Primary angiitis of the central nervous system (PACNS) is a rare autoimmune disease characterized by the inflammation of central nervous system arteries without compromising any other organ, and without a primary cause. This disease predominantly affects medium to small caliber arteries in the brain parenchyma, the spinal cord and the meninges, causing central nervous system (CNS) dysfunction.1 With an incidence rate of 2.4 cases per 1,000,000 habitants, it is a truly rare entity. Its pathophysiology is not yet elucidated, but it appears to be mediated by antigen presentation to the T lymphocytes in the arterial wall.2
PACNS is categorized into different subtypes according to pathological and histological findings: granulomatous angiitis of the central nervous system (GACNS), lymphocytic angiitis of the CNS, amyloid beta-related angiitis, mass-like lesions, and spinal cord vasculitis. With 59% of cases, GACNS is the most common of the subtypes.3
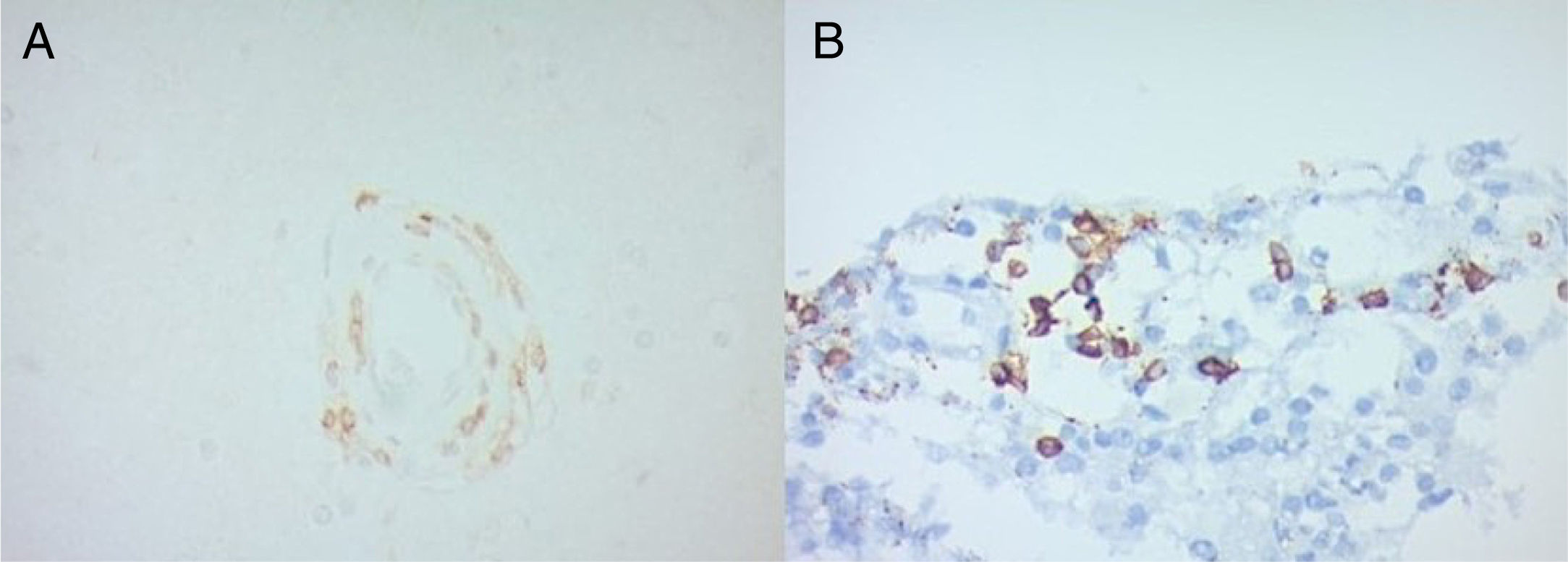
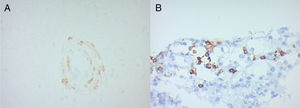
In 2013 our group reported 3 cases of patients with PACNS.4 This time, an immunohistochemical study was done in 2 of the patients’ samples, revealing a leukocytic infiltratate (CD45+) constituted almost entirely of T lymphocytes (CD3+) with a clearly higher prevalence of CD4+ cells (Fig. 1A), with no evidence of plasmatic cells (CD138 and CD38 markers were negative) and an absence of Treg Lymphocytes (negativity for CD25). HLA was detected in 50% of the cells in both samples (Fig. 1B).
In a report of 4 biopsies of Japanese patients, there was a T lymphocyte infiltrate, with a predominance of CD8+ cells in the brain parenchyma, and a B lymphocyte (CD20+) prevalence in the perivascular area.5 In another Japanese case report,6 the biopsy analysis showed an infiltrate of memory T cells (CD45RO+), suggesting that an activation by cytokines such as IFN-γ leads to an enhanced antigen presentation by perivascular macrophages, endothelial cells, smooth muscle cells, and astrocytes. These data, along with our results, suggests a T lymphocyte (with CD4 predominance), Th1 response (with IFN-γ and IL-12 cytokines) mediated disease. The negligible presence of B lymphocytes and the absence of plasmatic cells imply that this is not a humoral immunity mediated entity.
Nevertheless, more complex studies are required to understand the pathophysiology of this disease, the cytokine expression pattern, and to be able to establish a difference between the leukocyte infiltrate of the brain parenchyma and the perivascular space. In the future, this information could lead to targeted therapy against T lymphocyte co-stimulation.
Conflict of interestThe authors declare they have no conflicts of interest. No financial support was received.
The patients authorized the publication of this article and signed informed consent.