatic pain.
It is characterized by low back pain, because there is an abnormal mechanical tension which leads to an affectation of the facet joint, overstrain of the psoas and quadrate lumborum muscles, a compression of the nerve root due to the narrowing of the intervertebral foramina and the increased prevalence of protrusion or extrusion of the disk above the transitional vertebra L5. This would explain the lumbosciatic pain experienced by some of these patients. We should not forget that in almost 30% of patients who have undergone a surgery of herniated disc6 there is an alteration of the lumbosacral transition.
For its diagnosis we should be based on the clinic of low back pain and the radiological findings (lumbosacral radiograph, nuclear magnetic resonance, CT scan).
The lumbosacral transitional vertebra, anatomically defined as a vertebra that shares similar characteristics with both the upper and lower vertebral segments,2 has been classified into 4 types according to the method of Castellvi7:
- -
Type I: dysplastic transverse process.
- -
Type II: lumbarization/sacralization with enlargement of the transverse process which forms a diarthrosis with the sacrum.
- -
Type III: fusion of the transverse process with the sacrum.
- -
Type IV: mixed (it includes a unilateral type II with a type III in the contralateral side).
Each type is subdivided into a or b, according to whether they are unilateral or bilateral, respectively.
The initial treatment should be conservative (NSAIDs – muscle relaxants and rehabilitation),8 while there are interventionist alternatives3,9 such as infiltration of the lumbosacral neo-articulation9 with local anesthetics or steroids, the infiltration of facet joints and the radiofrequency sensitive ablation, also called rhizolysis, and even a more aggressive intervention such as the resection of the transverse mega-apophysis,10 with controversial outcomes.8
The block at the level of the nerves that supply the joint (facet or lumbosacral neo-articulation) is temporarily effective and it help us to identify the origin of the pain. In the case that we present, it was carried out a block with anesthetic and corticoid in the facet joints at different levels and, given the positive response, it was decided the radiofrequency ablation (rhizolysis) of the sensory branches which are responsible for the facet innervation and hypothetically for the neo-articulation formed between the mega-transverse and the iliac blade.
This interventional technique seeks the percutaneous radiofrequency lumbar facet denervation.11,12 It is based on the application of an electrode in the proximity of the posterior branch of the spinal nerve in its emergence between the facet and the transverse process, with the aid of fluoroscopy by AP or lateral projection, to verify the exact location of the electrode, which transmits heat generated by radiofrequency, causing damage in a controlled manner, which produces the cessation of the transmission of the pain originated in its innervation territory.11 A sensorimotor stimulation should be conducted before producing the lesion, in order to check the proper placement of the electrode and, therefore, it should be verified that the motor stimulation does not generate a muscle contraction in the territory of the stimulated root, thus ensuring there is no damage to the anterior branch of the spinal nerve.
ConclusionBertolotti syndrome has a high incidence and occurs in a high percentage in young people. The treatment should be initially conservative. However, in refractory cases and with an intense level of pain, interventional treatment can be an alternative in these patients.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors declare that they have no conflict of interest.
Please cite this article as: Moreno García MS, del Río-Martínez PS, Baltanás Rubio P, Cía Blasco P. Síndrome de Bertolotti: a propósito de un caso. Rev Colomb Reumatol. 2016;23:200–203.